The Diagnostic Value of Skin Biopsies Francis A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(ERYTHEMA NODOSUM LEPROSUM) the Term
? THE HISTOPATHOLOGY OF ACUTE PANNICULITIS NODOSA LEPROSA (ERYTHEMA NODOSUM LEPROSUM) w. J. PEPLER, M.B., Ch.B. Department of Pathology, South African Institute for Medical Research, Johannesburg R. KOOIJ, M.D. Westfort Institution, Pretoria AND J. MARSHALL, M.D. University of Pretoria, Pretoria The term "erythema nodosum leprosum" has frequently appeared in the literature on leprosy since the 1930's, apparently popularized by the Japanese (9). The occurrence of "erythema nodosum" in leprosy had previously been noted at the end of the nineteenth century by Brocq (6) and by Hansen and Looft (8), but the term seems to have fallen into disuse. As will become clear from our clinical and histological descriptions of the phenomenon commonly known as erythema nodosum leprosum, we believe the title to be a misnomer. We suggest that it would be more accurate to call it panniculitis nodosa leprosa (P.N.L,). This condition is commonly confused with acute lepra reaction, both processes being referred to as "acute reactions"; but a sharp line of distinction must be drawn between them. P.N.L. occurs only in patients with lepromatous leprosy as an acute, subacute or chronic skin eruption, with or without fever. It is characterized by showers of dusky red nodules, 0.5 to 2 cm. in diameter, on the extensor surfaces of the limbs, on the face, and, less often, on the trunk. The number of lesions appearing in an attack varies from a few to several hundreds, and they sometimes coalesce to form plaques. The nodules may be painful, and they are usually tender to touch. -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

Pattern of Cutaneous Tuberculosis Among Children and Adolescent
Bangladesh Med Res Counc Bull 2012; 38: 94-97 Pattern of cutaneous tuberculosis among children and adolescent Sultana A1, Bhuiyan MSI1, Haque A2, Bashar A3, Islam MT4, Rahman MM5 1Dept. of Dermatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, 2Dept. of Public health and informatics, BSMMU, Dhaka, 3SK Hospital, Mymensingh Medical College, Mymensingh, 4Dept. of Physical Medicine and Rehabilitation, BSMMU, Dhaka, 5Dept. of Dermatology, National Medical College, Dhaka. Email: [email protected] Abstract Cutaneous tuberculosis is one of the most subtle and difficult diagnoses for dermatologists practicing in developing countries. It has widely varied manifestations and it is important to know the spectrum of manifestations in children and adolescent. Sixty cases (age<19 years) of cutaneous tuberculosis were included in this one period study. The diagnosis was based on clinical examination, tuberculin reaction, histopathology, and response to antitubercular therapy. Histopahology revealed 38.3% had skin tuberculosis and 61.7% had diseases other than tuberculosis. Among 23 histopathologically proved cutaneous tuberculosis, 47.8% had scrofuloderma, 34.8% had lupus vulgaris and 17.4% had tuberculosis verrucosa cutis (TVC). Most common site for scrofuloderma lesions was neck and that for lupus vulgaris and TVC was lower limb. Cutaneous tuberculosis in children continues to be an important cause of morbidity, there is a high likelihood of internal involvement, especially in patients with scrofuloderma. A search is required for more sensitive, economic diagnostic tools. Introduction of Child Health (BICH) and Institute of Diseases of Tuberculosis (TB), an ancient disease has affected Chest and Hospital (IDCH) from January to humankind for more than 4,000 years1 and its December 2010. -

