The Pitfalls of Mass Hospital Healthcare Worker Testing for COVID
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Urgent Statement from Hospitals in the City of Toronto and the Regions of Durham, Halton, Peel and York GTA Hospitals Support Further Lockdown Measures
An Urgent Statement from Hospitals in the City of Toronto and the Regions of Durham, Halton, Peel and York GTA Hospitals Support Further Lockdown Measures December 20, 2020 - Today, on behalf of our patients, health care workers and staff, we are supporting the Ontario Hospital Association’s call for stronger lockdown measures from the Government of Ontario. Across the Greater Toronto Area, COVID-19 infections are continuing to rise, as are hospitalizations and intensive care cases. These trends show no sign of slowing – in fact, a surge in cases following the holiday season is expected to make the situation even worse. Our staff are caring for increasing numbers of COVID-19 patients in hospitals and assisting in other settings such as long-term care homes. They are also keeping up with the care needs of patients without COVID-19 and trying to make progress in the significant backlog of scheduled surgeries and procedures cancelled during the first wave. For many months now, these frontline health care workers have been devoting enormous energy and skill to caring for their patients, at the very epicenter of the pandemic. They are stressed and overstretched. This level of strain is simply not sustainable for much longer. We are seeing increasing numbers of staff becoming ill and not able to work – both with COVID-19 and other illnesses. While we are coping and planning for redeployment, we are seeing more illness and stress and hearing about the toll this is taking on people’s families. We recognize that lockdown measures are challenging for many members of our communities, but we cannot afford to put patients and health care workers at further risk. -
Redesigning Care Through Digital Health Implementation
Redesigning Care through Digital Health Implementation Lessons Learned from Ontario Hospitals Acknowledgements The Ontario Hospital Association (OHA) would like to thank all the member hospitals and provincial partners who contributed to this resource. Individual contributing authors are noted at the end of each story. The OHA also acknowledges the ongoing and valuable work of all health care professionals who embrace change as hospitals innovate to improve care delivery and patient experiences. Disclaimer This publication is a collection of hospital submissions The Ontario Hospital Association (OHA) assumes no showcasing digital health implementation initiatives responsibility or liability for any harm, damage or other across the province. It has been created for general losses, direct or indirect, resulting from any reliance on information purposes only and implementation the use or the misuse of any information contained in suggestions should be adapted to the circumstances of this resource. Facts, figures and resources mentioned each hospital. Hospitals should seek their own legal and/ throughout the document have not been validated by or professional advice and opinion when developing the OHA. For details on sources of information, readers their organization’s approach and plans for digital health are encouraged to contact the hospital directly using the implementation. contact information cited in each submission. I Introduction Digital technologies have, and will continue to, These factors point to what may be the key ingredient -

MEDICAL RESOURCES During COVID-19
MEDICAL RESOURCES During COVID-19 If You Think You Have COVID-19: If you are having symptoms of COVID-19 and need to get screened, it is important to follow the guidelines of Toronto Public Health and the Government of Ontario. DO NOT show up unannounced at a clinic or hospital. Instead follow these guidelines: Review this Self-Assessment Tool www.ontario.ca/page/2019-novel-coronavirus-covid-19-self-assessment If you answered yes to any of those questions on the Self-Assessment Tool, then seek assistance over the phone with Telehealth Ontario: Telehealth Ontario 24/7 | 1-866-797-0000 | Speak with a registered nurse regarding your symptoms If it is confirmed you need to be tested, visit one of these dedicated COVID-19 assessment centres: William Osler Health System – Peel Memorial 2-8pm daily | 20 Lynch Street, Brampton | 905-494-2120 Trillium Health Partners 9:30am-9:30pm daily | call 905-799-7700 first Mississauga Hospital: 15 Bronte College Court, Mississauga, ON Credit Valley Hospital: 2200 Erin Mills Parkway, Mississauga, ON North York General Hospital 11am-11pm daily | 4001 Leslie Street, North York, ON | 416-756-6000 Michael Garron Hospital 8am-8pm | 825 Coxwell Avenue | 416-469-6858 BY APPOINTMENT ONLY. CALL TO BOOK. Women’s College Hospital 9am-8pm daily | 76 Grenville Street | 416-323-6400 Humber River Hospital 12pm-8pm Monday-Friday | 2111 Finch Avenue West | 416-242-1000 St. Joseph’s Health Centre 9am-9pm daily | Sunnyside Building 1st floor; 30 The Queensway St. Michael’s Hospital 9am-7pm daily | Li Ka Shing Knowledge Institute; -

