Transplantation of Engineered Chimeric Liver with Autologous
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multi-Omic Understanding of the Evolution of Xenobiotic Tolerance in Bacterial Isolates and Communities
Washington University in St. Louis Washington University Open Scholarship Arts & Sciences Electronic Theses and Dissertations Arts & Sciences Summer 8-15-2019 Multi-omic Understanding of the Evolution of Xenobiotic Tolerance in Bacterial Isolates and Communities Tayte Paul Campbell Washington University in St. Louis Follow this and additional works at: https://openscholarship.wustl.edu/art_sci_etds Part of the Bioinformatics Commons, Biology Commons, and the Microbiology Commons Recommended Citation Campbell, Tayte Paul, "Multi-omic Understanding of the Evolution of Xenobiotic Tolerance in Bacterial Isolates and Communities" (2019). Arts & Sciences Electronic Theses and Dissertations. 1888. https://openscholarship.wustl.edu/art_sci_etds/1888 This Dissertation is brought to you for free and open access by the Arts & Sciences at Washington University Open Scholarship. It has been accepted for inclusion in Arts & Sciences Electronic Theses and Dissertations by an authorized administrator of Washington University Open Scholarship. For more information, please contact [email protected]. WASHINGTON UNIVERSITY IN ST. LOUIS Division of Biology and Biomedical Sciences Plant and Microbial Biosciences Dissertation Examination Committee: Gautam Dantas, Chair Arpita Bose Andrew Kau Audrey Odom-John Himadri Pakrasi Fuzhong Zhang Multi-omic Understanding of the Evolution of Xenobiotic Tolerance in Bacterial Isolates and Communities by Tayte P. Campbell A dissertation presented to The Graduate School of Washington University in partial fulfillment -

Polychlorinated Biphenyls in Pigments
doi: 10.1111/cote.12167 Polychlorinated biphenyls in pigments: inadvertent production and environmental Coloration significance Technology Lisa Rodenburg,a Jia Guoa and Robert Christieb,* aDepartment of Environmental Science, Rutgers, The State University of New Jersey, New Brunswick, NJ, 08901, USA bSchool of Textiles and Design, Heriot-Watt University, Scottish Borders Campus, Netherdale, Galashiels, TD1 3HF, UK Feature article Email: [email protected] Society of Dyers and Colourists Received: 18 December 2014; Accepted: 26 June 2015 Polychlorobiphenyls are toxic, bioaccumulative, and persistent chemicals whose intentional manufacture has been banned throughout the developed world. Polychlorobiphenyls may be generated inadvertently during the production of certain pigments, including diarylides. This inadvertent production is allowed under various regulatory schemes, such as the Toxic Substances Control Act in the United States and the Stockholm Convention on Persistent Organic Pollutants. Generally, these regulations require polychlorobiphenyl levels in batches of pigment to be less than certain regulatory limits, usually 50 ppm. A growing body of evidence suggests that the use of pigments is dispersing polychlorobiphenyls throughout the environment. Polychlorobiphenyl congeners associated with pigments have been found throughout the United States in sediments and in surface waters at levels exceeding the prevailing water quality standards. A recent Japanese government study reported measured polychlorobiphenyl concentrations well -
Development of a Transplantable Liver Graft from a Tiny Partial Liver( Dissertation 全文 )
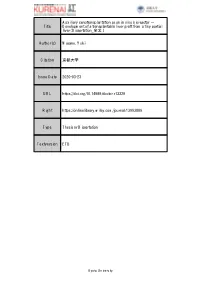
Auxiliary xenotransplantation as an in vivo bioreactor - Title Development of a transplantable liver graft from a tiny partial liver( Dissertation_全文 ) Author(s) Masano, Yuki Citation 京都大学 Issue Date 2020-03-23 URL https://doi.org/10.14989/doctor.r13329 Right https://onlinelibrary.wiley.com/journal/13993089 Type Thesis or Dissertation Textversion ETD Kyoto University Received: 27 November 2018 | Revised: 25 May 2019 | Accepted: 27 June 2019 DOI: 10.1111/xen.12545 ORIGINAL ARTICLE Auxiliary xenotransplantation as an in vivo bioreactor— Development of a transplantable liver graft from a tiny partial liver Yuki Masano1 | Shintaro Yagi1 | Yosuke Miyachi1 | Shinya Okumura1 | Toshimi Kaido1 | Hironori Haga2 | Eiji Kobayashi3 | Shinji Uemoto1 1Division of Hepato‐Biliary‐Pancreatic and Transplant Surgery, Department of Surgery, Abstract Graduate School of Medicine, Kyoto Background: We established a completely novel method of auxiliary xenogeneic University, Kyoto, Japan partial liver transplantation and examined whether liver grafts procured from Syrian 2Department of Diagnostic Pathology, Kyoto University Hospital, Kyoto, Japan hamsters regenerated in nude rats, which were used as in vivo bioreactors. 3Department of Organ Fabrication, Keio Methods: The hamsters and the rats were all males (n = 10). Partial liver grafts from University School of Medicine, Tokyo, Japan hamsters were transplanted into nude rats in an auxiliary manner. We evaluated liver Correspondence graft injury, rejection, and regeneration during 7 days after auxiliary xenogeneic par- Shintaro Yagi, 54 Kawahara‐cho, Shogoin, Sakyo‐ku, Kyoto, 606‐8507, Japan. tial liver transplantation. Email: [email protected]‐u.ac.jp Results: All rats survived until sacrifice on post‐operative day (POD) 1, 3, and 7. HE‐ Funding information staining showed normal at POD1, mild periportal edema, and slight bile duct and Japan Society for the Promotion of Science, venous endothelial inflammation at POD3, and moderate acute cellular rejection at Grant/Award Number: 17H06814 POD7 without parenchymal necrosis. -

