Nutrition and Mortality Survey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sindh Flood 2011 - Union Council Ranking - Sanghar District
PAKISTAN - Sindh Flood 2011 - Union Council Ranking - Sanghar District Union council ranking exercise, coordinated by UNOCHA and UNDP, is a joint effort of Government and humanitarian partners Community Restoration Food Education in the notified districts of 2011 floods in Sindh. Its purpose is to: Identify high priority union councils with outstanding needs. SHAHEED SHAHEED SHAHEED BENAZIRABAD KHAIRPUR BENAZIRABAD KHAIRPUR BENAZIRABAD KHAIRPUR Facilitate stackholders to plan/support interventions and divert Shah Shah Shah Sikandarabad Sikandarabad Sikandarabad Paritamabad Paritamabad Paritamabad Gujri Gujri resources where they are most needed. Gul Gul Gujri Khadro Khadwari Khadro Khadwari Gul Khadro Khadwari Muhammad Muhammad Muhammad Laghari Laghari Laghari Shahpur Sanghar Shahpur Sanghar Shahpur Sanghar Serhari Chakar Kanhar Serhari Chakar Kanhar Provide common prioritization framework to clusters, agencies Shah Shah Serhari Chakar Kanhar Barhoon Barhoon Barhoon Shah Mardan Abad Mardan Abad Shahdadpur Mian Chutiaryoon Shahdadpur Mian Chutiaryoon Shahdadpur Mardan Abad Mian Chutiaryoon Asgharabad Jafar Sanghar 2 Asgharabad Jafar Sanghar 2 Asgharabad Jafar Sanghar 2 Khan Khan Lundo Soomar Sanghar 1 Lundo Soomar Sanghar 1 Lundo Soomar Khan Sanghar 1 and donors. Faqir HingoroLaghari Laghari Laghari Faqir Hingoro Faqir Hingoro Kurkali Kurkali Kurkali Jatia Jatia Jatia Maldasi Sinjhoro Bilawal Hingoro Maldasi Sinjhoro Bilawal Hingoro Maldasi Sinjhoro Bilawal Hingoro Manik Manik Manik Tahim Khipro Tahim Khipro First round of this exercise is completed from February - March Khori Khori Tahim Khipro Kumb Jan Nawaz Kumb Jan Nawaz Kumb Khori Pero Jan Nawaz DarhoonTando Ali DarhoonTando Pero Ali DarhoonTando Pero Ali Faqir Jan Nawaz Ali Faqir Jan Nawaz Ali Faqir Jan Nawaz Ali AdamShoro Hathungo AdamShoro Hathungo AdamShoro Hathungo Nauabad Nauabad Nauabad 2012. -
Caravan Report
1 | P a g e 2 | P a g e Background: If there is ever to be a Third World War, many believe it will be fought over water, with South Asia serving as the flashpoint. The region houses a quarter of the world’s population and has less than 5 percent of the global annual renewable water resources. Low water availability per person and high frequency of extreme weather events, including severe droughts, further increase the vulnerability of the area. Any disturbance by the country upstream is likely to impact life downstream. Also, as heightened interests to tame and exploit a river through dams, canals and hydel projects suggest, this region will be a zone of constant confrontations in the future. The vision 2025 of Pakistan clearly indicates that the existing flow of water of rivers will be diverted through building various mega schemes for water conservation for energy and agricultural purposes. Such decisions and policies based on vested political interests will further aggravate the socio-economic conditions of deltaic communities of the Sindh. A large water share of the River Indus is utilized by Punjab Province. Resultantly, the lower end of the River Indus that used to be known as “Mighty River Indus” has been reduced to the level of canal shows only tiny inconsistent storage of water. Such a massive destruction of the River Indus has led to the death of livelihood of the deltaic people. The Pakistan government has been planning to build more dams on Indus River. The PFF believes that the indigenous people along with the other natural habitat have the basic right to use the land and water first. -
Pending Biometric) Non-Verified Unknown District S.No Employee Name Father Name Designation Institution Name CNIC Personel ID