Hospital Lhins Contact List
Hospital LHINs Contact List Patient Hospital LHIN Hospital LHIN LHIN Hospital Inquiry or Main Direct # or Address Map Fax # Number Extension Hotel-Dieu Grace Healthcare 519-257-5111 1453 Prince Rd Map it! (HDGH)(Windsor) Windsor, ON N9C 3Z4 Leamington District Memorial 519-326-2373 194 Talbot St W Map it! Hospital Leamington, ON N8H 1N9 Windsor Regional Hospital- 519-254-5577 1995 Lens Ave Map it! Metropolitan Campus Windsor, ON N8W 1L9 Windsor Regional Hospital- 519-253-5253 2220 Kildare Rd Map it! Erie St Clair LHIN Windsor Regional Cancer Windsor, ON N8W 2X3 1-888-447-4468 Centre Windsor Regional Hospital- 519-973-4411 1030 Ouellette Ave Map it Ouellette Campus Windsor, ON N9A 1E1 Chatham-Kent Health 519-352-6400 80 Grand Ave W Map it! Alliance-Chatham Campus Chatham, ON N7M 5L9 Chatham-Kent Health 519-352-6400 325 Margaret Ave Map it! Alliance Sydenham Campus Wallaceburg ON, N8A 2A7 Bluewater Health 419-464-4400 89 Norman St Map it! Sarnia, ON N7T 6S3 Charlotte Eleanor Englehart 519-882-4325 450 Blanche St Map it! Hospital of Bluewater Health Petrolia, ON N0N 1R0 1 Jan 2012 (Update Oct 12, 2016) Hospital LHIN(s) Contact List - Ontario Page 1 of 15 Patient Hospital LHIN Hospital LHIN LHIN Hospital Inquiry or Main Direct # or Address Map Fax # Number Extension Middlesex Hospital Alliance- 519-693-4441 519-474-5662 519-472-4045 1824 Concession Dr Map it! Four Counties Health Services Newbury, ON N0L 1Z0 Middlesex Hospital Alliance- 519-245-5295 519-474-5662 519-472-4045 395 Carrie St Map it! Strathroy Middlesex General Strathroy, ON N7G 3J4 Hospital London Health Sciences Centre 519-685-8500 519-474-5662 519-472-4045 800 Commissioners Rd E Map it! - Victoria Hospital London, ON N6A 5W9 London Health Sciences 519-685-8500 519-474-5662 519-472-4045 339 Windermere Rd Map it! Centre-University Hospital London, ON N6A 5A5 St Joseph's Health Care 519-646-6100 519-474-5662 519-472-4045 268 Grosvenor St Map it! London- St. -

Fracture Clinic Access at Toronto Hospitals Not All Hospitals Offer Fracture Clinic Telephone Call Or Referral Required - No Walk-Ins Accepted
Fracture Clinic Access at Toronto Hospitals Not all hospitals offer fracture clinic Telephone call or referral required - no walk-ins accepted Note: Fracture clinics are not for initial evaluation and stabilization of acute fractures. This must be done at primary care or emergency department level as appropriate Humber River Hospital 416-242-1000 Monday to Friday 7:30 am – 4:30 pm 1235 Wilson Ave x 23000 2.5 hrs for each AM, PM clinic Toronto, M3M 0B2 Call to speak to ortho-on-call, will accept if space avail Michael Garron Hospital 416-469-6384 Monday, Tuesday, Friday 8 – 4 pm 825 Coxwell Avenue Fx: 416-469-6424 Wednesday, Thurs 8:30 – 4 pm Toronto, M4C 3E7 Referral triaged according to urgency North York General Hospital 416-756-6970 Use referral form, only for minor fracture, 1st flr, West Lobby Fx: 416-756-6502 splinting/casting 4001 Leslie St., 1st flr Located near the Information Desk Toronto, M2K 1E1 Scarborough Health Network 416-495-2557 Referrals/consultation not accepted from Birchmount Hospital community physicians/NPs. 2 ways to access clinic: 3030 Birchmount Rd., 1) Through ER d/t injury Scarborough, M1W 3W3 2) Apt scheduled by Ortho Scarborough Health Network 416-431-8212 Monday to Thursday 7:00-3:00 pm General Hospital Refer to individual Ortho to obtain appointment 3050 Lawrence Ave. E., Scarborough, M1P 2V5 Scarborough Health Network 416-281-7269 Monday to Friday 7:30-3:30 pm Centenary Hospital Fx: 416-281-7204 2867 Ellesmere Road, M1E 4B9 Mount Sinai Hospital 416-596-4200 Clinic hours vary. -

