Aortitis: Radiological Findings in Relation to Its Various Etiologies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Known Infectious Causes of Vasculitis in Man
PATHOGENESIS Known infectious causes of vasculitis in man STANLEY J. NAIDES, MD n array of pathogens is known to cause vasculi- and our ability to intervene in disease processes, have ren- tis in man.1,2 For several of these agents, vas- dered some causes of vasculitis far less common. culitis is the major manifestation of disease. The Amajority, however, typically present as infec- ■ VIRAL CAUSES OF VASCULITIS tious processes in which vasculitis is an occasional mani- Our knowledge of viral pathogenesis has exploded in the festation of disease. For many, vasculitis may be a compo- last quarter of the twentieth century, accelerated in large nent of disease pathogenesis but is not a prominent feature part by epidemics of “emerging” viral diseases. Hepatitis C of the clinical presentation. The various agents—viruses, virus, discovered in 1989, has worldwide prevalence.3 The bacteria, and fungi—share a common target, blood vessels. 10- to 20-year latent period before hepatic or rheumatic The involvement of vessels may be direct, with vascular manifestations of disease explains the increasing number structures serving as targets. Many infectious pathogens of cases of hepatitis C virus–mediated vasculitis currently have tissue tropism that includes endothelium. Other being seen in the United States following the epidemic of agents may bind to the vessel wall because the vascular en- new infections in the 1980s.4 Prior to the discovery and dothelium expresses specific receptors for the pathogen or characterization of hepatitis C virus in the late 1980s, the another moiety with which the pathogen travels. Even triad of arthritis, palpable purpura, and type II cryoglobu- when the agent does not enter the endothelial cell, the im- linemia was given the sobriquet “essential mixed cryo- mune response to the agent may be focused at the vessel globulinemia” and considered an idiopathic vasculitis. -

Identification of Microorganisms Using Nucleic Acid Probes
Identification of Microorganisms Using Page 1 of 45 Nucleic Acid Probes Medical Policy An Independent Licensee of the Blue Cross and Blue Shield Association Title: Identification of Microorganisms Using Nucleic Acid Probes See Also: Influenza Virus Diagnostic Testing and Treatment in the Outpatient Setting Professional Institutional Original Effective Date: July 8, 2008 Original Effective Date: July 16, 2009 Revision Date(s): June 16, 2009; Revision Date(s): March 1, 2012; March 1, 2012; June 5, 2012; June 5, 2012; November 19, 2012; November 19, 2012; January 15, 2013; January 15, 2013; November 12, 2013 November 12, 2013 Current Effective Date: November 12, 2013 Current Effective Date: November 12, 2013 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. -

Syphilis As Seen by a Hospital Physician
284 Prof. Monro?Syphilis as seen by a Hospital Physician. SYPHILIS AS SEEN BY A HOSPITAL PHYSICIAN* By T. K. MONRO, M.A., M.D., Professor of Medicine, University of Glasgow. \ " / Mr. President and Gentlemen,?I thank you heartily for the honour you have done me in inviting me to be Honorary President of this Faculty for the session which is now opening. I was duly informed by Dr. Wardlaw that my principal duty as incumbent of this honourable office was to deliver an address to the Faculty, and as his invitation reached me while I was on holiday, with other objects in view, I had time to contemplate the responsibility I had undertaken, and to consider how I was to face it. In getting over the usual initial difficulty as to the choice of a subject, some assistance was afforded me by the President's instruction that the address ought to be one for the general practitioner. Quite a number of subjects would be appropriate from this point of view. I should have been glad to say some- thing on oral sepsis, a condition often spoken of, and no doubt often wrongly blamed, but also apt to be overlooked. Dentists do not always realise how completely one may be misled by the absence of subjective and objective evidence; so that even an experienced man may pass as innocuous a tooth which subse- quent extraction shows to have disease at its root. Medical men sometimes make a mistake in the opposite direction, by insisting, without sufficient justification, on the removal of teeth, e.g., in epileptiform neuralgia. -

