Identification of the Gene Expression Rules That
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Learning from Cadherin Structures and Sequences: Affinity Determinants and Protein Architecture
Learning from cadherin structures and sequences: affinity determinants and protein architecture Klára Fels ıvályi Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2014 © 2014 Klara Felsovalyi All rights reserved ABSTRACT Learning from cadherin structures and sequences: affinity determinants and protein architecture Klara Felsovalyi Cadherins are a family of cell-surface proteins mediating adhesion that are important in development and maintenance of tissues. The family is defined by the repeating cadherin domain (EC) in their extracellular region, but they are diverse in terms of protein size, architecture and cellular function. The best-understood subfamily is the type I classical cadherins, which are found in vertebrates and have five EC domains. Among the five different type I classical cadherins, the binding interactions are highly specific in their homo- and heterophilic binding affinities, though their sequences are very similar. As previously shown, E- and N-cadherins, two prototypic members of the subfamily, differ in their homophilic K D by about an order of magnitude, while their heterophilic affinity is intermediate. To examine the source of the binding affinity differences among type I cadherins, we used crystal structures, analytical ultracentrifugation (AUC), surface plasmon resonance (SPR), and electron paramagnetic resonance (EPR) studies. Phylogenetic analysis and binding affinity behavior show that the type I cadherins can be further divided into two subgroups, with E- and N-cadherin representing each. In addition to the affinity differences in their wild-type binding through the strand-swapped interface, a second interface also shows an affinity difference between E- and N-cadherin. -

The Conserved DNMT1-Dependent Methylation Regions in Human Cells
Freeman et al. Epigenetics & Chromatin (2020) 13:17 https://doi.org/10.1186/s13072-020-00338-8 Epigenetics & Chromatin RESEARCH Open Access The conserved DNMT1-dependent methylation regions in human cells are vulnerable to neurotoxicant rotenone exposure Dana M. Freeman1 , Dan Lou1, Yanqiang Li1, Suzanne N. Martos1 and Zhibin Wang1,2,3* Abstract Background: Allele-specifc DNA methylation (ASM) describes genomic loci that maintain CpG methylation at only one inherited allele rather than having coordinated methylation across both alleles. The most prominent of these regions are germline ASMs (gASMs) that control the expression of imprinted genes in a parent of origin-dependent manner and are associated with disease. However, our recent report reveals numerous ASMs at non-imprinted genes. These non-germline ASMs are dependent on DNA methyltransferase 1 (DNMT1) and strikingly show the feature of random, switchable monoallelic methylation patterns in the mouse genome. The signifcance of these ASMs to human health has not been explored. Due to their shared allelicity with gASMs, herein, we propose that non-tradi- tional ASMs are sensitive to exposures in association with human disease. Results: We frst explore their conservancy in the human genome. Our data show that our putative non-germline ASMs were in conserved regions of the human genome and located adjacent to genes vital for neuronal develop- ment and maturation. We next tested the hypothesized vulnerability of these regions by exposing human embryonic kidney cell HEK293 with the neurotoxicant rotenone for 24 h. Indeed,14 genes adjacent to our identifed regions were diferentially expressed from RNA-sequencing. We analyzed the base-resolution methylation patterns of the predicted non-germline ASMs at two neurological genes, HCN2 and NEFM, with potential to increase the risk of neurodegenera- tion. -

