Carpal Fractures and Dislocations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
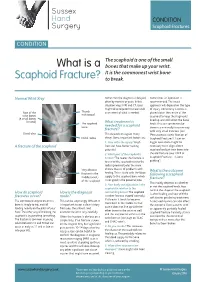
What Is a Scaphoid Fracture?
Sussex Hand CONDITION Surgery Scaphoid Fractures CONDITION The scaphoid is one of the small What is a bones that make up your wrist. It is the commonest wrist bone Scaphoid Fracture? to break. Normal Wrist Xray Sometimes the diagnosis is delayed, Sometimes an operation is often by months or years. In this recommended. The exact situation xrays, MRI and CT scans approach will depend on the type might all be required to make a full of injury. Commonly a screw is Rest of the Thumb assessment of what is needed. placed down the centre of the metacarpal wrist bones scaphoid to keep the fragments (8 small bones lined up and still whilst the bone in total) The scaphoid What treatment is heals. This can sometimes be bone needed for a scaphoid done in a minimally invasive way fracture? with very small incisions (see Distal ulna This depends on a great many ‘Percutaneous screw fixation of Distal radius things. Some important factors are: Scaphoid Fractures’). Later on 1. How old is the injury? Fresh bigger operations might be A fracture of the scaphoid fractures have better healing necessary to re-align a bent potential scaphoid and put new bone into 2. Which part of the scaphoid is the old fracture (see ‘ORIF of broken? The nearer the fracture is Scaphoid Fractures +/-bone to end of the scaphoid next to the grafting’). radius (proximal pole) the more Very obvious chance there is of problems with What is the outcome fracture in the healing. This is to do with the blood following a scaphoid middle (waist) supply to the scaphoid bone which fracture? of the scaphoid is not good in the proximal pole. -

Table 9-10 Ligaments of the Wrist and Their Function
Function and Movement of the Hand 283 Table 9-10 Ligaments of the Wrist and Their Function Extrinsic Ligaments Function Palmar radiocarpal Volarly stabilizes radius to carpal bones; limits excessive wrist extension Dorsal radiocarpal Dorsally stabilizes radius to carpal bones; limits excessive wrist flexion Ulnar collateral Provides lateral stability of ulnar side of wrist between ulna and carpals Radial collateral Provides lateral stability of radial side of wrist between radius and carpals Ulnocarpal complex and articular Stabilizes and helps glide the ulnar side of wrist; stabilizes distal disk (or triangular fibrocartilage radioulnar joint complex) Intrinsic Ligaments Palmar midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Dorsal midcarpal Forms and stabilizes the proximal and distal rows of carpal bones Interosseous Intervenes between each carpal bone contained within its proximal or distal row Accessory Ligament Transverse carpal Stabilizes carpal arch and contents of the carpal tunnel Adapted from Hertling, D., & Kessler, R. (2006). Management of common musculoskeletal disorders: Physical therapy principles and methods. Philadelphia, PA: Lippincott, Williams & Wilkins.; Oatis, C. A. (2004). Kinesiology: The mechanics and pathomechanics of human movement. Philadelphia, PA: Lippincott, Williams & Wilkins.; Weiss, S., & Falkenstein, N. (2005). Hand rehabilitation: A quick reference guide and review. St. Louis, MO: Mosby Elsevier. The radial and ulnar collateral ligaments provide lateral and medial support, respectively, to the wrist joint. The ulnocarpal complex is more likely to be referred to as the triangular fibro- cartilage complex (TFCC) and includes the articular disk of the wrist. The TFCC is the major stabilizer of the distal radioulnar joint (DRUJ) and can tear after direct compressive force such as a fall on an outstretched hand. -

Carpals and Tarsals of Mule Deer, Black Bear and Human: an Osteology Guide for the Archaeologist
Western Washington University Western CEDAR WWU Graduate School Collection WWU Graduate and Undergraduate Scholarship 2009 Carpals and tarsals of mule deer, black bear and human: an osteology guide for the archaeologist Tamela S. Smart Western Washington University Follow this and additional works at: https://cedar.wwu.edu/wwuet Part of the Anthropology Commons Recommended Citation Smart, Tamela S., "Carpals and tarsals of mule deer, black bear and human: an osteology guide for the archaeologist" (2009). WWU Graduate School Collection. 19. https://cedar.wwu.edu/wwuet/19 This Masters Thesis is brought to you for free and open access by the WWU Graduate and Undergraduate Scholarship at Western CEDAR. It has been accepted for inclusion in WWU Graduate School Collection by an authorized administrator of Western CEDAR. For more information, please contact [email protected]. MASTER'S THESIS In presenting this thesis in partial fulfillment of the requirements for a master's degree at Western Washington University, I grant to Western Washington University the non-exclusive royalty-free right to archive, reproduce, distribute, and display the thesis in any and all forms, including electronic format, via any digital library mechanisms maintained by WWu. I represent and warrant this is my original work, and does not infringe or violate any rights of others. I warrant that I have obtained written permissions from the owner of any third party copyrighted material included in these files. I acknowledge that I retain ownership rights to the copyright of this work, including but not limited to the right to use all or part of this work in future works, such as articles or books. -