Details of Employees (Pending Biometric) Non-Verified Unknown District S.no Employee Name Father Name Designation Institution Name CNIC Personel ID Women Medical 1 Dr. Afroze Khan Muhammad Chang (NULL) (NULL) Officer Women Medical 2 Dr. Shahnaz Abdullah Memon (NULL) 4130137928800 (NULL) Officer Muhammad Yaqoob Lund Women Medical 3 Dr. Saira Parveen (NULL) 4130379142244 (NULL) Baloch Officer Women Medical 4 Dr. Sharmeen Ashfaque Ashfaque Ahmed (NULL) 4140586538660 (NULL) Officer 5 Sameera Haider Ali Haider Jalbani Counselor (NULL) 4230152125668 214483656 Women Medical 6 Dr. Kanwal Gul Pirbho Mal Tarbani (NULL) 4320303150438 (NULL) Officer Women Medical 7 Dr. Saiqa Parveen Nizamuddin Khoso (NULL) 432068166602- (NULL) Officer Tertiary Care Manager 8 Faiz Ali Mangi Muhammad Achar (NULL) 4330213367251 214483652 /Medical Officer Women Medical 9 Dr. Kaneez Kalsoom Ghulam Hussain Dobal (NULL) 4410190742003 (NULL) Officer Women Medical 10 Dr. Sheeza Khan Muhammad Shahid Khan Pathan (NULL) 4420445717090 (NULL) Officer Women Medical 11 Dr. Rukhsana Khatoon Muhammad Alam Metlo (NULL) 4520492840334 (NULL) Officer Women Medical 12 Dr. Andleeb Liaqat Ali Arain (NULL) 454023016900 (NULL) Officer Badin S.no Employee Name Father Name Designation Institution Name CNIC Personel ID 1 MUHAMMAD SHAFI ABDULLAH WATER MAN unknown 1350353237435 10334485 2 IQBAL AHMED MEMON ALI MUHMMED MEMON Senior Medical Officer unknown 4110101265785 10337156 3 MENZOOR AHMED ABDUL REHAMN MEMON Medical Officer unknown 4110101388725 10337138 4 ALLAH BUX ABDUL KARIM Dispensor unknown -
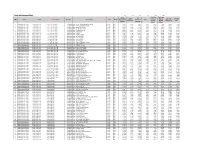
Tando Muhammad Khan
Tando Muhammad Khan 475 476 477 478 479 480 Travelling Stationary Inclass Co- Library Allowance (School Sub Total Furniture S.No District Teshil Union Council School ID School Name Level Gender Material and Curricular Sport Laboratory (School Specific (80% Other) 20% supplies Activities Specific Budget) 1 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010002 GBPS - YAR M. KANDRA@PIR BUX KANDRA Primary Boys 9,117 1,823 7,294 1,823 1,823 7,294 29,175 7,294 2 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010016 GBPS - YAR MUHAMMAD KANDRA Primary Boys 11,323 2,265 9,058 2,265 2,265 9,058 36,233 9,058 3 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010017 GBPS - KHUDA BUX GUMB Primary Boys 14,353 2,871 11,482 2,871 2,871 11,482 45,929 11,482 4 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010022 GBPS - ALAM KHAN TALPUR Primary Boys 44,542 8,908 35,634 8,908 8,908 35,634 142,535 35,634 5 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010025 GBPS - PALIO GHUMRANI Primary Boys 28,220 5,644 22,576 5,644 5,644 22,576 90,303 22,576 6 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. Khan 425010026 GBPS - KARIMABAD Primary Boys 28,690 5,738 22,952 5,738 5,738 22,952 91,808 22,952 7 Tando Muhammad Khan Tando Mohd Khan 1-UC-I Town T.M. -

A Spatio-Temporal Analysis of Rainfall and Drought Monitoring in the Tharparkar Region of Pakistan
remote sensing Article A Spatio-Temporal Analysis of Rainfall and Drought Monitoring in the Tharparkar Region of Pakistan Muhammad Usman 1 and Janet E. Nichol 2,* 1 Centre for Geographical Information System, University of the Punjab, Lahore 54590, Pakistan; [email protected] 2 Department of Geography, School of Global Studies, University of Sussex, Brighton BN19RH, UK * Correspondence: [email protected]; Tel.: +852-9363-8044 Received: 6 January 2020; Accepted: 5 February 2020; Published: 10 February 2020 Abstract: The Tharpakar desert region of Pakistan supports a population approaching two million, dependent on rain-fed agriculture as the main livelihood. The almost doubling of population in the last two decades, coupled with low and variable rainfall, makes this one of the world’s most food-insecure regions. This paper examines satellite-based rainfall estimates and biomass data as a means to supplement sparsely distributed rainfall stations and to provide timely estimates of seasonal growth indicators in farmlands. Satellite dekadal and monthly rainfall estimates gave good correlations with ground station data, ranging from R = 0.75 to R = 0.97 over a 19-year period, with tendency for overestimation from the Tropical Rainfall Monitoring