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -

Pediatric and Adolescent Dermatology
Pediatric and adolescent dermatology Management and referral guidelines ICD-10 guide • Acne: L70.0 acne vulgaris; L70.1 acne conglobata; • Molluscum contagiosum: B08.1 L70.4 infantile acne; L70.5 acne excoriae; L70.8 • Nevi (moles): Start with D22 and rest depends other acne; or L70.9 acne unspecified on site • Alopecia areata: L63 alopecia; L63.0 alopecia • Onychomycosis (nail fungus): B35.1 (capitis) totalis; L63.1 alopecia universalis; L63.8 other alopecia areata; or L63.9 alopecia areata • Psoriasis: L40.0 plaque; L40.1 generalized unspecified pustular psoriasis; L40.3 palmoplantar pustulosis; L40.4 guttate; L40.54 psoriatic juvenile • Atopic dermatitis (eczema): L20.82 flexural; arthropathy; L40.8 other psoriasis; or L40.9 L20.83 infantile; L20.89 other atopic dermatitis; or psoriasis unspecified L20.9 atopic dermatitis unspecified • Scabies: B86 • Hemangioma of infancy: D18 hemangioma and lymphangioma any site; D18.0 hemangioma; • Seborrheic dermatitis: L21.0 capitis; L21.1 infantile; D18.00 hemangioma unspecified site; D18.01 L21.8 other seborrheic dermatitis; or L21.9 hemangioma of skin and subcutaneous tissue; seborrheic dermatitis unspecified D18.02 hemangioma of intracranial structures; • Tinea capitis: B35.0 D18.03 hemangioma of intraabdominal structures; or D18.09 hemangioma of other sites • Tinea versicolor: B36.0 • Hyperhidrosis: R61 generalized hyperhidrosis; • Vitiligo: L80 L74.5 focal hyperhidrosis; L74.51 primary focal • Warts: B07.0 verruca plantaris; B07.8 verruca hyperhidrosis, rest depends on site; L74.52 vulgaris (common warts); B07.9 viral wart secondary focal hyperhidrosis unspecified; or A63.0 anogenital warts • Keratosis pilaris: L85.8 other specified epidermal thickening 1 Acne Treatment basics • Tretinoin 0.025% or 0.05% cream • Education: Medications often take weeks to work AND and the patient’s skin may get “worse” (dry and red) • Clindamycin-benzoyl peroxide 1%-5% gel in the before it gets better. -
Erythema Ab Igne and Use of Laptop Computers
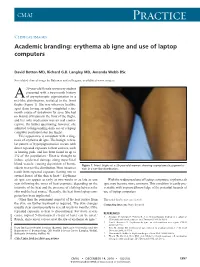
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital
ﺑﺴﻢ اﷲ اﻟﺮﺣﻤﻦ اﻟﺮﺣﻴﻢ Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital A thesis submitted in the partial fulfillment of the degree of clinical MD in pediatrics and child health University of Khartoum By DR. AMNA ABDEL KHALIG MOHAMED ATTAR MBBS University of Khartoum Supervisor PROF. SALAH AHMED IBRAHIM MD, FRCP, FRCPCH Department of Pediatrics and Child Health University of Khartoum University of Khartoum The Graduate College Medical and Health Studies Board 2008 Dedication I dedicate my study to the Department of Pediatrics University of Khartoum hoping to be a true addition to neonatal care practice in Sudan. i Acknowledgment I would like to express my gratitude to my supervisor Prof. Salah Ahmed Ibrahim, Professor of Peadiatric and Child Health, who encouraged me throughout the study and provided me with advice and support. I am also grateful to Dr. Osman Suleiman Al-Khalifa, the Dermatologist for his support at the start of the study. Special thanks to the staff at Omdurman Maternity Hospital for their support. I am also grateful to all mothers and newborns without their participation and cooperation this study could not be possible. Love and appreciation to my family for their support, drive and kindness. ii Table of contents Dedication i Acknowledgement ii Table of contents iii English Abstract vii Arabic abstract ix List of abbreviations xi List of tables xiii List of figures xiv Chapter One: Introduction & Literature Review 1.1 The skin of NB 1 1.2 Traumatic lesions 5 1.3 Desquamation 8 1.4 Lanugo hair 9 1.5 -

Approach to Elephantiasis Nostra of Unclear Etiology: a Case Report with a Brief Review
Journal of Phebology and Lymphology Approach to Elephantiasis Nostra of Unclear Etiology: A Case Report with a Brief Review Authors: Hamit Serdar BAŞBUĞ, Macit BİTARGİ, Kanat ÖZIŞIK Affiliation: Kafkas University Faculty of Medicine, Department of Cardiovascular Surgery, Kars, TURKEY Adress: 1Physiotherapist, Post Graduate Lato Sensu Course on Lymphovenous Rehabilitation of the Medical School in São José do Rio Preto‐FAMERP‐ Rua Tursa 1442 ,apto 201‐ Barroca ‐ Belo Horizonte‐Minas Gerais‐Brazil‐Cep 30431‐091 E‐mail: [email protected]*corresponding author Published: April 2015 Received: January 2015 Journal Phlebology and Lymphology 2015; 8:1‐5 Accepted: 20 March 2015 Abstract Lower extremity lymphedema is an important clinical condition causing morbidity and is frequently encountered by the phlebologists. Elephantiasis Nostra is the status characterized with the extraordinary massive swelling of one or both legs with subsequent thickening and fibrosis of the overlying skin. It is an exaggerated manifestation of a longstanding chronic lymphedema. Etiologically, secondary lymphedema is caused by an external effect such as a chronic lymphangitis, removal of the lymph nodes, trauma, mechanical obstruction, radiotherapy, venous insufficiency, obesity, heart failure, bacterial or helminthic infection (Lymphatic Filariasis), in contrary to the primary lymphedema in which an inherent malfunction of lymphatic channels exists. A morbidly obese female patient with a bilateral Elephantiasis Nostra and our effort on setting the etiological definition and the treatment approach is presented. Key words: Lymphoedema; obesity; leg ulcers Introduction Elephantiasis is the end result of lymphogranuloma Elephantiasis is a progressive enlargement of an extremity venereum, and lastly the Proteus Syndrome which is an 4 or body part accompanied by a chronic inflammatory genetic disorder widely called as "Elephant Man" . -