Development of Fluorescent Substrates for Microsomal Epoxide Hydrolase
Analytical Biochemistry 414 (2011) 154–162 Contents lists available at ScienceDirect Analytical Biochemistry journal homepage: www.elsevier.com/locate/yabio Development of fluorescent substrates for microsomal epoxide hydrolase and application to inhibition studies ⇑ Christophe Morisseau a, , Maud Bernay a, Aurélie Escaich a, James R. Sanborn a, Jozsef Lango b, Bruce D. Hammock a a Department of Entomology and Cancer Center, University of California – Davis, Davis, CA 95616, USA b Department of Molecular Biosciences, University of California – Davis, Davis, CA 95616, USA article info abstract Article history: The microsomal epoxide hydrolase (mEH) plays a significant role in the metabolism of numerous Received 18 January 2011 xenobiotics. In addition, it has a potential role in sexual development and bile acid transport, and it is Received in revised form 23 February 2011 associated with a number of diseases such as emphysema, spontaneous abortion, eclampsia, and several Accepted 25 February 2011 forms of cancer. Toward developing chemical tools to study the biological role of mEH, we designed and Available online 1 March 2011 synthesized a series of absorbent and fluorescent substrates. The highest activity for both rat and human mEH was obtained with the fluorescent substrate cyano(6-methoxy-naphthalen-2-yl)methyl glycidyl Keywords: carbonate (11). An in vitro inhibition assay using this substrate ranked a series of known inhibitors sim- Microsomal epoxide hydrolase ilarly to the assay that used radioactive cis-stilbene oxide but with a greater discrimination between Fluorescent substrate a-Cyanocarbonate inhibitors. These results demonstrate that the new fluorescence-based assay is a useful tool for the dis- Xenobiotic metabolism covery of structure–activity relationships among mEH inhibitors. -

Animal Plant Warfare and Secondary Metabolite Evolution
Review Nat. Prod. Bioprospect. 2013, 3, 1–7 DOI 10.1007/s13659-013-0004-0 Animal plant warfare and secondary metabolite evolution a a b a, Steffen WÖLL, Sun Hee KIM, Henry Johannes GRETEN, and Thomas EFFERTH * aDepartment of Pharmaceutical Biology, Institute of Pharmacy and Biochemistry, Johannes Gutenberg-University, Mainz, Germany bInstitute of Biomedical Sciences (ICBAS), University of Porto, Portugal Received 10 January 2013; Accepted 16 February 2013 © The Author(s) 2013. This article is published with open access at Springerlink.com Abstract: The enduring discussion, why plants produce secondary metabolites with pharmacologically and toxicologically active towards mammals traces back to the eminent role of medicinal plants in the millennia-old history of manhood. In recent years, the concept of an animal plant warfare emerged, which focused on the co-evolution between plants and herbivores. As a reaction to herbivory, plants developed mechanical defenses such as thorns and hard shells, which paved the way for adapted animal physiques. Plants evolved further defense systems by producing chemicals that exert toxic effects on the animals that ingest them. As a result of this selective pressure, animals developed special enzymes, e.g. cytochrome P450 monooxigenases (CYP450) that metabolize xenobiotic phytochemicals. As a next step in the evolutionary competition between plants and animals, plants evolved to produce non-toxic pro-drugs, which become toxic only after ingestion by animals through metabolization by enzymes such as CYP450. Because these sequestered evolutionary developments call to mind an arms race, the term animal plant warfare has been coined. The evolutionary competition between plants and animals may help to better understand the modes of action of medicinal plants and to foster the efficient and safe use of phytotherapy nowadays. -