A Discovery Resource of Rare Copy Number Variations in Individuals with Autism Spectrum Disorder
INVESTIGATION A Discovery Resource of Rare Copy Number Variations in Individuals with Autism Spectrum Disorder Aparna Prasad,* Daniele Merico,* Bhooma Thiruvahindrapuram,* John Wei,* Anath C. Lionel,*,† Daisuke Sato,* Jessica Rickaby,* Chao Lu,* Peter Szatmari,‡ Wendy Roberts,§ Bridget A. Fernandez,** Christian R. Marshall,*,†† Eli Hatchwell,‡‡ Peggy S. Eis,‡‡ and Stephen W. Scherer*,†,††,1 *The Centre for Applied Genomics, Program in Genetics and Genome Biology, The Hospital for Sick Children, Toronto M5G 1L7, Canada, †Department of Molecular Genetics, University of Toronto, Toronto M5G 1L7, Canada, ‡Offord Centre for Child Studies, Department of Psychiatry and Behavioural Neurosciences, McMaster University, Hamilton L8P 3B6, § Canada, Autism Research Unit, The Hospital for Sick Children, Toronto M5G 1X8, Canada, **Disciplines of Genetics and Medicine, Memorial University of Newfoundland, St. John’s, Newfoundland A1B 3V6, Canada, ††McLaughlin Centre, University of Toronto, Toronto M5G 1L7, Canada, and ‡‡Population Diagnostics, Inc., Melville, New York 11747 ABSTRACT The identification of rare inherited and de novo copy number variations (CNVs) in human KEYWORDS subjects has proven a productive approach to highlight risk genes for autism spectrum disorder (ASD). A rare variants variety of microarrays are available to detect CNVs, including single-nucleotide polymorphism (SNP) arrays gene copy and comparative genomic hybridization (CGH) arrays. Here, we examine a cohort of 696 unrelated ASD number cases using a high-resolution one-million feature CGH microarray, the majority of which were previously chromosomal genotyped with SNP arrays. Our objective was to discover new CNVs in ASD cases that were not detected abnormalities by SNP microarray analysis and to delineate novel ASD risk loci via combined analysis of CGH and SNP array cytogenetics data sets on the ASD cohort and CGH data on an additional 1000 control samples. -

393LN V 393P 344SQ V 393P Probe Set Entrez Gene
393LN v 393P 344SQ v 393P Entrez fold fold probe set Gene Gene Symbol Gene cluster Gene Title p-value change p-value change chemokine (C-C motif) ligand 21b /// chemokine (C-C motif) ligand 21a /// chemokine (C-C motif) ligand 21c 1419426_s_at 18829 /// Ccl21b /// Ccl2 1 - up 393 LN only (leucine) 0.0047 9.199837 0.45212 6.847887 nuclear factor of activated T-cells, cytoplasmic, calcineurin- 1447085_s_at 18018 Nfatc1 1 - up 393 LN only dependent 1 0.009048 12.065 0.13718 4.81 RIKEN cDNA 1453647_at 78668 9530059J11Rik1 - up 393 LN only 9530059J11 gene 0.002208 5.482897 0.27642 3.45171 transient receptor potential cation channel, subfamily 1457164_at 277328 Trpa1 1 - up 393 LN only A, member 1 0.000111 9.180344 0.01771 3.048114 regulating synaptic membrane 1422809_at 116838 Rims2 1 - up 393 LN only exocytosis 2 0.001891 8.560424 0.13159 2.980501 glial cell line derived neurotrophic factor family receptor alpha 1433716_x_at 14586 Gfra2 1 - up 393 LN only 2 0.006868 30.88736 0.01066 2.811211 1446936_at --- --- 1 - up 393 LN only --- 0.007695 6.373955 0.11733 2.480287 zinc finger protein 1438742_at 320683 Zfp629 1 - up 393 LN only 629 0.002644 5.231855 0.38124 2.377016 phospholipase A2, 1426019_at 18786 Plaa 1 - up 393 LN only activating protein 0.008657 6.2364 0.12336 2.262117 1445314_at 14009 Etv1 1 - up 393 LN only ets variant gene 1 0.007224 3.643646 0.36434 2.01989 ciliary rootlet coiled- 1427338_at 230872 Crocc 1 - up 393 LN only coil, rootletin 0.002482 7.783242 0.49977 1.794171 expressed sequence 1436585_at 99463 BB182297 1 - up 393 -

Thousands of Cpgs Show DNA Methylation Differences in ACPA-Positive Individuals