Mission (TRMM) and underestimation from Climate Hazards Group Infrared Precipitation with Stations (CHIRPS) datasets. CHIRPS was selected for further modeling, as overestimation from TRMM implies the risk of under-predicting drought. The use of satellite rainfall products from CHIRPS was also essential for derivation of spatial estimates of phenological variables and rainfall criteria for comparison with normalized difference vegetation index (NDVI)-based biomass productivity. This is because, in this arid region where drought is common and rainfall unpredictable, determination of phenological thresholds based on vegetation indices proved unreliable. -

Population According to Religion, Tables-6, Pakistan
-No. 32A 11 I I ! I , 1 --.. ".._" I l <t I If _:ENSUS OF RAKISTAN, 1951 ( 1 - - I O .PUlA'TION ACC<!>R'DING TO RELIGIO ~ (TA~LE; 6)/ \ 1 \ \ ,I tin N~.2 1 • t ~ ~ I, . : - f I ~ (bFICE OF THE ~ENSU) ' COMMISSIO ~ ER; .1 :VERNMENT OF PAKISTAN, l .. October 1951 - ~........-.~ .1',l 1 RY OF THE INTERIOR, PI'ice Rs. 2 ~f 5. it '7 J . CH I. ~ CE.N TABLE 6.-RELIGION SECTION 6·1.-PAKISTAN Thousand personc:. ,Prorinces and States Total Muslim Caste Sch~duled Christian Others (Note 1) Hindu Caste Hindu ~ --- (l b c d e f g _-'--- --- ---- KISTAN 7,56,36 6,49,59 43,49 54,21 5,41 3,66 ;:histan and States 11,54 11,37 12 ] 4 listricts 6,02 5,94 3 1 4 States 5,52 5,43 9 ,: Bengal 4,19,32 3,22,27 41,87 50,52 1,07 3,59 aeral Capital Area, 11,23 10,78 5 13 21 6 Karachi. ·W. F. P. and Tribal 58,65 58,58 1 2 4 Areas. Districts 32,23 32,17 " 4 Agencies (Tribal Areas) 26,42 26,41 aIIjab and BahawaJpur 2,06,37 2,02,01 3 30 4,03 State. Districts 1,88,15 1,83,93 2 19 4,01 Bahawa1pur State 18,22 18,08 11 2 ';ind and Kbairpur State 49,25 44,58 1,41 3,23 2 1 Districts 46,06 41,49 1,34 3,20 2 Khairpur State 3,19 3,09 7 3 I.-Excluding 207 thousand persons claiming Nationalities other than Pakistani. -
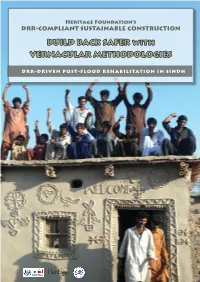
BUILD BACK SAFER with VERNACULAR METHODOLOGIES
Heritage Foundation’s DRR-COMPLIANT SUSTAINABLE CONSTRUCTION BUILD BACK SAFER with VERNACULAR METHODOLOGIES DRR-DRIVEN POST-FLOOD REHABILITATION IN SINDH Introduction to Heritage Foundation eritage Foundation established in 1980 is a Pakistan- based, not-for-profit, social and cultural entrepreneur organization engaged in research, publication and Hconservation of Pakistan’s cultural heritage. The Foundation has been instrumental in saving a large num- ber of heritage treasures and, as UNESCO team leader 2003- 2005, undertook the stabilization of the endangered Shish Ma- hal ceiling of the 16th c. Lahore Fort World Heritage Site. The Foundation publishes monographs and documents relat- ing to heritage and history of Pakistan as well as guides for her- itage safeguarding aspects. It has published a series of invento- ries of historic assets as National Register of Historic Places of Pakistan. In the National Register series, in addition to several Karachi documents listing over 600 historic buildings, docu- ments covering parts of Peshawar, the Siran Valley, Hazara District and Azad Kashmir have been published. Since 2000, its outreach arm KaravanPakistan has involved communities and youth in heritage safeguarding activities. Since 2005, as part of Heritage for Rehabilitation and Devel- opment Program, in partnership with Nokia and Nokia Sie- mens Network, Heritage Foundation has carried out work of rehabilitation of communities, particularly women, affected by the Earthquake 2005 in Northern Pakistan. A 3-year pro- gram, suppported by Scottish Government Fund, Glasgow University and Scottish Pakistan Association on disaster risk resistance (DRR) focusing on women is currently being car- ried out in the Siran Valley. The establishment of KIRAT, Kar- avanPakistan Institute for Research and Training in 2008 has helped in carrying out research and training on varied aspect of sustainable construction techniques drawn from traditional materials and vernacular methods. -
Building Back Stronger