Selection of Endophytic Strains for Enhanced Bacteria-Assisted Phytoremediation of Organic Pollutants Posing a Public Health Hazard
International Journal of Molecular Sciences Review Selection of Endophytic Strains for Enhanced Bacteria-Assisted Phytoremediation of Organic Pollutants Posing a Public Health Hazard Magdalena Anna Kara´s*, Sylwia Wdowiak-Wróbel and Wojciech Sokołowski Department of Genetics and Microbiology, Institute of Biological Sciences, Faculty of Biology and Biotechnology, Maria Curie-Skłodowska University, Akademicka 19, 20-033 Lublin, Poland; [email protected] (S.W.-W.); [email protected] (W.S.) * Correspondence: [email protected]; Tel.: +48-81-537-50-58 Abstract: Anthropogenic activities generate a high quantity of organic pollutants, which have an impact on human health and cause adverse environmental effects. Monitoring of many hazardous contaminations is subject to legal regulations, but some substances such as therapeutic agents, personal care products, hormones, and derivatives of common organic compounds are currently not included in these regulations. Classical methods of removal of organic pollutants involve economically challenging processes. In this regard, remediation with biological agents can be an alternative. For in situ decontamination, the plant-based approach called phytoremediation can be used. However, the main disadvantages of this method are the limited accumulation capacity of plants, sensitivity to the action of high concentrations of hazardous pollutants, and no possibility of using pollutants for growth. To overcome these drawbacks and additionally increase the efficiency of Citation: Kara´s,M.A.; the process, an integrated technology of bacteria-assisted phytoremediation is being used recently. Wdowiak-Wróbel, S.; Sokołowski, W. For the system to work, it is necessary to properly select partners, especially endophytes for specific Selection of Endophytic Strains for Enhanced Bacteria-Assisted plants, based on the knowledge of their metabolic abilities and plant colonization capacity. -
The Evolutionary Significance of Drug Toxicity Over Reward
The evolutionary significance of drug toxicity over reward Edward H. Hagen and Roger J. Sullivan Forthcoming in the Routledge Handbook of Philosophy and Science of Addiction, S. Ahmed and H. Pickard, eds. Drug reward is an evolutionary conundrum. It is not surprising that neural circuitry evolved to reward or reinforce behaviors leading to the essentials of survival and reproduction, like food, water, and sex. Why, though, would these same circuits reward and reinforce the consumption of drugs of abuse, which is often harmful? Here we briefly review the history of reward-based learning, which resulted in a widely accepted evolutionary account of drug reward that we term the hijack hypothesis. We then critique the evolutionary bases of the hijack hypothesis. We conclude by sketching an alternative evolutionary model of human drug use grounded in drug toxicity. Specifically, avoidance of toxic drugs is a compelling hypothesis for the low use of drugs by children and women relative to men. In addition, the regulated ingestion of small quantities of toxins might have provided important medicinal and other benefits to humans and non-human animals over the course of their evolution. Neurobiological theories of drug use are deeply intertwined with those of reward- based learning. The main idea was captured in Thorndike’s law of effect: “Of several responses made to the same situation, those which are accompanied or closely followed by satisfaction to the animal will, other things being equal, be more firmly connected with the situation, so that, when it recurs, they will be more likely to recur" (Thorndike 1911). The related concept of reinforcement refers to the ability of certain stimuli, such as food, to strengthen learned stimulus-response associations. -