G C A T T A C G G C A T genes Article Thousands of CpGs Show DNA Methylation Differences in ACPA-Positive Individuals Yixiao Zeng 1,2, Kaiqiong Zhao 2,3, Kathleen Oros Klein 2, Xiaojian Shao 4, Marvin J. Fritzler 5, Marie Hudson 2,6,7, Inés Colmegna 6,8, Tomi Pastinen 9,10, Sasha Bernatsky 6,8 and Celia M. T. Greenwood 1,2,3,9,11,* 1 PhD Program in Quantitative Life Sciences, Interfaculty Studies, McGill University, Montréal, QC H3A 1E3, Canada; [email protected] 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montréal, QC H3T 1E2, Canada; [email protected] (K.Z.); [email protected] (K.O.K.); [email protected] (M.H.) 3 Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montréal, QC H3A 1A2, Canada 4 Digital Technologies Research Centre, National Research Council Canada, Ottawa, ON K1A 0R6, Canada; [email protected] 5 Cumming School of Medicine, University of Calgary, Calgary, AB T2N 1N4, Canada; [email protected] 6 Department of Medicine, McGill University, Montréal, QC H4A 3J1, Canada; [email protected] (I.C.); [email protected] (S.B.) 7 Division of Rheumatology, Jewish General Hospital, Montréal, QC H3T 1E2, Canada 8 Division of Rheumatology, McGill University, Montréal, QC H3G 1A4, Canada 9 Department of Human Genetics, McGill University, Montréal, QC H3A 0C7, Canada; [email protected] 10 Center for Pediatric Genomic Medicine, Children’s Mercy, Kansas City, MO 64108, USA 11 Gerald Bronfman Department of Oncology, McGill University, Montréal, QC H4A 3T2, Canada * Correspondence: [email protected] Citation: Zeng, Y.; Zhao, K.; Oros Abstract: High levels of anti-citrullinated protein antibodies (ACPA) are often observed prior to Klein, K.; Shao, X.; Fritzler, M.J.; Hudson, M.; Colmegna, I.; Pastinen, a diagnosis of rheumatoid arthritis (RA). -

Distinct Transcriptomes Define Rostral and Caudal 5Ht Neurons
DISTINCT TRANSCRIPTOMES DEFINE ROSTRAL AND CAUDAL 5HT NEURONS by CHRISTI JANE WYLIE Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Dissertation Advisor: Dr. Evan S. Deneris Department of Neurosciences CASE WESTERN RESERVE UNIVERSITY May, 2010 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of ______________________________________________________ candidate for the ________________________________degree *. (signed)_______________________________________________ (chair of the committee) ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. TABLE OF CONTENTS TABLE OF CONTENTS ....................................................................................... iii LIST OF TABLES AND FIGURES ........................................................................ v ABSTRACT ..........................................................................................................vii CHAPTER 1 INTRODUCTION ............................................................................................... 1 I. Serotonin (5-hydroxytryptamine, 5HT) ....................................................... 1 A. Discovery.............................................................................................. -

Remote Memory and Cortical Synaptic Plasticity Require Neuronal CCCTC-Binding Factor (CTCF)
5042 • The Journal of Neuroscience, May 30, 2018 • 38(22):5042–5052 Cellular/Molecular Remote Memory and Cortical Synaptic Plasticity Require Neuronal CCCTC-Binding Factor (CTCF) X Somi Kim,1* Nam-Kyung Yu,1* Kyu-Won Shim,2 XJi-il Kim,1 X Hyopil Kim,1 Dae Hee Han,1 XJa Eun Choi,1 X Seung-Woo Lee,1 X Dong Il Choi,1 Myung Won Kim,1 Dong-Sung Lee,3 Kyungmin Lee,4 Niels Galjart,5 X Yong-Seok Lee,6 XJae-Hyung Lee,7 and XBong-Kiun Kaang1 1Department of Biological Sciences, College of Natural Sciences, Seoul National University, Seoul 08826, South Korea, 2Interdisciplinary Program in Bioinformatics, Seoul National University, Seoul 08826, South Korea, 3Salk Institute for Biological Studies, La Jolla, California 92130, 4Department of Anatomy, Graduate School of Medicine, Kyungpook National University, Daegu 700-422, Korea, 