Insrt Image Looking Beyond the Symptoms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Changes to Bus Services in Brighton and Hove the Following Changes To
Changes to Bus Services in Brighton and Hove The following changes to bus services will take place in September 2018 c Route details Changes to current service Service provided Date of by change 1 Whitehawk - County Hospital On Saturday mornings the combined westbound service 1/1A frequency Brighton & Hove 16.09.18 - City Centre - Hove - will be slightly reduced between approximately 7am and 8am – from Buses Portslade – Valley Road - every 10 minutes to every 12 or 13 minutes. Mile Oak On Sunday mornings, the first three eastbound journeys will additionally serve Brighton Station. The journeys concerned are the 6.29am and 6.59am from New Church Road/Boundary Road, and the 7.14am from Mile Oak. 1A Whitehawk - County Hospital Please see service 1, above. Brighton & Hove 16.09.18 - City Centre - Hove - Buses Portslade – Mile Oak Road - Mile Oak N1 (night Whitehawk - County Hospital No change Brighton & Hove bus) - City Centre - Hove - Buses Portslade - Mile Oak - Downs Park - Portslade 2 Rottingdean - Woodingdean - Some early morning and early evening journeys that currently terminate Brighton & Hove 16.09.18 Sutherland Road - City at Shoreham High Street will be extended to start from or continue to Old Buses Centre - Hove - Portslade - Shoreham, Red Lion. Shoreham - Steyning On Saturdays, the 7.03am journey from Steyning will instead start from Old Shoreham, Red Lion, at 7.20am. 2B Hove - Old Shoreham Road - Minor timetable changes Brighton & Hove 16.09.18 Steyning Buses Date of Service No. Route details Changes to current service Service provided by Change 5 Hangleton - Grenadier – Elm On Sundays, there will be earlier buses. -

Property Brochure 1
PORTSLADE 1 OAK POINT PORTSLADE LIFE, AS IT SHOULD BE Oak Point is a new neighbourhood designed with first time buyers in mind. Where Portslade-by-Sea meets the South Downs, between Brighton, Hove and Shoreham, these two, three and four bedroom homes are all available through Shared Ownership. Homes of lasting quality, ideally suited to everyday modern living: space with light, and room to grow. Computer generated image is indicative only 2 3 OAK POINT PORTSLADE LIVING, HOW IT OUGHT TO BE Convenient, connected, and just around the corner. Shops, schools, coffee; it’s the everyday made easy. Stroll or scoot to doctors, dentists, the essence of community, and the lasting quality of local life. Discover a place of wellbeing, within reach of woods and waves, between town and country. Find your lifetime home to create new memories. Brought to you through Shared Ownership by Clarion. 4 5 OAK POINT PORTSLADE 6 7 OAK POINT PORTSLADE SHOPPING & OTHER AMENITIES 1 North Laine Bazaar LOCAL AREA MAP A27 2 Holmbush Shopping Centre 3 Hangleton Manor 4 The Schooner NORTH 5 The Coal Shed 6 Rotunda Café Churchill Square 7 4 D d Shopping Centre 5 y a k o A27 e R R o g a n d i l A v h 4 c 8 L d e 1 3 t 6 n o i 0 a 2 u n D o e A d R o n 2 7 3 l l i v R e o a N d 0 6 S 7 8 2 03 h A2 A i r l e d Shoreham-By-Sea y a D o R r i PRESTON s v e e 270 A D PARK w e y L k e PORTSLADE S R a o R oad c a d k n v 6 re i r l e a l v W i R Elm r Grove o D a 1 e d Kin g 3 h sw T 4 ay 2 5 HOVE Royal Pavilion Hove Lawns 3 7 Brighton City Airport 5 2 BRIGHTON British Airways i360 SPORTS & ACTIVITIES KEMPTOWN FUN FOR ALL 1 1 Brighton Footgolf 1 SEA LIFE Brighton 2 Lagoon Watersports 2 LaserZone Brighton Palace Pier 3 King Alfred Leisure Centre ENGLISH CHANNEL 3 Hove Museum & Art Gallery 4 Benfield Hill Local Nature Reserve 4 Foredown Tower 5 West Hove Golf Club 5 ODEON West Blatchington Windmill 6 Mile Oak Football Club 6 (Grade II* listed) 7 Portslade Sports Centre Brighton Marina 8 9 OAK POINT PORTSLADE FAMILY FUN A run with little ones away to swings, swims and parks, themed for larks. -