Phytoremediation: an Analytical Technique for the Assessment of Biodegradation of Organic Xenobiotic Pollutants: a Review
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2013): 6.14 | Impact Factor (2013): 4.438 Phytoremediation: An Analytical Technique for the Assessment of Biodegradation of Organic Xenobiotic Pollutants: A Review Adil Sikandar1, Kiran Shehzadi2, Qiraat Arshad3, Komal Munir4 Institute of Life Sciences, Department of Environmental Sciences, Hafiz Hayat Campus, University of Gujrat, Punjab, Pakistan. [email protected] Abstract: Phytoremediation is an emerging environmental friendly approach for remediation of contaminated sites using plants, is the matter of great attention from the past few years. Environmental problems are caused mainly due to accumulation of industrial effluents which form xenobiotants. There is an immediate need to degrade these xenobiotic compounds in an eco-friendly way. Various techniques that have been in use are microbial remediation, phytoremediation and photoremediation. Each having its own ways of degradation, and also have some impacts on the environment. This review examines the developments in the use of transgenic plants for the degradation and phytoremediation of organic xenobiotics. From last many years, considerable progress has been made to increase the efficiency and effectiveness of phytoremediation. Still the technique is not widely in use as it could be for the treatment of contaminated sites. Present studies with transgenic plants indicate that specific degradation capabilities can be added to plants for remediation of pollutants. Keywords: Phytoremediation, Biodegradation, Xenobiotics, Pollutants 1. Introduction Due to man-made activities and natural processes environmental problems are increasing day by day which is a Biodegradation is the total breakdown of the complex and result of increase in population, industrialization, and toxic contaminants into non-toxic elements by the action of urbanization. -

Evidence for the Role of CYP51A and Xenobiotic Detoxification In
International Journal of Molecular Sciences Article Evidence for the Role of CYP51A and Xenobiotic Detoxification in Differential Sensitivity to Azole Fungicides in Boxwood Blight Pathogens Stefanos Stravoravdis 1,2, Robert E. Marra 3 , Nicholas R. LeBlanc 4,5, Jo Anne Crouch 4 and Jonathan P. Hulvey 2,* 1 Department of Microbiology, University of Massachusetts Amherst, Amherst, MA 01003, USA; [email protected] 2 Biology Department, Eastern Connecticut State University, Willimantic, CT 06226, USA 3 Department of Plant Pathology and Ecology, The Connecticut Agricultural Experiment Station, New Haven, CT 06504, USA; [email protected] 4 Mycology and Nematology Genetic Diversity and Biology Laboratory, United States Department of Agriculture, Agricultural Research Service, Beltsville, MD 20705, USA; [email protected] (N.R.L.); [email protected] (J.A.C.) 5 ARS Research Participation Program, Oak Ridge Institute for Science and Education, Oak Ridge, TN 37831-0117, USA * Correspondence: [email protected] Abstract: Boxwood blight, a fungal disease of ornamental plants (Buxus spp.), is caused by two sister species, Calonectria pseudonaviculata (Cps) and C. henricotiae (Che). Compared to Cps, Che is documented to display reduced sensitivity to fungicides, including the azole class of antifungals, Citation: Stravoravdis, S.; Marra, which block synthesis of a key fungal membrane component, ergosterol. A previous study reported R.E.; LeBlanc, N.R.; Crouch, J.A.; an ergosterol biosynthesis gene in Cps, CYP51A, to be a pseudogene, and RNA-Seq data confirm that a Hulvey, J.P. Evidence for the Role of functional CYP51A is expressed only in Che. The lack of additional ergosterol biosynthesis genes show- CYP51A and Xenobiotic ing significant differential expression suggests that the functional CYP51A in Che could contribute to Detoxification in Differential reduced azole sensitivity when compared to Cps. -

Xenobiotics: an Essential Precursor for Living System
American Journal of Advanced Drug Delivery www.ajadd.co.uk Review Article Xenobiotics: An Essential Precursor for Living System Dhaval K. Patel* and Dr. Dhrubo Jyoti Sen Department of Pharmaceutical Chemistry, Shri Sarvajanik Pharmacy College, Gujarat Technological University, Arvind Baug, Mehsana-384001, Gujarat, India Date of Receipt- 20/07/2013 ABSTRACT Date of Revision- 22/07/2013 Date of Acceptance- 24/07/2013 A xenobiotic is a chemical which is found in an organism but which is not normally produced or expected to be present in it. It can also cover substances which are present in much higher concentrations than are usual. Specifically, drugs such as antibiotics are xenobiotics in humans because the human body does not produce them itself, nor are they part of a normal diet. Natural compounds can also become xenobiotics if they are taken up by another organism, such as the uptake of natural human hormones by fish found downstream of sewage treatment plant outfalls, or the chemical defenses produced by some organisms as protection against predators. Xenobiotic metabolism is the set of metabolic pathways that modify the chemical structure of xenobiotics. In general, drugs are metabolized more Address for slowly in fetal, neonatal and elderly humans and animals than in Correspondence adults. The body removes xenobiotics by xenobiotic metabolism. Department of This consists of the deactivation and the excretion of xenobiotics and Pharmaceutical happens mostly in the liver. Excretion routes are urine, feces, breath, Chemistry, Shri and sweat. Hepatic enzymes are responsible for the metabolism of Sarvajanik Pharmacy xenobiotics by first activating them (oxidation, reduction, hydrolysis College, Gujarat and/or hydration of the xenobiotic) and then conjugating the active Technological secondary metabolite with glucuronic or sulphuric acid, or University, Arvind glutathione followed by excretion in bile or urine. -