Upper Limb Fractures in Rugby in Huddersfield 1986- 1 990
Br J Sp Med 1991; 25(3) From the Clinic Br J Sports Med: first published as 10.1136/bjsm.25.3.139 on 1 September 1991. Downloaded from Upper limb fractures in rugby in Huddersfield 1986- 1 990 K.S. Eyres FRCS', A. Abdel-Salam FRCS2 and J. Cleary FRCS3 Research Registrar, Department of Human Metabolism and Clinical Biochemistry, University of Sheffield, Sheffield, UK 2 Orthopaedic Registrar, Huddersfield Royal Infirmary, Huddersfield, UK 3 Orthopaedic Consultant, Huddersfield Royal Infirmary, Huddersfield, UK Most injuries sustained by rugby players affect the soft Case 1 tissues, and fracture is relatively uncommon. Whereas the lower limb is most affected in footballers, the upper limb A 24-year-old full-back fractured his left clavicle in a tends to be injured in rugby players. Thirty consecutive scrummage in 1988 (Figure 1). Six months later, he fractures and ten dislocations affecting the upper limb, sustained a direct blow to the left shoulder. Radio- sustained by 35 rugby players, are reported. graphs showed a fracture to the greater tuberosity of the left humerus (Figure 2). He was treated with a Keywords: Rugby injury, hamate fracture, sports injury collar and cuff and was able to return to matchplay after 2 months. Nine months later he fell onto his left hand after a tackle. Radiographs showed a sagittal Most injuries sustained in rugby matches are to the fracture of the body of the hamate and a fracture of soft tissues. Fractures are relatively uncommon, the base of the fourth metacarpal (Figure 3). He was estimated to account for only 4% of injuries in adult treated conservatively with plaster immobilization, matches and for 5% of injuries in school matches'. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

Radiohamate Impingement After Proximal Row Carpectomy ‘Radiohamate Impingement PRC’
Acta Orthop. Belg., 2020, 86 e-supplement 1, 19-21 CASE REPORT Radiohamate impingement after proximal row carpectomy ‘Radiohamate impingement PRC’ Pieter Caekebeke, Luc De Smet From the Department of Orthopaedics UZ Leuven, Pellenberg, Belgium Radiocarpal impingement after PRC is a well-known from 0% to 18% (5). Radiocarpal and pisiform complication due to impingement of the radial styloid impingement have been described after PRC. The against the radial carpal bones. A less common first is probably due to the proximalization of the impingement syndrome is that of the pisiforme. distal row with impingement of the trapezium/ We describe a radiohamate impingement and its trapezoid against the radial styloid process. The diagnosis and treatment. Based on a case we saw treatment is a radial styloid process resection for at our practice. Diagnosis is bases on standard radiographs and SPECT-CT. The treatment is the first and a pisiformectomy for the latter (3,5). No initially conservative. Surgery is necessary when other impingement syndromes have been described. conservative treatment fails and consists of resectie We present a case of radiohamate impingement of the proximal pole of the hamate. syndrome after proximal row carpectomy. Keywords: Radiohamate ; impingement ; proximal row CASE REPORT carpectomy. A 53-year-old mechanic contacted us 1 year after a work-accident with localized radiocarpal INTRODUCTION pain and swelling. Radiographs showed a stage Proximal row carpectomy (PRC) is a well- two SLAC wrist. (Fig. 1) A PRC with synovectomy established motion-preserving salvage procedure was performed. The following 3 years were for degenerative disorders of the proximal carpal uneventful with no to minimal pain complaints. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -

The Muscles That Act on the Upper Limb Fall Into Four Groups
MUSCLES OF THE APPENDICULAR SKELETON UPPER LIMB The muscles that act on the upper limb fall into four groups: those that stabilize the pectoral girdle, those that move the arm, those that move the forearm, and those that move the wrist, hand, and fingers. Muscles Stabilizing Pectoral Girdle (Marieb / Hoehn – Chapter 10; Pgs. 346 – 349; Figure 1) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: ANTERIOR THORAX: anterior surface coracoid process protracts & depresses Pectoralis minor* pectoral nerves of ribs 3 – 5 of scapula scapula medial border rotates scapula Serratus anterior* ribs 1 – 8 long thoracic nerve of scapula laterally inferior surface stabilizes / depresses Subclavius* rib 1 --------------- of clavicle pectoral girdle POSTERIOR THORAX: occipital bone / acromion / spine of stabilizes / elevates / accessory nerve Trapezius* spinous processes scapula; lateral third retracts / rotates (cranial nerve XI) of C7 – T12 of clavicle scapula transverse processes upper medial border elevates / adducts Levator scapulae* dorsal scapular nerve of C1 – C4 of scapula scapula Rhomboids* spinous processes medial border adducts / rotates dorsal scapular nerve (major / minor) of C7 – T5 of scapula scapula * Need to be familiar with on both ADAM and the human cadaver Figure 1: Muscles stabilizing pectoral girdle, posterior and anterior views 2 BI 334 – Advanced Human Anatomy and Physiology Western Oregon University Muscles Moving Arm (Marieb / Hoehn – Chapter 10; Pgs. 350 – 352; Figure 2) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: intertubercular -