A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification
Hindawi International Journal of Rheumatology Volume 2020, Article ID 8392542, 11 pages https://doi.org/10.1155/2020/8392542 Review Article A Review of Primary Vasculitis Mimickers Based on the Chapel Hill Consensus Classification Farah Zarka ,1 Charles Veillette ,1 and Jean-Paul Makhzoum 2 1Hôpital du Sacré-Cœur de Montreal, University of Montreal, Canada 2Vasculitis Clinic, Department of Internal Medicine, Hôpital du Sacré-Coeur de Montreal, University of Montreal, Canada Correspondence should be addressed to Jean-Paul Makhzoum; [email protected] Received 10 July 2019; Accepted 7 January 2020; Published 18 February 2020 Academic Editor: Charles J. Malemud Copyright © 2020 Farah Zarka et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Primary systemic vasculitides are rare diseases that may manifest similarly to more commonly encountered conditions. Depending on the size of the vessel affected (large vessel, medium vessel, or small vessel), different vasculitis mimics must be considered. Establishing the right diagnosis of a vasculitis mimic will prevent unnecessary immunosuppressive therapy. 1. Introduction 2. Large-Vessel Vasculitis Mimics Vasculitides are rare heterogenous diseases that affect vessel Large-vessel vasculitis (LVV) is an inflammatory vascu- walls as the main site of inflammation. Organs affected vary lopathy affecting large arteries; giant cell arteritis (GCA) depending on the type and size of blood vessels involved and Takayasu’s arteritis (TAK) are the two main docu- [1]. Autoimmune vasculitis can be primary (idiopathic) or mented variants, each with their own characteristic fea- secondary to an underlying disease. -
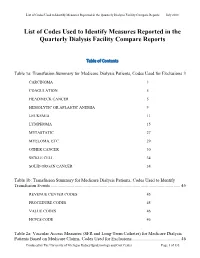
List of Codes Used to Identify Measures Reported in the QDFC
List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports Table of Contents Table 1a: Transfusion Summary for Medicare Dialysis Patients, Codes Used for Exclusions 3 CARCINOMA 3 COAGULATION 5 HEAD/NECK CANCER 5 HEMOLYTIC OR APLASTIC ANEMIA 9 LEUKEMIA 11 LYMPHOMA 15 METASTATIC 27 MYELOMA, ETC. 29 OTHER CANCER 30 SICKLE CELL 34 SOLID ORGAN CANCER 34 Table 1b: Transfusion Summary for Medicare Dialysis Patients, Codes Used to Identify Transfusion Events .................................................................................................................. 45 REVENUE CENTER CODES 45 PROCEDURE CODES 45 VALUE CODES 46 HCPCS CODE 46 Table 2a: Vascular Access Measures (SFR and Long-Term Catheter) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Exclusions ........................................... 46 Produced by The University of Michigan Kidney Epidemiology and Cost Center Page 1 of 135 List of Codes Used to Identify Measures Reported in the Quarterly Dialysis Facility Compare Reports July 2018 COMA 46 END STAGE LIVER DISEASE 48 METASTATIC CANCER 48 Table 2b: Standardized Fistulae Rate (SFR) for Medicare Dialysis Patients Based on Medicare Claims, Codes Used for Prevalent Comorbidities Adjusted in Model .................................... 50 ANEMIA 50 CORONARY ARTERY DISEASE 52 CONGESTIVE HEART FAILURE 55 CEREBROVASCULAR DISEASE 56 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 68 DIABETES 69 DRUG DEPENDENCE 79 INFECTIONS (NON-VASCULAR ACCESS-RELATED): 93 PERIPHERAL VASCULAR DISEASE (INCLUDES ARTERIAL, VENOUS AND NONSPECIFIC DISEASES) 124 Table 3: Dialysis Adequacy ................................................................................................... -

