Shoulder Dystocia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Refusal to Undergo a Cesarean Section: a Woman's Right Or a Criminal Act ? Monica K
Health Matrix: The Journal of Law- Medicine Volume 15 | Issue 2 2005 Refusal to Undergo a Cesarean Section: A Woman's Right or a Criminal Act ? Monica K. Miller Follow this and additional works at: https://scholarlycommons.law.case.edu/healthmatrix Part of the Health Law and Policy Commons Recommended Citation Monica K. Miller, Refusal to Undergo a Cesarean Section: A Woman's Right or a Criminal Act ?, 15 Health Matrix 383 (2005) Available at: https://scholarlycommons.law.case.edu/healthmatrix/vol15/iss2/6 This Article is brought to you for free and open access by the Student Journals at Case Western Reserve University School of Law Scholarly Commons. It has been accepted for inclusion in Health Matrix: The ourJ nal of Law-Medicine by an authorized administrator of Case Western Reserve University School of Law Scholarly Commons. REFUSAL TO UNDERGO A CESAREAN SECTION: A WOMAN'S RIGHT OR A CRIMINAL ACT? Monica K. Millert INTRODUCTION In March, 2004, Melissa Ann Rowland, a twenty-eight-year-old woman from Salt Lake City, gained national media attention when she was arrested on charges of homicide relating to the death of her son. Although there are many child homicide cases that occur regularly across the country that do not attract wide-spread media attention, this case was exceptional because her son died before he was ever born. 1 Rowland had sought medical treatment several times between late December 2003 and January 9, 2004. Each time, she was allegedly advised to get immediate medical treatment, including a cesarean sec- tion (c-section), because her twin fetuses were in danger of death or serious injury. -
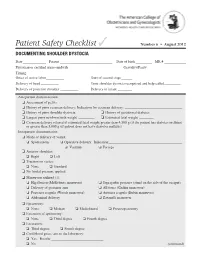
Documenting Shoulder Dystocia
Patient Safety Checklist ✓ Number 6 • August 2012 DOCUMENTING SHOULDER DYSTOCIA Date _____________ Patient _____________________________ Date of birth _________ MR # ____________ Physician or certified nurse–midwife _____________________________ Gravidity/Parity______________________ Timing: Onset of active labor __________ Start of second stage ______ Delivery of head __________ Time shoulder dystocia recognized and help called _________ Delivery of posterior shoulder __________ Delivery of infant ________ Antepartum documentation: ❏ Assessment of pelvis ❏ History of prior cesarean delivery: Indication for cesarean delivery: ________________________________ ❏ History of prior shoulder dystocia ❏ History of gestational diabetes ❏ Largest prior newborn birth weight _________ ❏ Estimated fetal weight ________ ❏ Cesarean delivery offered if estimated fetal weight greater than 4,500 g (if the patient has diabetes mellitus) or greater than 5,000 g (if patient does not have diabetes mellitus) Intrapartum documentation: ❏ Mode of delivery of vertex: ❏ Spontaneous ❏ Operative delivery: Indication: _________________________________________ ❏ Vacuum ❏ Forceps ❏ Anterior shoulder: ❏ Right ❏ Left ❏ Traction on vertex: ❏ None ❏ Standard ❏ No fundal pressure applied ❏ Maneuvers utilized (1): ❏ Hip flexion (McRoberts maneuver) ❏ Suprapubic pressure (stand on the side of the occiput) ❏ Delivery of posterior arm ❏ All fours (Gaskin maneuver) ❏ Posterior scapula (Woods maneuver) ❏ Anterior scapula (Rubin maneuver) ❏ Abdominal delivery ❏ Zavanelli maneuver -

Caesarean Section Or Vaginal Delivery in the 21St Century
CAESAREAN SECTION OR VAGINAL DELIVERY IN THE 21ST CENTURY ntil the 20th Century, caesarean fluid embolism. The absolute risk of trans-placentally to the foetus, prepar- section (C/S) was a feared op- death with C/S in high and middle- ing the foetus to adopt its mother’s Ueration. The ubiquitous classical resource settings is between 1/2000 and microbiome. C/S interferes with neonatal uterine incision meant high maternal 1/4000 (2, 3). In subsequent pregnancies, exposure to maternal vaginal and skin mortality from bleeding and future the risk of placenta previa, placenta flora, leading to colonization with other uterine rupture. Even with aseptic surgi- accreta and uterine rupture is increased. environmental microbes and an altered cal technique, sepsis was common and These conditions increase maternal microbiome. Routine antibiotic exposure lethal without antibiotics. The operation mortality and severe maternal morbid- with C/S likely alters this further. was used almost solely to save the life of ity cumulatively with each subsequent Microbial exposure and the stress of a mother in whom vaginal delivery was C/S. This is of particular importance to labour also lead to marked activation extremely dangerous, such as one with women having large families. of immune system markers in the cord placenta previa. Foetal death and the use blood of neonates born vaginally or by of intrauterine foetal destructive proce- Maternal Benefits C/S after labour. These changes are absent dures, which carry their own morbidity, C/S has a modest protective effect against in the cord blood of neonates born by were often preferable to C/S. -