The Structure and Movement of Clarinet Playing D.M.A
The Structure and Movement of Clarinet Playing D.M.A. DOCUMENT Presented in Partial Fulfilment of the Requirements for the Degree Doctor of Musical Arts in the Graduate School of The Ohio State University By Sheri Lynn Rolf, M.D. Graduate Program in Music The Ohio State University 2018 D.M.A. Document Committee: Dr. Caroline A. Hartig, Chair Dr. David Hedgecoth Professor Katherine Borst Jones Dr. Scott McCoy Copyrighted by Sheri Lynn Rolf, M.D. 2018 Abstract The clarinet is a complex instrument that blends wood, metal, and air to create some of the world’s most beautiful sounds. Its most intricate component, however, is the human who is playing it. While the clarinet has 24 tone holes and 17 or 18 keys, the human body has 205 bones, around 700 muscles, and nearly 45 miles of nerves. A seemingly endless number of exercises and etudes are available to improve technique, but almost no one comments on how to best use the body in order to utilize these studies to maximum effect while preventing injury. The purpose of this study is to elucidate the interactions of the clarinet with the body of the person playing it. Emphasis will be placed upon the musculoskeletal system, recognizing that playing the clarinet is an activity that ultimately involves the entire body. Aspects of the skeletal system as they relate to playing the clarinet will be described, beginning with the axial skeleton. The extremities and their musculoskeletal relationships to the clarinet will then be discussed. The muscles responsible for the fine coordinated movements required for successful performance on the clarinet will be described. -

Scaphoid Fracture PA Radiograph
30 y/o male with acute left wrist pain Student Name….None was listed Atul Kumar, MD, MS PA Radiograph Non Contrast Coronal CT ? Scaphoid Fracture PA radiograph Distal pole Scaphoid fracture Proximal pole • PA x-ray showing transverse scaphoid fracture. Non Contrast Coronal CT Capitate Trapezoid Hamate Trapezium Triquetrum Lunate Scaphoid fracture Scaphoid Fracture • Mechanism: direct axial compression or with hyperextension (fall onto an outstretched hand). • Symptoms: pain localized at the radial aspect of wrist often associated with swelling and reduced grip strength. – Pain in anatomic snuffbox suspicious for waist fracture, which is the most common type. • Because scaphoid fractures are often radiologically occult, any tenderness in the anatomic snuffbox should be treated as a scaphoid fracture. • Scaphoid blood supply (palmar carpal branch of the radial artery) runs from the distal to the proximal pole. Transverse fracture of the proximal pole can lead to osteonecrosis and nonunion due to disruption of blood flow. http://epmonthly.com/wp-content/uploads/2016/04/OrthoB.png Scaphoid Fracture • Differential diagnosis: distal radius fracture, wrist sprain, and other carpal injuries other than scaphoid. • In suspected scaphoid fractures, plain radiographs (including PA, true lateral, oblique, and scaphoid views) are ordered as the first diagnostic step. • However, the false negative rate for radiographs taken immediately after injury up to 20-54%. • Definitive diagnosis can be made by MRI or CT scan. They have a comparable diagnostic accuracy and do not result in overtreatments. Avascular necrosis/Nonunion Scaphoid view radiograph (A) and CT scan (B) showing nonunion (arrow) and avascular necrosis (asterisk) and the Terry Thomas sign – scapholunate ligament injury (arrowhead). -

Fractures of Hamate: a Clinical Overview
MUSCULOSKELETAL SURGERY (2019) 103:15–21 https://doi.org/10.1007/s12306-018-0543-y REVIEW Fractures of hamate: a clinical overview G. Mouzopoulos1 · C. Vlachos1 · L. Karantzalis1 · K. Vlachos1 Received: 28 June 2017 / Accepted: 20 May 2018 / Published online: 29 May 2018 © Istituto Ortopedico Rizzoli 2018 Abstract Hamate fractures are exceedingly rare clinical entities. However, the diagnosis and treatment of these injuries are often delayed and can severely handicap the performance of afected laborers or athletes. This review focuses on fractures of the hamate and provides an update on the current consensus as to mechanism, diagnosis, management, and complications after such injuries. Keywords Hamate · Hook · Fracture Epidemiology the hook of the hamate [2]. If the grip is relaxed or control is lost, the fracture occurs at the end of a poor swing, as Fractures of the hamate usually occur through the hook centrifugal force is transmitted through the handle of the or body of the bone [1]. Type I fractures involve the hook racquet against the hook [7]. In golfers or baseball players, of the hamate and further are subdivided into three sub- a dubbed shot or a checked swing will fracture the hamulus types involving: base, waist, and avulsion (tip). Fractures because the butt of the club or bat will strike the hook. It has located at the base and proximal third (76%) of the hook also been described in polo and ice hockey [8]. are presented more frequently than fractures located at the Fall on an outstretched hand causing sudden forcible mid-third (13%) or the distal third (11%).