5Department of Cell Biology and Genetics, 3000 CA Rotterdam, The Netherlands, 6Department of Physiology, Seoul National University College of Medicine, Seoul 03080, South Korea, and 7Department of Life and Nanopharmaceutical Sciences, Department of Maxillofacial Biomedical Engineering, School of Dentistry, Kyung Hee University, Seoul 02447, South Korea The molecular mechanism of long-term memory has been extensively studied in the context of the hippocampus-dependent recent memory examined within several days. However, months-old remote memory maintained in the cortex for long-term has not been investigated much at the molecular level yet. Various epigenetic mechanisms are known to be important for long-term memory, but how the 3D chromatin architecture and its regulator molecules contribute to neuronal plasticity and systems consolidation is still largely unknown. -

Identification of Functional Genetic Variants in Inflammatory Bowel Disease by Genome and Transcriptome Sequencing
Identification of Functional Genetic Variants in Inflammatory Bowel Disease by Genome and Transcriptome Sequencing Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultät der Christian-Albrechts-Universität zu Kiel vorgelegt von Matthias Barann August, 2012 Kiel, Deutschland 1 2 Referent/in: Prof. Dr. Philip Rosenstiel Korreferent/in: Prof. Dr. Dr. h.c. Thomas Bosch Tag der mündlichen Prüfung: 31.10.2012 Zum Druck genehmigt: 31.10.2012 gez. Prof. Dr. Wolfgang J. Duschl, Dekan 3 Parts of this dissertation are contained in the following two manuscripts. Rosenstiel R, Barann M, Klostermeier UC, Sheth V, Ellinghaus D, Rausch T, Korbel J, Nothnagel M, Krawczak M, Gilissen C, Veltman J, Forster M, Stade B, McLaughlin S, Lee CC, Fritscher-Ravens A, Franke A, Schreiber S. Whole Genome Sequence of a Crohn disease trio Barann M, Klostermeier UC, Esser D, Ammerpohl O, Siebert R, Sudbrak R, Lehrach H, Schreiber S, Rosenstiel R. Janus – Investigating the two faces of transcription 4 Contents 1. Introduction ............................................................................................................................. 7 1.1. Pathogenesis of inflammatory bowel diseases ...................................................................................... 8 1.2. Physical barrier function of the gut ......................................................................................................... 11 1.3. Pathogen recognition .................................................................................................................................. -
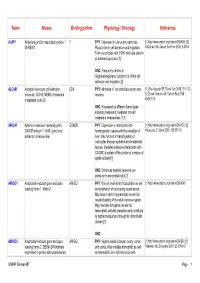
Name Aliases Binding Partner Physiology / Oncology References
Name Aliases Binding partner Physiology / Oncology References AJAP1 Adherens junction associated protein 1, ? PHY : Expressed in uterus and pancreas. [1] http://www.uniprot.org/uniprot/Q9UKB5. [2] SHREW1 Plays a role in cell adhesion and migration. McDonald JM, Cancer Biol Ther 2006, 5:300-4 Forms a complex with CDH1 and beta-catenin at adherens junctions [1] ONC : Frequently deleted in oligodendrogliomas, functions to inhibit cell adhesion and migration [2] ALCAM Activated leukocyte cell adhesion CD6 PHY : Adhesion of activated leukocytes and [1] Ofori-Acquah SF, Transl Res 2008, 151:122- molecule, CD166, MEMD (melanoma neurons 8. [2] van Kilsdonk JW, Cancer Res 2008, metastasis clone D) 68:3671-9 ONC : Expressed by different tumor types including melanoma; mediates cancer/ melanoma invasiveness [1,2] AMICA1 Adhesion molecule interacting with CXADR PHY : Expression is restricted to the [1] http://www.uniprot.org/uniprot/Q86YT9. [2] CXADR antigen 1, JAML (junctional hematopoietic tissues with the exception of Moog-Lutz C, Blood 2003, 102:3371-8 adhesion molecule-like) liver. May function in transmigration of leukocytes through epithelial and endothelial tissues. Mediates