1063 Relation Between Vaginal Hiatus and Perineal Body
1063 Campanholi V1, Sanches M1, Zanetti M R D1, Alexandre S1, Resende A P M1, Petricelli C D1, Nakamura M U1 1. Unifesp- Brasil RELATION BETWEEN VAGINAL HIATUS AND PERINEAL BODY LENGTHS WITH EPISIOTOMY IN VAGINAL DELIVERY Hypothesis / aims of study The aim of the study was to assess the relationship between vaginal hiatus and perineal body lengths with the occurrence of episiotomy during vaginal delivery. Study design, materials and methods It´s a cross-sectional observational study with a consecutive sample of 60 parturients, made from July 2009 to March 2010 in the Obstetric Center at University Hospital in São Paulo, Brazil. Inclusion criteria were parturients at term (37 to 42 weeks gestation) in the first stage of labour, with less than 9 cm dilatation, with a single fetus in cephalic presentation and good vitality confirmed by cardiotocography. Exclusion criteria were parturients submitted to cesarean section or forceps delivery. The patients were evaluated in the lithotomic position. The measurement was performed in the first stage of labour, by the same examiner using a metric measuring tape previously cleaned with alcohol 70% and discarded after each use. The vaginal hiatus length (distance between the external urethral meatus and the vulvar fourchette) and the perineal body (distance between the vulvar fourchette and the center of the anal orifice) were evaluated. For statistical analysis the SPSS (Statistical Package for Social Sciences) version 17® was used, applying Mann-Whitney Test and Spearman Rank Correlation Test to determine the importance of vaginal hiatus and perineal body length in the occurrence of episiotomy, with p<0.05. -

Clinical Policy: Fetal Surgery in Utero for Prenatally Diagnosed
Clinical Policy: Fetal Surgery in Utero for Prenatally Diagnosed Malformations Reference Number: CP.MP.129 Effective Date: 01/18 Coding Implications Last Review Date: 09/18 Revision Log Description This policy describes the medical necessity requirements for performing fetal surgery. This becomes an option when it is predicted that the fetus will not live long enough to survive delivery or after birth. Therefore, surgical intervention during pregnancy on the fetus is meant to correct problems that would be too advanced to correct after birth. Policy/Criteria I. It is the policy of Pennsylvania Health and Wellness® (PHW) that in-utero fetal surgery (IUFS) is medically necessary for any of the following: A. Sacrococcygeal teratoma (SCT) associated with fetal hydrops related to high output heart failure : SCT resecton: B. Lower urinary tract obstruction without multiple fetal abnormalities or chromosomal abnormalities: urinary decompression via vesico-amniotic shunting C. Ccongenital pulmonary airway malformation (CPAM) and extralobar bronchopulmonary sequestration with hydrops (hydrops fetalis): resection of malformed pulmonary tissue, or placement of a thoraco-amniotic shunt; D. Twin-twin transfusion syndrome (TTTS): treatment approach is dependent on Quintero stage, maternal signs and symptoms, gestational age and the availability of requisite technical expertise and include either: 1. Amnioreduction; or 2. Fetoscopic laser ablation, with or without amnioreduction when member is between 16 and 26 weeks gestation; E. Twin-reversed-arterial-perfusion (TRAP): ablation of anastomotic vessels of the acardiac twin (laser, radiofrequency ablation); F. Myelomeningocele repair when all of the following criteria are met: 1. Singleton pregnancy; 2. Upper boundary of myelomeningocele located between T1 and S1; 3. -