Changes to Bus Services in Brighton and Hove the Following Changes to Bus Services Will Take Place in January 2018
Changes to Bus Services in Brighton and Hove The following changes to bus services will take place in January 2018 Service No. Route details Changes to current service Service provided Date of by change 1 Whitehawk - County The combined service 1/1A evening frequency will be improved - from Brighton & Hove 14.01.18 Hospital - City Centre - every 15 minutes to every 12 minutes - for most of the evening on Buses Hove - Portslade – Valley Mondays to Saturdays. There will be an additional morning commuter Road - Mile Oak journey on service 1 from Whitehawk to Mile Oak, Monday to Friday - plus an additional journey at 7.29am from Hove Town Hall to Mile Oak on schooldays. 1A Whitehawk - County Please see service 1, above. Brighton & Hove 14.01.18 Hospital - City Centre - Buses Hove - Portslade – Mile Oak Road - Mile Oak N1 (night Whitehawk - County Night Bus N1 will be revised to operate westbound only, from Brighton Brighton & Hove 14.01.18 bus) Hospital - City Centre - Station, then via Churchill Square and the current N1 route to Mile Oak Buses Hove - Portslade - Mile and Downs Park. There will be no eastbound journeys. Oak - Downs Park The section of route from Churchill Square to Whitehawk will be withdrawn. Service N7 provides an alternative between the city centre and Kemp Town (Roedean Road/Arundel Road). On Monday to Saturday nights, the revised N1 will leave Brighton Station at 12.40am, then every 30 minutes until 3.10am, then 4.10am. On Sunday nights buses leave Brighton Station at 12.40am, 1.40am and 2.40am. -

Your Local Support
Your local support Community Support Newsletter Covid-19 Your local emergency food hubs The Food Partnership is working with The Purple People Kitchen, The Hangleton and Knoll Brighton & Hove City Council project, The Hangleton & West Blatchington foodbank and Extra Time to arrange food aid distribution. Please see contact details on the front page for Community Support Hub. Support is available, COVID-19 Community Transport Food Delivery Service: you are not alone Community Support Hub Service for anyone in the city who needs food and basic supplies. In partnership with local Hello, this newsletter is to give you If you can’t find what you need in these pages independent grocer. Deliveries in Hangleton, Portslade & Mile Oak on Tuesdays & Fridays. information about the various services and and need extra help accessing essential Residents can order online on the website food.bhct.co.uk or by calling Community Transport support that is available for all residents services and supplies 9am-5pm Ellis: 07548 226452 or Daniel: 07739 953600. across Brighton West — covering Where possible please use the online, easy to Hangleton & Knoll, North Portslade and use form, or fill it in on behalf of someone Other local groups South Portslade communities. else, so we can keep phone lines free for Hangleton & Knoll Project website: www.hkproject.org.uk those with no alternative. The following Covid19 Mutual Aid groups can be found on Facebook or WhatsApp: Hangleton; Go to: new.brighton-hove.gov.uk/ Portslade and Mile Oak; Portslade and West Hove; Southern Cross. Find links to join them coronavirus-covid-19/request-help here www.brightonmutualaid.co.uk/local-groups Your West Support Team Struggling to access information If you can’t get online, you can call: The following local groups can be found by searching on Facebook: online? Not enough data allowance, 01273 293117 Portslade and Mile Oak Forum; Buzz on Boundary. -

FINAL Sussex Wildlife Trust Response to City Plan Part Two Reg 19 Oct2020
Contact: Jess Price E-mail: [email protected] Date: 29 October 20 By email only planningpolicy@brighton -hove.gov.uk Brighton & Hove City Council’s Development Plan April 2020 - Proposed Submission City Plan Part Two The Sussex Wildlife Trust recognises the importance of a plan led system as opposed to a developer led process and supports Brighton & Hove City Council’s (BHCC) desire to produce part 2 of their City Plan. We hope that our comments to this Regulation 19 consultation are used constructively to make certain that the plan properly plans for the natural capital needed within the city and ensures that any development is truly sustainable. Please find attatched our response within BHCC’s word document response form. We have made comments in the following sections: Section A – Your details Section C – Representations on policies DM1 – DM46, SA7, SSA1 to SSA7 DM22 – support DM32 – support DM37 – objection DM38 – objection DM39 – support DM40 – support DM42 – support Special Area SA7 – objection SSA1 – objection Section D – H1 Housing Sites and Mixed Use Sites – Objection Section E – H2 Housing Sites – Urban Fringe – Objection We have also included an Appendix – Appendix A. The Sussex Wildlife Trust wishes to participate in any examination hearings sessions relevant to any sections of the City Plan Part Two that we have submitted objections to. We wish to discuss our objections formally with the Inspector and respond to any additional evidence presented by other respondents. Yours sincerely Jess Price Conservation Officer Sussex Wildlife Trust City Plan Part Two - Proposed Submission Response Form (7 September – 30 October 2020) Please Note Policies in the Proposed Submission City Plan Part Two were agreed at Full Council on 23 April 2020. -

