New Zealand Data Sheet APO-CLOMIPRAMINE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

Dosulepin Prescribing
SAFETY BULLETIN: DOSULEPIN PRESCRIBING In December 2007, the Medicines and Healthcare Regulatory Agency (MHRA) issued safety advice around prescribing of dosulepin, related to the narrow margin between therapeutic doses and potentially fatal doses. Nevertheless, dosulepin continues to be prescribed widely. Over eight years after the safety advice was published, prescribing of dosulepin in the Dorset area remains high. In the South West area, Dorset CCG was the highest prescriber of dosulepin for the 2015/16 financial year (3.238% of all antidepressant items). Of the 209 CCGs in the UK, Dorset is the fourteenth highest prescriber of dosulepin, and well above the national average of 2.111%. The following points summarise the reasons that dosulepin is not recommended for prescribing nationally, and in Dorset: Dosulepin has a small margin of safety between the (maximum) therapeutic dose and potentially fatal doses. The NICE guideline on depression in adults recommends that dosulepin should not be prescribed for adults with depression because evidence supporting its tolerability relative to other antidepressants is outweighed by the increased cardiac risk and toxicity in overdose. Dosulepin has also been used ‘off label’ in other indications such as fibromyalgia and neuropathic pain. However the evidence for use in in this way is weak, and is not recommended. The lethal dose of dosulepin is relatively low and can be potentiated by alcohol and other CNS depressants. Dosulepin overdose is associated with high mortality and can occur rapidly, even before hospital treatment can be received. Onset of toxicity occurs within 4-6 hours. Every year, up to 200 people in England and Wales fatally overdose with dosulepin. -

Switching from Clonidine Immediate-Release to Guanfacine Extended-Release
/ DE L’ACADÉMIE CANADIENNE DE PSYCHIATRIE DE L’ENFANT ET DE L’ADOLESCENT PSYCHOPHARMACOLOGY Switching from Clonidine Immediate-Release to Guanfacine Extended-Release Dean Elbe PharmD, BCPP1,2,3 s a clinical pharmacy specialist in child and adolescent (Canada) Ltd, 2012b). Clonidine has been used off-label Amental health, I am frequently asked how to switch in children for many years for treatment of insomnia, patients from clonidine immediate-release (IR) to guanfa- ADHD, and disruptive behaviour disorders (Hunt, Capper cine extended-release (XR). This therapeutic switch may be & O’Connell, 1990; Rubinstein; Jaselskis, Cook, Fletcher required when poor adherence to a clonidine IR regimen & Leventhal, 1992; Silver & Licamele, 1994; Palumbo et (typically requiring 3–4 doses daily) is identified, when al., 2008; Efron, Lycett & Sciberras, 2014). A clonidine XR clonidine dose-optimization is limited by sedation, brady- formulation is not available in Canada, but is available in cardia or hypotension, or when coverage situations change. the United States for treatment of ADHD (Concordia Phar- The latter may occur if, for example, new eligibility for a maceuticals, Inc. 2015). government program or a third party-payer occurs. Weight-based dosing guidelines exist for clonidine IR Guanfacine XR, a selective alpha2A agonist, was first mar- (0.003–0.008 mg/kg/day) and guanfacine XR (0.05–0.08 keted in Canada in late 2013 for the treatment of attention mg/kg/day) (Shire Pharma Canada ULC, 2019; Elbe et deficit hyperactivity disorder (ADHD) in children and ado- al., 2018). Based on these guidelines and other literature, lescents (Shire Pharma Canada ULC, 2019). -

Molecular Signatures of G-Protein-Coupled Receptors A
REVIEW doi:10.1038/nature11896 Molecular signatures of G-protein-coupled receptors A. J. Venkatakrishnan1, Xavier Deupi2, Guillaume Lebon1,3,4,5, Christopher G. Tate1, Gebhard F. Schertler2,6 & M. Madan Babu1 G-protein-coupled receptors (GPCRs) are physiologically important membrane proteins that sense signalling molecules such as hormones and neurotransmitters, and are the targets of several prescribed drugs. Recent exciting developments are providing unprecedented insights into the structure and function of several medically important GPCRs. Here, through a systematic analysis of high-resolution GPCR structures, we uncover a conserved network of non-covalent contacts that defines the GPCR fold. Furthermore, our comparative analysis reveals characteristic features of ligand binding and conformational changes during receptor activation. A holistic understanding that integrates molecular and systems biology of GPCRs holds promise for new therapeutics and personalized medicine. ignal transduction is a fundamental biological process that is comprehensively, and in the process expand the current frontiers of required to maintain cellular homeostasis and to ensure coordi- GPCR biology. S nated cellular activity in all organisms. Membrane proteins at the In this analysis, we objectively compare known structures and reveal cell surface serve as the communication interface between the cell’s key similarities and differences among diverse GPCRs. We identify a external and internal environments. One of the largest and most diverse consensus structural scaffold of GPCRs that is constituted by a network membrane protein families is the GPCRs, which are encoded by more of non-covalent contacts between residues on the transmembrane (TM) than 800 genes in the human genome1. GPCRs function by detecting a helices. -