Fetal Surgery in Utero for Prenatally Diagnosed Malformations
Clinical Policy: Fetal Surgery in Utero for Prenatally Diagnosed Malformations Reference Number: PA.CP.MP.129 Effective Date: 01/18 Coding Implications Last Review Date: 12/18 Revision Log Description This policy describes the medical necessity requirements for performing fetal surgery. This becomes an option when it is predicted that the fetus will not live long enough to survive delivery or after birth. Therefore, surgical intervention during pregnancy on the fetus is meant to correct problems that would be too advanced to correct after birth. Policy/Criteria I. It is the policy of Pennsylvania Health and Wellness® (PHW) that in-utero fetal surgery (IUFS) is medically necessary for any of the following: A. Sacrococcygeal teratoma (SCT) associated with fetal hydrops related to high output heart failure : SCT resection; B. Lower urinary tract obstruction without multiple fetal abnormalities or chromosomal abnormalities: urinary decompression via vesico-amniotic shunting C. Congenital pulmonary airway malformation (CPAM) and extralobar bronchopulmonary sequestration with hydrops (hydrops fetalis): resection of malformed pulmonary tissue, or placement of a thoraco-amniotic shunt; D. Twin-twin transfusion syndrome (TTTS): treatment approach is dependent on Quintero stage, maternal signs and symptoms, gestational age and the availability of requisite technical expertise and include either: 1. Amnioreduction; or 2. Fetoscopic laser ablation, with or without amnioreduction when member is between 16 and 26 weeks gestation; E. Twin-reversed-arterial-perfusion (TRAP): ablation of anastomotic vessels of the acardiac twin (laser, radiofrequency ablation); F. Myelomeningocele repair when all of the following criteria are met: 1. Singleton pregnancy; 2. Upper boundary of myelomeningocele located between T1 and S1; 3. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

THE PRACTICE of EPISIOTOMY: a QUALITATIVE DESCRIPTIVE STUDY on PERCEPTIONS of a GROUP of WOMEN Online Brazilian Journal of Nursing, Vol
Online Brazilian Journal of Nursing E-ISSN: 1676-4285 [email protected] Universidade Federal Fluminense Brasil Yi Wey, Chang; Rejane Salim, Natália; Pires de Oliveira Santos Junior, Hudson; Gualda, Dulce Maria Rosa THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Online Brazilian Journal of Nursing, vol. 10, núm. 2, abril-agosto, 2011, pp. 1-11 Universidade Federal Fluminense Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=361441674008 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Chang Yi Wey1, Natália Rejane Salim2, Hudson Pires de Oliveira Santos Junior3, Dulce Maria Rosa Gualda4 1. Hospital Universitário, Universidade de São Paulo 2,3,4. Escola de Enfermagem, Universidade de São Paulo ABSTRACT: This study set out to understand the experiences and perceptions of women from the practices of episiotomy during labor. This is a qualitative descriptive approach, performed in a school hospital in São Paulo, which data were collected through interviews with the participation of 35 women, who experienced and not episiotomy in labor. The thematic analysis shows these categories: Depends the size of the baby facilitates the childbirth; Depends each woman; The woman is not open; and Episiotomy is not necessary. The results allowed that there is lack of clarification and knowledge regarding this practice, which makes the role of decision ends up in the professionals’ hands. -

Journal of Surgery and Trauma
In the name of GOD Journal of Birjand University of Medical Surgery and trauma Sciences & Health Services 2345-4873ISSN 2015; Vol. 3; Supplement Issue 2 Publisher: Deputy Editor: Birjand University of Medical Sciences & Health Seyyed Amir Vejdan, Assistant Professor of General Services Surgery, Birjand University of Medical Sciences Director-in-Charge: Managing Editor: Ahmad Amouzeshi, Assistant Professor of General Zahra Amouzeshi, Instructor of Nursing, Birjand Surgery, Birjand University of Medical Sciences University of Medical Sciences Editor-in-Chief: Journal Expert: Mehran Hiradfar, Associate professor of pediatric Fahime Arabi Ayask, B.Sc. surgeon, Mashhad University of Medical Sciences Editorial Board Ahmad Amouzeshi: Assistant Professor of General Surgery, Birjand University of Medical Sciences, Birjand, Iran; Masoud Pezeshki Rad: Assistant professor Department of Radiology, Mashhad university of Medical Sciences, Mashhad, Iran; Ali Taghizadeh kermani: Assistant professor Department of Radiology, Mashhad university of Medical Sciences, Mashhad, Iran; Ali Jangjo: Assistant Professor of General Surgery, Mashhad University of Medical Sciences, Mashhad, Iran; Sayyed-zia-allah Haghi: Professor of Thoracic-Surgery, Mashhad University of Medical Sciences, Mashhad, Iran; Ramin Sadeghi: Assistant professor Department of Radiology, Mashhad University of Medical Sciences, Mashhad, Iran; Mohsen Aliakbarian: Assistant Professor of General Surgery, Mashhad University of Medical Sciences, Mashhad, Iran; Mohammad Ghaemi: Assistant Professor -