Circulating the Facts About Peripheral Vascular Disease
Abdominal Arterial Disease Circulating the Facts About Peripheral Vascular Disease Brought to you by the Education Committee of the Society for Vascular Nursing 1 www.svnnet.org Circulating the Facts for Peripheral Artery Disease: ABDOMINAL AORTIC ANEURYSM-Endovascular Repair Abdominal Aortic Aneurysms Objectives: Define Abdominal Aortic Aneurysm Identify the risk factors Discuss medical management and surgical repair of Abdominal Aortic Aneurysms Unit 1: Review of Aortic Anatomy Unit 2: Definition of Aortic Aneurysm Unit 3: Risk factors for Aneurysms Unit 4: Types of aneurysms Unit 5: Diagnostic tests for Abdominal Aortic Aneurysms Unit 6: Goals Unit 7: Treatment Unit 8: Endovascular repair of Abdominal Aortic Aneurysms Unit 9: Complications Unit 10: Post procedure care 1 6/2014 Circulating the Facts for Peripheral Artery Disease: ABDOMINAL AORTIC ANEURYSM-Endovascular Repair Unit 1: Review of Abdominal Aortic Anatomy The abdominal aorta is the largest blood vessel in the body and directs oxygenated blood flow from the heart to the rest of the body. This provides necessary food and oxygen to all body cells. The abdominal aorta contains the celiac, superior mesenteric, inferior mesenteric, renal and iliac arteries. It begins at the diaphragm and ends at the iliac artery branching. Unit 2: Definition of Abdominal Aortic Aneurysm Normally, the lining of an artery is strong and smooth, allowing for blood to flow easily through it. The arterial wall consists of three layers. A true aneurysm involves dilation of all three arterial wall layers. Abdominal aortic aneurysms occur over time due to changes of the arterial wall. The wall of the artery weakens and enlarges like a balloon (aneurysm). -

Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm (AAA) Abdominal aortic aneurysm (AAA) occurs when atherosclerosis or plaque buildup causes the walls of the abdominal aorta to become weak and bulge outward like a balloon. An AAA develops slowly over time and has few noticeable symptoms. The larger an aneurysm grows, the more likely it will burst or rupture, causing intense abdominal or back pain, dizziness, nausea or shortness of breath. Your doctor can confirm the presence of an AAA with an abdominal ultrasound, abdominal and pelvic CT or angiography. Treatment depends on the aneurysm's location and size as well as your age, kidney function and other conditions. Aneurysms smaller than five centimeters in diameter are typically monitored with ultrasound or CT scans every six to 12 months. Larger aneurysms or those that are quickly growing or leaking may require open or endovascular surgery. What is an abdominal aortic aneurysm? The aorta, the largest artery in the body, is a blood vessel that carries oxygenated blood away from the heart. It originates just after the aortic valve connected to the left side of the heart and extends through the entire chest and abdomen. The portion of the aorta that lies deep inside the abdomen, right in front of the spine, is called the abdominal aorta. Over time, artery walls may become weak and widen. An analogy would be what can happen to an aging garden hose. The pressure of blood pumping through the aorta may then cause this weak area to bulge outward, like a balloon (called an aneurysm). An abdominal aortic aneurysm (AAA, or "triple A") occurs when this type of vessel weakening happens in the portion of the aorta that runs through the abdomen. -