IOM One Room Shelters - 2011 Sindh Floods Response uc, manjhand odero lal village kamil hingoro jhando mari Punjab sekhat khirah Balochistan dasori San gha r ismail jo goth odero lal station khan khahi bilawal hingorjo Matiari roonjho khokhrapar matiari mirabad balouchabad tando soomro chhore bau khan pathan piyaro lund turk ali mari mirpurkhas-05 Sindh shaikh moosa daulatpur shadi pali tajpur pithoro shah mardan shah dhoro naro i m a khan samoon sabho kaplore jheluri Tando Allahpak singhar Yar mosu khatian ii iii iv missan tandojam dhingano bozdar hingorno khararo syed umerkot mirpur old haji sawan khan satriyoon Legend atta muhammad palli tando qaiser araro bhurgari began jarwar mir ghulam hussain Union Council bukera sharif tando hyder dengan sanjar chang mirwah Ume rkot District Boundary hoosri gharibabad samaro road dad khan jarwar girhore sharif seriHyd erabmoolan ad Houses Damaged & Destroyed tando fazal chambar-1 chambar-2 Mirpur Khas samaro kangoro khejrari - Flood 2011 mir imam bux talpur latifabad-20 haji hadi bux 1 - 500 kot ghulam muhammad bhurgari mir wali muhammad latifabad-22 shaikh bhirkio halepota faqir abdullah seri 501 - 1500 ghulam shah laghari padhrio unknown9 bustan manik laghari digri 1501 - 2500 khuda dad kunri 2501 - 3500 uc-iii town t.m. khan pabban tando saindad jawariasor saeedpur uc-i town t.m. khan malhan 3501 - 5000 tando ghulam alidumbalo shajro kantio uc-ii town t.m. khan phalkara kunri memon Number of ORS dilawar hussain mir khuda bux aahori sher khan chandio matli-1 thari soofan shah nabisar road saeed -

Budget Execution Report 2Nd QUARTER 2020-21
Budget Execution Report 2nd QUARTER 2020-21 31th December, 2020 Government of Sindh Finance Department Table of contents: Introduction ............................................................................................................................................................................. 2 Table 1 Interim Fiscal Statement .......................................................................................................................................... 3 Table 2 Revenue by Object .................................................................................................................................................... 4 Table 3 Revenue by Department........................................................................................................................................... 7 Table 4 Expenditure by Department .................................................................................................................................... 9 Table 5 Recurrent Expenditure by Department, Grant and Object ............................................................................... 20 Table 6 Provincial ADP by Sector and Sub-sector .......................................................................................................... 41 Table 7 Development Expenditure by Sector, Subsector and Scheme ....................................................................... 42 Table 8 Current Capital Expenditure ............................................................................................................................... -

1951-81 Population Administrative . Units
1951- 81 POPULATION OF ADMINISTRATIVE . UNITS (AS ON 4th FEBRUARY. 1986 ) - POPULATION CENSUS ORGANISATION ST ATIS TICS DIVISION GOVERNMENT OF PAKISTAN PREFACE The census data is presented in publica tions of each census according to the boundaries of districts, sub-divisions and tehsils/talukas at the t ime of the respective census. But when the data over a period of time is to be examined and analysed it requires to be adjusted fo r the present boundaries, in case of changes in these. It ha s been observed that over the period of last censuses there have been certain c hanges in the boundaries of so me administrative units. It was, therefore, considered advisable that the ce nsus data may be presented according to the boundary position of these areas of some recent date. The census data of all the four censuses of Pakistan have, therefore, been adjusted according to the administ rative units as on 4th February, 1986. The details of these changes have been given at Annexu re- A. Though it would have been preferable to tabulate the whole census data, i.e., population by age , sex, etc., accordingly, yet in view of the very huge work involved even for the 1981 Census and in the absence of availability of source data from the previous three ce nsuses, only population figures have been adjusted. 