Housing Provision Paper
Housing Provision May 2018 SCAPE Carden Avenue and Norton Road pilot projects ITT exhibition feedback report 0 Contents 1. Introduction ........................................................................................................................ 1 2. Background ......................................................................................................................... 2 b) Updated information on housing land supply ................................................................ 3 c) Site allocations in City Plan Part Two .............................................................................. 4 3. Assessment of Housing Delivery against the City Plan Target ........................................... 5 a) Large Identified Sites (6+ dwellings) in Development Areas .......................................... 5 b) Large Identified Sites (6+ dwellings) in the Rest of the City ........................................... 6 c) Small Sites (5 or less dwellings) ...................................................................................... 7 d) Other Sources of Housing Supply ................................................................................... 7 e) Housing supply summary ................................................................................................ 8 4. Conclusion .......................................................................................................................... 9 Appendices Appendix 1: City Plan Part 2 Housing delivery against City Plan targets Appendix -

71A Bus Time Schedule & Line Route
71A bus time schedule & line map 71A Portslade Academy - Hangleton - Hove - Brighton View In Website Mode The 71A bus line Portslade Academy - Hangleton - Hove - Brighton has one route. For regular weekdays, their operation hours are: (1) Mile Oak: 7:16 AM Use the Moovit App to ƒnd the closest 71A bus station near you and ƒnd out when is the next 71A bus arriving. Direction: Mile Oak 71A bus Time Schedule 53 stops Mile Oak Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:16 AM Swanborough Drive, Whitehawk Tuesday 7:16 AM Haybourne Road, Whitehawk Wednesday 7:16 AM Coolham Drive, Whitehawk Thursday 7:16 AM Pulborough Close, Brighton and Hove Friday 7:16 AM St Cuthmans Church, Whitehawk Whitehawk Way, Brighton and Hove Saturday Not Operational Piltdown Road, Whitehawk Community Hub, Whitehawk Selmeston Place, Brighton and Hove 71A bus Info Direction: Mile Oak St David's Hall, Whitehawk Stops: 53 Hellingly Close, Brighton and Hove Trip Duration: 58 min Line Summary: Swanborough Drive, Whitehawk, Findon Road, Whitehawk Haybourne Road, Whitehawk, Coolham Drive, Whitehawk, St Cuthmans Church, Whitehawk, Bus Garage, Whitehawk Piltdown Road, Whitehawk, Community Hub, Whitehawk, St David's Hall, Whitehawk, Findon Road, Arundel Road, Brighton Whitehawk, Bus Garage, Whitehawk, Arundel Road, Brighton, Lidl Superstore, Brighton, Sussex Square, Lidl Superstore, Brighton Kemp Town, St Mary's Hall, Kemp Town, Chesham Street, Kemp Town, County Hospital, Kemp Town, Arundel Road, Brighton and Hove College Place, Kemp Town, Upper Bedford -

Sunday April 14Th 2013
A23 A27 Ditchling A27 Road Viaduct Road R A27 New England Road 25 2 Upper LewesFalmer Road A270 Union Road LEWES ROAD A270 LONDON ROAD A23 Sunday April 14th 2013 - 9am Brighton Bypass A23 Patcham Coldean Elm Grove Ditchling The Road Level 25 Westdene A27 Terminus 4 Road A27 Hollingbury North Moulsecoomb Brighton St. Peter’s Station Dyke Withdean Church Road East MoulsecoombeTrafalgar Street A270 Place York Hollingdean A23 North Road Hangleton Preston London Mile Oak Park Road Southern Station Preston Moulsecoomb Grand Parade Queens Queens Park Road Portslade Jubilee Street Park Village Queens Road Church 1 StreetBevendean West Blatchington New Royal Road Edward Street A270 North Street Pavilion A270 START Lewes 3 A270 London Road 25 Old Shoreham Road Road West Street 25 A270 Station St. James Street 25 Upper Rock Southwick Hove A23 A270 Old Station Steine Gardens Cross KINGS ROAD A259 Marine Parade25 5 Boundary WoodingdeanF Fishersgate Road A259 Aldrington 2625 Coast Road 16 2 FINISH F F 15 4 Madeira Drive F 21 17 Brighton F Whitehawk 20 Station Power 22 A259 Station 19 18 23 14 Portslade by Sea A259 F 3 BRIGHTON Brighton Pier 24 E 25 5 F Kemp Town HOVE West Pier (derelict) A259 26 FINISH F F BRIGHTON 12 6 Ovingdean CHURCH ROAD Brighton Pier A259 Mile Markers 11 Roedean Black Rock 7 8 Halfway Point Palmeira Square Brighton Marina WESTERN ROAD 9 Water and Toilets 10 Albany Villas Third Avenue Fourth Avenue A259 GRAND AVENUE Neville Second Avenue Coast Road First Avenue Brunswick Road First Aid 14 Adelaide Holland Road Crescent Square MONTPELIER ROAD E Lansdowne Place Waterloo Street E Entertainment HOVE LAWNS KINGSWAY A259 WesternBedford Street Square Rottingdean F Runner Fuel Preston Street Peace Statue 25 ® HOVE West Pier (derelict). -