Cogan's Syndrome
IMAGING IN MEDICINE COLODETTI R ET AL. Cogan’s syndrome – A rare aortitis, difficult to diagnose but with therapeutic potential RAIZA COLODETTI1, GUILHERME SPINA2, TATIANA LEAL3, MUCIO OLIVEIRA JR4, ALEXANDRE SOEIRO3* 1MD Cardiologist, Instituto do Coração (InCor), Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil 2Assistant Physician at the Valvular Heart Disease Outpatient Clinic, InCor, HC-FMUSP, São Paulo, SP, Brazil 3Assistant Physician at the Clinical Emergency Service, InCor, HC-FMUSP, São Paulo, SP, Brazil 4Director of the Clinical Emergency Service, InCor, HC-FMUSP, São Paulo, SP, Brazil SUMMARY Study conducted at Unidade Clínica de Emergência, Instituto do Coração (InCor), The inflammation of aortic wall, named aortitis, is a rare condition that can Hospital das Clínicas, Faculdade de be caused by a number of pathologies, mainly inflammatory or infectious in Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil nature. In this context, the occurrence of combined audiovestibular and/or ocular manifestations eventually led to the diagnosis of Cogan’s syndrome, Article received: 8/18/2017 Accepted for publication: 9/9/2017 making it the rare case, but susceptible to adequate immunosuppressive treatment and satisfactory disease control. *Correspondence: Address: Av. Dr. Enéas de Carvalho Aguiar, 44 Keywords: chest pain, aortitis, Cogan’s syndrome. São Paulo, SP – Brazil Postal code: 05403-900 [email protected] http://dx.doi.org/10.1590/1806-9282.63.12.1028 INTRODUCTION four years ago the episodes began to intensify. He was Inflammation of the aortic wall, called aortitis, is an in- admitted to another service a week before for the same frequent clinical condition that manifests itself with sys- reason, where he underwent coronary angiography, show- temic symptoms and may cause precordial pain.1-4 One ing no coronary obstruction, and an echocardiogram, of the rheumatologic causes of aortitis is a rare disease which revealed a slight dilatation of the ascending aorta. -

Guideline-Management-Giant-Cell
Arthritis Care & Research Vol. 73, No. 8, August 2021, pp 1071–1087 DOI 10.1002/acr.24632 © 2021 American College of Rheumatology. This article has been contributed to by US Government employees and their work is in the public domain in the USA. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis Mehrdad Maz,1 Sharon A. Chung,2 Andy Abril,3 Carol A. Langford,4 Mark Gorelik,5 Gordon Guyatt,6 Amy M. Archer,7 Doyt L. Conn,8 Kathy A. Full,9 Peter C. Grayson,10 Maria F. Ibarra,11 Lisa F. Imundo,5 Susan Kim,2 Peter A. Merkel,12 Rennie L. Rhee,12 Philip Seo,13 John H. Stone,14 Sangeeta Sule,15 Robert P. Sundel,16 Omar I. Vitobaldi,17 Ann Warner,18 Kevin Byram,19 Anisha B. Dua,7 Nedaa Husainat,20 Karen E. James,21 Mohamad A. Kalot,22 Yih Chang Lin,23 Jason M. Springer,1 Marat Turgunbaev,24 Alexandra Villa-Forte, 4 Amy S. Turner,24 and Reem A. Mustafa25 Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particu- lar patient. The ACR considers adherence to the recommendations within this guideline to be voluntary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote beneficial or desirable outcomes but cannot guarantee any specific outcome. -

Risk Factors in Abdominal Aortic Aneurysm and Aortoiliac Occlusive
OPEN Risk factors in abdominal aortic SUBJECT AREAS: aneurysm and aortoiliac occlusive PHYSICAL EXAMINATION RISK FACTORS disease and differences between them in AORTIC DISEASES LIFESTYLE MODIFICATION the Polish population Joanna Miko ajczyk-Stecyna1, Aleksandra Korcz1, Marcin Gabriel2, Katarzyna Pawlaczyk3, Received Grzegorz Oszkinis2 & Ryszard S omski1,4 1 November 2013 Accepted 1Institute of Human Genetics, Polish Academy of Sciences, Poznan, 60-479, Poland, 2Department of Vascular Surgery, Poznan 18 November 2013 University of Medical Sciences, Poznan, 61-848, Poland, 3Department of Hypertension, Internal Medicine, and Vascular Diseases, Poznan University of Medical Sciences, Poznan, 61-848, Poland, 4Department of Biochemistry and Biotechnology of the Poznan Published University of Life Sciences, Poznan, 60-632, Poland. 18 December 2013 Abdominal aortic aneurysm (AAA) and aortoiliac occlusive disease (AIOD) are multifactorial vascular Correspondence and disorders caused by complex genetic and environmental factors. The purpose of this study was to define risk factors of AAA and AIOD in the Polish population and indicate differences between diseases. requests for materials should be addressed to J.M.-S. he total of 324 patients affected by AAA and 328 patients affected by AIOD was included. Previously (joannastecyna@wp. published population groups were treated as references. AAA and AIOD risk factors among the Polish pl) T population comprised: male gender, advanced age, myocardial infarction, diabetes type II and tobacco smoking. This study allowed defining risk factors of AAA and AIOD in the Polish population and could help to develop diagnosis and prevention. Characteristics of AAA and AIOD subjects carried out according to clinical data described studied disorders as separate diseases in spite of shearing common localization and some risk factors. -