Tinea Capitis 2014 L.C
BJD GUIDELINES British Journal of Dermatology British Association of Dermatologists’ guidelines for the management of tinea capitis 2014 L.C. Fuller,1 R.C. Barton,2 M.F. Mohd Mustapa,3 L.E. Proudfoot,4 S.P. Punjabi5 and E.M. Higgins6 1Department of Dermatology, Chelsea & Westminster Hospital, Fulham Road, London SW10 9NH, U.K. 2Department of Microbiology, Leeds General Infirmary, Leeds LS1 3EX, U.K. 3British Association of Dermatologists, Willan House, 4 Fitzroy Square, London W1T 5HQ, U.K. 4St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, U.K. 5Department of Dermatology, Hammersmith Hospital, 150 Du Cane Road, London W12 0HS, U.K. 6Department of Dermatology, King’s College Hospital, Denmark Hill, London SE5 9RS, U.K. 1.0 Purpose and scope Correspondence Claire Fuller. The overall objective of this guideline is to provide up-to- E-mail: [email protected] date, evidence-based recommendations for the management of tinea capitis. This document aims to update and expand Accepted for publication on the previous guidelines by (i) offering an appraisal of 8 June 2014 all relevant literature since January 1999, focusing on any key developments; (ii) addressing important, practical clini- Funding sources cal questions relating to the primary guideline objective, i.e. None. accurate diagnosis and identification of cases; suitable treat- ment to minimize duration of disease, discomfort and scar- Conflicts of interest ring; and limiting spread among other members of the L.C.F. has received sponsorship to attend conferences from Almirall, Janssen and LEO Pharma (nonspecific); has acted as a consultant for Alliance Pharma (nonspe- community; (iii) providing guideline recommendations and, cific); and has legal representation for L’Oreal U.K. -

Atypical Variants of Mycosis Fungoides
Altınışık et al. Atypical Variants of Mycosis Fungoides REVIEW DOI: 10.4274/jtad.galenos.2021.09719 J Turk Acad Dermatol 2021;15(2):30-33 Atypical Variants of Mycosis Fungoides Dursun Dorukhan Altınışık, Özge Aşkın, Tuğba Kevser Uzunçakmak, Burhan Engin Istanbul University-Cerrahpasa, Cerrahpasa Faculty of Medicine, Department of Dermatology, Istanbul, Turkey ABSTRACT Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL) and it is characterised by specific histological features. MF is in a spectrum of disorders which includes Sezary syndrome and other CTCL subtypes. Clinically and histopathologically it can imitate other T-cell mediated dermatosis hence making its diagnosis difficult. Due to different prognosis and difference in treatment strategies other subtypes of CTCL must be differentiated from MF. MF is a clinically indolent low-grade lymphoma which is seen in people aged between 55- 60 and it’s seen more commonly in men (2:1 ratio). Meanwhile other subtypes of MF like folliculotropic variant may show relatively a more aggressive course and our treatment strategy may differ. Keywords: Mycosis fungoides, Cutaneous T-cell lymphoma, Phototherapy, PUVA Introduction follicles frequently causing alopecia and in the paediatric population Mycosis fungoides (MF) is the most common type of cutaneous T-cell it tends to accompany hypopigmented patches and plaques. FMF lymphoma (CTCL) and it is characterised by specific histological preferentially involves the head and neck region however it can features [1]. MF is in a spectrum of disorders which includes Sezary sometimes involve the trunk or the extremities [6]. Patients with syndrome and other CTCL subtypes. Clinically and histopathologically FMF have significant pruritus which may be overlapped by S.