Route 1 1A Whitehawk
Route 1 1A Whitehawk - County Hospital - City Centre - Hove - Portslade - Mile Oak Emergency timetable from Monday 13 July and every Monday to Saturday until further notice. For Sunday and Bank Holiday times see separate pdf. route 1 1 1 1A 1 1 1A 1 1 1A 1 1A 1 1A 1 1A 1 1A 1 1A 1 1A 1 1A Swanborough Drive 0455 0525 0555 0610 0625 0635 0645 0654 0702 0709 0715 0722 0728 0735 0742 0748 0754 0800 0807 0813 0819 0825 0832 0838 Whitehawk Garage 0500 0530 0600 0615 0630 0640 0650 0659 0707 0714 0721 0728 0735 0742 0749 0755 0801 0807 0814 0820 0826 0832 0839 0845 County Hospital 0504 0534 0604 0619 0634 0644 0654 0703 0711 0718 0725 0733 0740 0747 0754 0800 0806 0812 0819 0825 0831 0837 0844 0850 Old Steine (H) 0509 0539 0609 0624 0639 0649 0659 0708 0717 0725 0732 0740 0747 0754 0801 0807 0813 0819 0826 0832 0838 0844 0851 0857 Brighton Stn (C) 0513 0543 0613 0628 - - - - - - - - - - - - - - - - - - - - Churchill Sq (C) 0517 0547 0617 0632 0643 0653 0703 0713 0722 0730 0737 0745 0752 0759 0806 0812 0818 0824 0831 0837 0843 0849 0856 0902 Hove Town Hall (D) 0523 0553 0623 0639 0650 0700 0710 0720 0730 0738 0746 0754 0800 0808 0815 0821 0827 0833 0840 0846 0852 0858 0905 0911 Boundary Rd (A) 0528 0558 0628 0645 0657 0708 0718 0728 0738 0746 0754 0802 0809 0816 0823 0829 0835 0841 0848 0854 0900 0906 0913 0919 Old Village 0533 0603 0633 0651 0703 0715 0725 0735 0745 0751 0801 0809 0816 0823 0830 0836 0842 0848 0855 0901 0907 0913 0920 0926 Mile Oak Gardens - - - 0652 - - 0726 - - 0754 - 0810 - 0824 - 0837 - 0849 - 0902 - 0914 - 0927 Mile Oak -
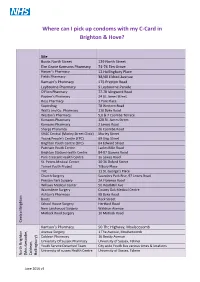
Where Can I Pick up Condoms with My C-Card in Brighton & Hove?
Where can I pick up condoms with my C-Card in Brighton & Hove? Site Boots North Street 129 North Street Elm Grove Kamsons Pharmacy 74-76 Elm Grove Harper’s Pharmacy 12 Hollingbury Place Fields Pharmacy 38/40 Eldred Avenue Kamson’s Pharmacy 175 Preston Road Leybourne Pharmacy 9 Leybourne Parade O'Flinn Pharmacy 77-78 Islingword Road Payden's Pharmacy 24 St. James Street Ross Pharmacy 3 York Place Superdrug 78 Western Road Watts and Co. Pharmacy 110 Dyke Road Weston's Pharmacy 5,6 & 7 Coombe Terrace Kamsons Pharmacy 128 St. James Street Kamsons Pharmacy 2 Lewes Road Sharps Pharamcy 26 Coombe Road SHAC Central (Morley Street Clinic) Morley Street Young People’s Centre (YPC) 69 Ship Street Brighton Youth Centre (BYC) 64 Edward Street Patcham Youth Centre Ladies Mile Road Brighton Station Health Centre 84-87 Queens Road Park Crescent Health Centre 1a Lewes Road St. Peters Medical Center 30-36 Oxford Street Tarner Youth Project Tilbury Place YAC 11 St. George’s Place Church Surgery Saunders Park Rise, 97 Lewes Road Preston Park Surgery 2A Florence Road Willows Medical Center 50 HeathHill Ave Warmdene Surgery County Oak Medical Centre Ashton’s Pharmacy 98 Dyke Road Boots Rock Street School House Surgery Hertford Road New Larchwood Surgery Waldron Avenue Matlock Road Surgery 10 Matlock Road Central Central Brighton Kamson’s Pharmacy 50 The Highway, Moulsecoomb Avenue Surgery 1 The Avenue, Moulsecoomb Coldean Pharmacy 16 Beatty Avenue University Of Sussex Pharmacy University of Sussex, Falmer Youth Service Detached Team City wide Youth Bus various -