A 69-Year-Old Woman with Intermittent Claudication and Elevated ESR
756 Self-assessment corner Postgrad Med J: first published as 10.1136/pgmj.74.878.756 on 1 December 1998. Downloaded from A 69-year-old woman with intermittent claudication and elevated ESR M L Amoedo, M P Marco, M D Boquet, S Muray, J M Piulats, M J Panades, J Ramos, E Fernandez A 69-year-old woman was referred to our out-patient clinic because of long-term hypertension and stable chronic renal failure (creatinine 132 ,umol/l), which had been attributed to nephroan- giosclerosis. She presented with a one-year history of anorexia, asthenia and loss of 6 kg ofweight. In addition, she complained of intermittent claudication of the left arm and both legs lasting 2 months. This provoked important functional limitation of the three limbs, and impaired ambula- tion. She did not complain of headache or symptoms suggestive of polymyalgia rheumatica. Her blood pressure was 160/95 mmHg on the right arm and undetectable on the left arm and lower limbs. Both temporal arteries were palpable and not painful. Auscultation of both carotid arteries was normal, without murmurs. Cardiac and pulmonary auscultation were normal. Mur- murs were audible on both subclavian arteries. Neither the humeral nor the radial pulse were detectable on the left upper limb. Murmurs were also audible on both femoral arteries, and nei- ther popliteal nor distal pulses were palpable. Her feet were cold although they had no ischaemic lesions. Funduscopic examination was essentially normal. The most relevant laboratory data were: erythrocyte sedimentation rate (ESR) 120 mm/h, C-reactive protein 4.4 mg/dl (normal range <1.5); antinuclear and antineutrophil cytoplasmic antibodies were negative. -

Crohn's Disease
Harvard-MIT Division of Health Sciences and Technology HST.121: Gastroenterology, Fall 2005 Instructors: Dr. Jonathan Glickman Vascular and Inflammatory Diseases of the Intestines Overview • Vascular disorders – Vascular “malformations” – Vasculitis – Ischemic disease • Inflammatory disorders of specific etiology – Infetious enterocolitis – “Immune-mediated” enteropathy – Diverticular disease • Idiopathic inflammatory bowel disease – Crohn’s disease – Ulcerative colitis Sporadic Vascular Ectasia (Telangiectasia) • Clusters of tortuous thin-walled small vessels lacking muscle or adventitia located in the mucosa and the submucosa • The most common type occurs in cecum or ascending colon of individuals over the age of 50 and is commonly known as “angiodysplasia” • Angiodysplasias account for 40% of all colonic vascular lesions and are the most common cause of lower GI bleeding in individuals over the age of 60 Angiodysplasia Hereditary Vascular Ectasia • Hereditary Hemorrhagic Telangiectasia (HHT) or Osler- Webber-Rendu disease • Systematic disease primarily involving skin and mucous membranes, and often the GI tract • Autosomal dominant disease with positive family history in 80% of cases • After epistaxis which occurs in 80% of individuals, GI bleed is the most frequent presentation and occurs in 10-40% of cases Arteriovenous Malformations (AVM’s) • Irregular meshwork of structurally abnormal medium to large ectatic vessels • Unlike small vessel ectasias, AVM’s can be distributed in all layers of the bowel wall • AVM’s may present anywhere