Inhibition of Microsomal Epoxide Hydrolases by Ureas, Amides, and Amines
Chem. Res. Toxicol. 2001, 14, 409-415 409 Inhibition of Microsomal Epoxide Hydrolases by Ureas, Amides, and Amines Christophe Morisseau, John W. Newman, Deanna L. Dowdy, Marvin H. Goodrow, and Bruce D. Hammock* Department of Entomology and University of California Cancer Center, University of California, Davis, California 95616 Received August 11, 2000 The microsomal epoxide hydrolase (mEH) plays a significant role in the metabolism of xenobiotics such as polyaromatic toxicants. Additionally, polymorphism studies have underlined a potential role of this enzyme in relation to several diseases, such as emphysema, spontaneous abortion, and several forms of cancer. To provide new tools for studying the function of mEH, inhibition of this enzyme was investigated. Inhibition of recombinant rat and human mEH was achieved using primary ureas, amides, and amines. Several of these compounds are more potent than previously published inhibitors. Elaidamide, the most potent inhibitor that is obtained, has a Ki of 70 nM for recombinant rat mEH. This compound interacts with the enzyme forming a noncovalent complex, and blocks substrate turnover through an apparent mix of competitive and noncompetitive inhibition kinetics. Furthermore, in insect cell cultures expressing rat mEH, elaidamide enhances the toxicity effects of epoxide-containing xenobiotics. These inhibitors could be valuable tools for investigating the physiological and toxicological roles of mEH. Introduction Over the past decade, mEH was also described as mediating the transport of bile acid into hepatocytes (14, Epoxides are highly strained three-membered cyclic 15). The mechanism by which mEH participates in bile ethers that are often electrophilically reactive mutagens, absorption is not known. Obtaining potent mEH inhibi- carcinogens, or cytotoxins (1). -

Highly Chlorinated Pcbs Inhibit the Human Xenobiotic Response Mediated by the Steroid and Xenobiotic Receptor (SXR) Michelle M
Research | Article Highly Chlorinated PCBs Inhibit the Human Xenobiotic Response Mediated by the Steroid and Xenobiotic Receptor (SXR) Michelle M. Tabb,1 Vladyslav Kholodovych,2 Felix Grün1, Changcheng Zhou,1 William J. Welsh,2 and Bruce Blumberg1 1Department of Developmental and Cell Biology, University of California, Irvine, California, USA; 2University of Medicine & Dentistry of New Jersey–Robert Wood Johnson Medical School and The UMDNJ Informatics Institute, Piscataway, New Jersey USA (Blumberg et al. 1998; Jones et al. 2000; Polychlorinated biphenyls (PCBs) are a family of persistent organic contaminants suspected to cause Maglich et al. 2002), we infer that the metab- adverse effects in wildlife and humans. In rodents, PCBs bind to the aryl hydrocarbon (AhR) and olism of some compounds will be correspond- pregnane X receptors (PXR) inducing the expression of catabolic cytochrome p450 enzymes of the ingly different between humans and model CYP1A and 3A families. We found that certain highly chlorinated PCBs are potent activators of organisms. To test this possibility, we tested a rodent PXR but antagonize its human ortholog, the steroid and xenobiotic receptor (SXR), inhibit- variety of PCBs to determine their ability to ing target gene induction. Thus, exposure to PCBs may blunt the human xenobiotic response, activate human and rodent SXR/PXR. We inhibiting the detoxification of steroids, bioactive dietary compounds, and xenobiotics normally found that more highly chlorinated PCB con- mediated by SXR. The antagonistic PCBs are among the most stable and abundant in human tis- geners were able to activate rodent PXR but sues. These findings have important implications for understanding the biologic effects of PCB not human SXR.