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

22 Psychiatric Medications for Monitoring in Primary Care
22 Psychiatric Medications for Monitoring in Primary Care Medication Warnings, Precautions, and Adverse Events Comments Class: SSRI Fluvoxamine Boxed Warnings: Suicidality Used much less than SSRIs in the group of eight Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, probably because it has no Adult: OCD Adverse Events: Similar to other SSRIs FDA indication for MDD or any anxiety disorder. Still Child/Adolescent: OCD (10-17 years) somewhat popular as a medication for OCD. Uses: Anxiety, OCD Monitoring: Same as other SSRIs Citalopram Boxed Warning: Suicidality. Escitalopram, one of the SSRIs in the group of Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, is an active metabolite of Adult: MDD Adverse Events: Similar to other SSRIs citalopram. Escitalopram reportedly has fewer AEs and Child/Adolescent: None less interaction with hepatic metabolic enzymes than Uses: Anxiety, MDD, OCD citalopram but is otherwise essentially identical. Citalopram offers no advantage other than price, as Monitoring: Same as other SSRIs escitalopram is branded until 2012. Paroxetine Boxed Warnings: Suicidality. Paroxetine used much less than the SSRIs for Indications: Warnings and Precautions: Similar to other SSRIs prescribing, probably because of its nonlinear kinetics. Adult: MDD, OCD, Panic Disorder, Generalized Anxiety Adverse Events: Similar to other SSRIs A study of children and adolescents showed doubling Disorder, Social Anxiety Disorder, Posttraumatic Stress Disorder the dose of paroxetine from 10 mg/day to 20 mg/day Child/Adolescent: None resulted in a 7-fold increase in blood levels (Findling et Uses: Anxiety, MDD, OCD al, 1999). Thus, once metabolic enzymes are saturated, paroxetine levels can increase dramatically with dose Monitoring: Same as other SSRIs increases and decrease dramatically with dose decreases, sometimes leading to adverse events. -

Clomipramine | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Clomipramine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Anafranil Brand Names: Canada Anafranil; MED ClomiPRAMINE; TARO-Clomipramine Warning Drugs like this one have raised the chance of suicidal thoughts or actions in children and young adults. The risk may be greater in people who have had these thoughts or actions in the past. All people who take this drug need to be watched closely. Call the doctor right away if signs like low mood (depression), nervousness, restlessness, grouchiness, panic attacks, or changes in mood or actions are new or worse. Call the doctor right away if any thoughts or actions of suicide occur. This drug is not approved for use in all children. Talk with the doctor to be sure that this drug is right for your child. What is this drug used for? It is used to treat obsessive-compulsive problems. It may be given to you for other reasons. Talk with the doctor. Clomipramine 1/8 What do I need to tell my doctor BEFORE I take this drug? If you have an allergy to clomipramine or any other part of this drug. If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have had a recent heart attack. If you are taking any of these drugs: Linezolid or methylene blue. -

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Drugs That Can Cause Delirium (Anticholinergic / Toxic Metabolites)
Drugs that can Cause Delirium (anticholinergic / toxic metabolites) Deliriants (drugs causing delirium) Prescription drugs . Central acting agents – Sedative hypnotics (e.g., benzodiazepines) – Anticonvulsants (e.g., barbiturates) – Antiparkinsonian agents (e.g., benztropine, trihexyphenidyl) . Analgesics – Narcotics (NB. meperidine*) – Non-steroidal anti-inflammatory drugs* . Antihistamines (first generation, e.g., hydroxyzine) . Gastrointestinal agents – Antispasmodics – H2-blockers* . Antinauseants – Scopolamine – Dimenhydrinate . Antibiotics – Fluoroquinolones* . Psychotropic medications – Tricyclic antidepressants – Lithium* . Cardiac medications – Antiarrhythmics – Digitalis* – Antihypertensives (b-blockers, methyldopa) . Miscellaneous – Skeletal muscle relaxants – Steroids Over the counter medications and complementary/alternative medications . Antihistamines (NB. first generation) – diphenhydramine, chlorpheniramine). Antinauseants – dimenhydrinate, scopolamine . Liquid medications containing alcohol . Mandrake . Henbane . Jimson weed . Atropa belladonna extract * Requires adjustment in renal impairment. From: K Alagiakrishnan, C A Wiens. (2004). An approach to drug induced delirium in the elderly. Postgrad Med J, 80, 388–393. Delirium in the Older Person: A Medical Emergency. Island Health www.viha.ca/mhas/resources/delirium/ Drugs that can cause delirium. Reviewed: 8-2014 Some commonly used medications with moderate to high anticholinergic properties and alternative suggestions Type of medication Alternatives with less deliriogenic -
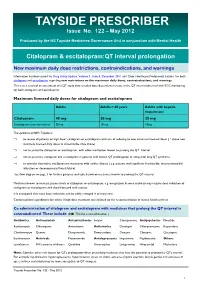
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

FDA Approved Drugs with Broad Anti-Coronaviral Activity Inhibit SARS-Cov-2 in Vitro
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.25.008482; this version posted March 27, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. FDA approved drugs with broad anti-coronaviral activity inhibit SARS-CoV-2 in vitro Stuart Weston1, Rob Haupt1, James Logue1, Krystal Matthews1 and Matthew B. Frieman*1 1 - Department of Microbiology and Immunology, University of Maryland School of Medicine, 685 W. Baltimore St., Room 380, Baltimore, MD, 21201, USA *Corresponding author. Email: [email protected] Key words: SARS-CoV-2, nCoV-2019, COVID-19, drug repurposing, FDA approved drugs, antiviral therapeutics, pandemic, chloroquine, hydroxychloroquine AbstraCt SARS-CoV-2 emerged in China at the end of 2019 and has rapidly become a pandemic with over 400,000 recorded COVID-19 cases and greater than 19,000 recorded deaths by March 24th, 2020 (www.WHO.org) (1). There are no FDA approved antivirals or vaccines for any coronavirus, including SARS-CoV-2 (2). Current treatments for COVID-19 are limited to supportive therapies and off-label use of FDA approved drugs (3). Rapid development and human testing of potential antivirals is greatly needed. A potentially quicker way to test compounds with antiviral activity is through drug re-purposing (2, 4). Numerous drugs are already approved for use in humans and subsequently there is a good understanding of their safety profiles and potential side effects, making them easier to test in COVID-19 patients.