Gtg-No-20B-Breech-Presentation.Pdf
Guideline No. 20b December 2006 THE MANAGEMENT OF BREECH PRESENTATION This is the third edition of the guideline originally published in 1999 and revised in 2001 under the same title. 1. Purpose and scope The aim of this guideline is to provide up-to-date information on methods of delivery for women with breech presentation. The scope is confined to decision making regarding the route of delivery and choice of various techniques used during delivery. It does not include antenatal or postnatal care. External cephalic version is the topic of a separate RCOG Green-top Guideline No. 20a: ECV and Reducing the Incidence of Breech Presentation. 2. Background The incidence of breech presentation decreases from about 20% at 28 weeks of gestation to 3–4% at term, as most babies turn spontaneously to the cephalic presentation. This appears to be an active process whereby a normally formed and active baby adopts the position of ‘best fit’ in a normal intrauterine space. Persistent breech presentation may be associated with abnormalities of the baby, the amniotic fluid volume, the placental localisation or the uterus. It may be due to an otherwise insignificant factor such as cornual placental position or it may apparently be due to chance. There is higher perinatal mortality and morbidity with breech than cephalic presentation, due principally to prematurity, congenital malformations and birth asphyxia or trauma.1,2 Caesarean section for breech presentation has been suggested as a way of reducing the associated perinatal problems2,3 and in many countries in Northern Europe and North America caesarean section has become the normal mode of breech delivery. -

Leapfrog Hospital Survey Hard Copy
Leapfrog Hospital Survey Hard Copy QUESTIONS & REPORTING PERIODS ENDNOTES MEASURE SPECIFICATIONS FAQS Table of Contents Welcome to the 2016 Leapfrog Hospital Survey........................................................................................... 6 Important Notes about the 2016 Survey ............................................................................................ 6 Overview of the 2016 Leapfrog Hospital Survey ................................................................................ 7 Pre-Submission Checklist .................................................................................................................. 9 Instructions for Submitting a Leapfrog Hospital Survey ................................................................... 10 Helpful Tips for Verifying Submission ......................................................................................... 11 Tips for updating or correcting a previously submitted Leapfrog Hospital Survey ...................... 11 Deadlines ......................................................................................................................................... 13 Deadlines for the 2016 Leapfrog Hospital Survey ...................................................................... 13 Deadlines Related to the Hospital Safety Score ......................................................................... 13 Technical Assistance....................................................................................................................... -

Mid-Trimester Preterm Premature Rupture of Membranes (PPROM): Etiology, Diagnosis, Classification, International Recommendations of Treatment Options and Outcome
J. Perinat. Med. 2018; 46(5): 465–488 Review article Open Access Michael Tchirikov*, Natalia Schlabritz-Loutsevitch, James Maher, Jörg Buchmann, Yuri Naberezhnev, Andreas S. Winarno and Gregor Seliger Mid-trimester preterm premature rupture of membranes (PPROM): etiology, diagnosis, classification, international recommendations of treatment options and outcome DOI 10.1515/jpm-2017-0027 neonates delivered without antecedent PPROM. The “high Received January 23, 2017. Accepted May 19, 2017. Previously pub- PPROM” syndrome is defined as a defect of the chorio- lished online July 15, 2017. amniotic membranes, which is not located over the inter- nal cervical os. It may be associated with either a normal Abstract: Mid-trimester preterm premature rupture of mem- or reduced amount of amniotic fluid. It may explain why branes (PPROM), defined as rupture of fetal membranes sensitive biochemical tests such as the Amniosure (PAMG-1) prior to 28 weeks of gestation, complicates approximately or IGFBP-1/alpha fetoprotein test can have a positive result 0.4%–0.7% of all pregnancies. This condition is associ- without other signs of overt ROM such as fluid leakage with ated with a very high neonatal mortality rate as well as an Valsalva. The membrane defect following fetoscopy also increased risk of long- and short-term severe neonatal mor- fulfils the criteria for “high PPROM” syndrome. In some bidity. The causes of the mid-trimester PPROM are multi- cases, the rupture of only one membrane – either the cho- factorial. Altered membrane morphology including marked rionic or amniotic membrane, resulting in “pre-PPROM” swelling and disruption of the collagen network which is could precede “classic PPROM” or “high PPROM”.