adhesive interactions with CXADR, a protein of the junctional complex of epithelial cells [1] ONC : Enhances myeloid leukemia cell adhesion to endothelial cells [2] AMIGO1 Amphoterin-induced gene and open AMIGO PHY : May be involved in fasciculation as well [1] http://www.uniprot.org/uniprot/Q86WK6 reading frame 1, Alivin-2 as myelination of developing neural axons. May have a role in regeneration as well as neural plasticity in the adult nervous system. May mediate homophilic as well as heterophilic cell-cell interaction and contribute to signal transduction through its intracellular domain [1] ONC : - AMIGO2 Amphoterin-induced gene and open AMIGO PHY : Highest levels in breast, ovary, cervix, [1] http://www.uniprot.org/uniprot/Q86SJ2. -

H3K27 Methylation Dynamics During CD4 T Cell Activation: Regulation of JAK/STAT and IL12RB2 Expression by JMJD3
H3K27 Methylation Dynamics during CD4 T Cell Activation: Regulation of JAK/STAT and IL12RB2 Expression by JMJD3 This information is current as Sarah A. LaMere, Ryan C. Thompson, Xiangzhi Meng, H. of September 24, 2021. Kiyomi Komori, Adam Mark and Daniel R. Salomon J Immunol published online 25 September 2017 http://www.jimmunol.org/content/early/2017/09/23/jimmun ol.1700475 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2017/09/23/jimmunol.170047 Material 5.DCSupplemental http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2017 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published September 25, 2017, doi:10.4049/jimmunol.1700475 The Journal of Immunology H3K27 Methylation Dynamics during CD4 T Cell Activation: Regulation of JAK/STAT and IL12RB2 Expression by JMJD3 Sarah A. LaMere,1 Ryan C. Thompson, Xiangzhi Meng, H. Kiyomi Komori,2 Adam Mark,1 and Daniel R. -
Evolutionary Perspective and Expression Analysis of Intronless Genes Highlight the Conservation of Their Regulatory Role
fgene-12-654256 July 5, 2021 Time: 19:1 # 1 ORIGINAL RESEARCH published: 09 July 2021 doi: 10.3389/fgene.2021.654256 Evolutionary Perspective and Expression Analysis of Intronless Genes Highlight the Conservation of Their Regulatory Role Katia Aviña-Padilla1,2, José Antonio Ramírez-Rafael3, Gabriel Emilio Herrera-Oropeza1,4, Edited by: Vijaykumar Yogesh Muley1, Dulce I. Valdivia2, Erik Díaz-Valenzuela2, Katja Nowick, Andrés García-García3, Alfredo Varela-Echavarría1* and Maribel Hernández-Rosales2* Freie Universität Berlin, Germany 1 Instituto de Neurobiología, Universidad Nacional Autónoma de México, Querétaro, Mexico, 2 Centro de Investigacioìn y Reviewed by: de Estudios Avanzados del IPN, Unidad Irapuato, Guanajuato, Mexico, 3 Centro de Física Aplicada y Tecnología Avanzada, Jarosław Bryk, Universidad Nacional Autónoma de México, Querétaro, Mexico, 4 Centre for Developmental Neurobiology, Institute University of Huddersfield, of Psychiatry, Psychology, and Neuroscience, King’s College London, London, United Kingdom United Kingdom Scott William Roy, San Francisco State University, The structure of eukaryotic genes is generally a combination of exons interrupted by United States intragenic non-coding DNA regions (introns) removed by RNA splicing to generate Ekaterina Shelest, University of Portsmouth, the mature mRNA. A fraction of genes, however, comprise a single coding exon United Kingdom with introns in their untranslated regions or are intronless genes (IGs), lacking introns *Correspondence: entirely. The latter code for essential proteins involved in development, growth, and cell Alfredo Varela-Echavarría [email protected] proliferation and their expression has been proposed to be highly specialized for neuro- Maribel Hernández-Rosales specific functions and linked to cancer, neuropathies, and developmental disorders. The [email protected] abundant presence of introns in eukaryotic genomes is pivotal for the precise control Specialty section: of gene expression.