2. The population of some of the district s and tehsils could no t be worked out clue to non-availability of comparable data of mauzas/dehs/villages comprising these areas. Consequently, their population has been shown against t he district out of which new districts or rehsils were created. -

Soes March 2021
Implementation and Economic Reforms Unit Ministry of Finance, Islamabad Tel: 051-9217854 www.finance.gov.pk FY 2019 VOL 1: COMMERCIAL SOEs March 2021 FEDERAL FOOTPRINT SOEs ANNUAL REPORT TABLE OF CONTENTS LIST OF ABBREVIATIONS ______________________________________________________________________________ 2 LIST OF TABLES __________________________________________________________________________________________ 3 FOREWORD ______________________________________________________________________________________________ 4 PORTFOLIO OVERVIEW ________________________________________________________________________________ 5 EXECUTIVE SUMMARY ________________________________________________________________________________ 11 INTRODUCTION _______________________________________________________________________________________ 12 Year in Review - Financial _____________________________________________________________________________ 13 Year in Review - Infrastructure, Transport and ITC _________________________________________________ 17 Year in Review - Manufacturing, Mining & Engineering ____________________________________________ 21 Year in Review - Oil & Gas _____________________________________________________________________________ 25 Year in Review - Power ________________________________________________________________________________ 29 Year in Review - Industrial Estate Development ____________________________________________________ 33 Year in Review - Trading and Marketing _____________________________________________________________ -
Drought Assessment Report Districts Tharparkar and Umerkot
Rapid Assessment Report Draft (19th November 2014) Drought Assessment Report Districts Tharparkar and Umerkot 26th October -- 1st November 2014 Consortium Management Unit PEFSA V Table of Contents 1 EXECUTIVE SUMMARY ..................................................................................................... 4 2 THE CONTEXT ................................................................................................................ 6 2.1 Background ............................................................................................................................. 6 2.2 Methodology ........................................................................................................................... 6 2.2.1 Objective ....................................................................................................................................... 7 2.2.2 Approach to Assessment .............................................................................................................. 7 2.3 Demographics ......................................................................................................................... 8 2.4 Taluka wise Affected Union Councils of District Tharparkar .................................................. 9 3 MAIN FINDINGS ........................................................................................................... 11 3.1 Affected population and Migration ...................................................................................... 11 3.2 Drought Intensity