City Centre Hove Portslade Mile Oak Downs Park Hangleton
nightbus DL mar14.qxp_nightbus99x210-8pp 20/03/2014 14:42 Page 2 These are increasingly becoming the nights to hit the town to paint and party. And why not? Brighton and Hove has such terrific Whitehawk £6 £5 to £7 to £4 Hove nightlife with bars and clubs to suit everyone, whatever your city centre £4 Rottingdean N12 now runs Hurstpierpoint the town £4 Portslade N2 £4tcham everywhere else then get home any ride Hove Saltdean every Monday Hassocks N40 style or mood. N1 Shoreham to Saturday Portslade as far as Shoreham everywhere else Worthing or Steyning as far as Saltdean Saltdean - Seaford Peacehaven as far as Pa Burgess Hill safe & sound Downs Park Newhaven N14 night red Getting home is so easy with our nightclub buses. The map Haywards Heath Mile Oak Seaford & Eastbourne* and timetables on this side show the wide range of places West Street Wetherspoons 1.30 3.05 Churchill Square stop C 1.35 3.10 you can get back to - reliably, inexpensively and safely. West Street Wetherspoons 3.05 nightclub buses Whitehawk Swanborough Drive 12.26 1.16 2.06 2.56 Hove Town Hall Tisbury Road 1.41 3.16 N 14 N 12 N 14 N 12 N 14 Blatchington Road Co-op 1.43 3.18 Churchill Square stop F 3.11 Whitehawk Bus Garage 12.30 1.20 2.10 3.00 West Street Wetherspoons 12.50 1.30 2.00 3.15 3.15 Portland Road / Olive Road 1.47 3.22 Old Steine stop D 3.14 Get partying. -

Brighton Station
d e de R c Cly D d y n R k e a H n t a R o t m d s Brighton Station x i i lt u o n S B t d anle R y Roa g d d in lk a Old Sho reham Ro w ad E ld e s Onwardr Travel Information P km e la t c e 0 0.5 Highdown Rd u n d P R i d r i n e la s ng ill m t o E H k n ew or 0 v N Y 0 0.25 i l l 1 e Buses, Taxis and Cycle Hire Miles Local area map R Addison Road d H Key l ow S J a t d P r r N u d o BC Brighton Centre R P e l m u i la w Granvil a a t c d d le Rd h e n t e l Rd e E n Melville a e BP Brighton Palace Pier r y R o h t n C S R g t d 3 m o l C Odeon Cinema e a 2 s L t e a d S n o or r f A t d O x d O n F S d CS Churchill Square Shoppingr Centre l S e e Buckingham Place o t v e r n o Rd e d t D Goldsmi St The Dome n n R D e An 0 a av S 7 igd T t o H o t r e 2 Rd r r a IT British Airways i360 Tower m e A d h i e S t n Brighton Station a u t RP B e s A Royal Pavilion u n R 2 e 3 v o SL Sea Life Centre a The e A c n d Level a to Cycle routes r t S r p o e S u m T o th n C n Footpathso o o v t e n f r i r e l S V Brighton Ch C eapside tr Station ee t t S t e n u P S o i n Wes e n e t Hill Road t e l a v v h t a A a h S rk m w o d e t Guildfo Y R rd R S N d Y S n t o e to A V v if t r a d l Albert Rd k r e g C a B e l e P c e r o r r t l B t a R C A a e St l S S E T c T ra falg P y a e m y r Peters e k Al s r e d b C a l S r a r H tre Church io e n e l h r t if P n J t o m o g u H t n k i n D n t l D S m l e H i c S y i S i h ll k D r k n D c c e p d i e o u d i t R m R t b l R B e l S l i CS r e s S i o A H F K y w a y e d RP o d i e v T n o