Supporting Those Impacted by COVID-19
Supporting those impacted by COVID-19 Many of you have reached out to us either looking for suggestions or offering ideas on how our TFS community can support those impacted by COVID-19. We are indeed a strong community and we know that it is essential, as citizens, that we act for the common good, most especially in situations such as this one. Please see below a list of organizations that you might want to support, specifically considering the shortage of personal protective equipment and other items. Of the many worthy institutions making an impact, we have put together a list of those with which we have partnered over the years as part of our citizenship program or where our alumni and parents are engaged. We will post this list online at tfs.ca and sr.tfs.ca/coronavirus. To quote President John F. Kennedy, from his inaugural speech, “Ask not what your country can do for you - ask what you can do for your country.” Or province or city. And, of course, for the world at large. Thank you! Baycrest Hospital CAMH Canadian Cancer Society Daily Bread Food Bank Holland Bloorview Kids Rehabilitation Hospital Humber River Hospital Lakeridge Health Mackenzie Health Markham Stouffville Hospital Michael Garron Hospital Foundation Oakville Hospital Foundation North York General Hospital Foundation Second Harvest Scarborough Hospital Network Foundation Sick Kids Foundation Sinai Health System Southlake Regional Health Centre Sunnybrook Health Sciences Centre Toronto General & Western Hospitals Toronto Rehab Trillium Health Partners Foundation Unity Health (St. Michael's, St. Joseph's and Providence Health Care) War Child William Osler Health System Women's College Hospital Foundation . -
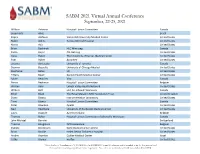
Current Attendee List
SABM 2021 Virtual Annual Conference September, 22-25, 2021 William Acheson Hospital Liaison Committee Canada Susankerle Alves Brazil Kaycie Atchison Vanderbilt University Medical Center United States Robin Atkins Tampa General Hospital United States Maria Aziz United States Brian Bachinski HLC Winnipeg Canada Paolo Bajcic CSL Behring United States Dana Baker The University of Kansas Medical Center United States Pam Baker Accumen United States Justyna Bartoszko University of Toronto Canada Deanna Bassette University of Chicago Medical United States Stephanie Bates UC United States Tiffany Beam Garnet Health Medical Center United States Sylvie Beaulieu Visa Canada Pierre Beekman Hospital Liaison Committee Belgium Warren Behr Lehigh Valley Health Network United States William Bell HLC for Jehovah Witnesses Canada Ethel Black The Royal Marsden NHS Foundation Trust United Kingdom Diana Blanco Instrumentation Laboratory United States Trent Blanco Hospital Liaison Committee Canada Peter Blandino Apellis United States Neil Blumberg University of Rochester Medical Center United States Laura Bogaert AZ Rivierenland Belgium Thomas Bokor Hospital Liaison Committee of Jehovah's Witnesses Canada John Michael Bonvini Switzerland Thomas Boogmans AZ Rivierenland Belgium Pamela Bordonaro Keck Medical Center at USC United States Brian Boville Helen DeVos Children's Hospital United States Andrei Braester Galilee Medical Center Israel Cathy Brewer werfen United States This is the list of Attendees as of 8/23/2021 for the SABM 2021 Annual Conference and is -

2020 International Symposium on Human Factors and Ergonomics in Health Care Program Committee Consists of Experts in a Wide Variety of Domains and Organizations�
INTERNATIONAL SYMPOSIUM ON HUMAN FACTORS AND ERGONOMICS IN HEALTH CARE VIRTUAL CONFERENCE | MAY 18-21, 2020 TABLE OF CONTENTS WELCOME ...............................................................................................................................................3 PROGRAM COMMITTEE ..................................................................................................................4 SPONSORS, EXHIBITORS, & ADVERTISERS .......................................................................5 SCHEDULE AT A GLANCE ..............................................................................................................7 MONDAY, MAY 18 - WORKSHOPS ...............................................................................................8 TUESDAY, MAY 19 - LECTURE PROGRAM Digital Health .................................................................................................................................10 Hospital Environments ..............................................................................................................13 Medical and Drug-Delivery Devices ..................................................................................15 Patient Safety Research and Initiatives ............................................................................17 WEDNESDAY, MAY 20 - LECTURE PROGRAM Digital Health ............................................................................................................................11-12 Hospital Environments ..............................................................................................................14 -

AC Open Sites 18 March 2020.Xlsx
Region Title Location name / operated by (lead HSP) City, Address, Postal Code Womens College Hospital 76 Grenville St. Toronto Womens College Hospital 76 Grenville St, Toronto ON Toronto North York General Ambulance Bay Ambulance Bay ‐ 4001 Leslie Street 4001 Leslie Street Toronto ON Michale Garron Hospital ‐ 825 Coxwell Avenue, Toronto ON 1) ED COVID‐19 Assessment Centre (ED, through Mortimer entrance); 2) COVID‐19 Assessment Centre ‐ Outpatient clinic location in D‐wing, 1st floor at hospital; accessed directly off of Mortimer Avenue – exterior of the hospital (intersection of Toronto Michael Garron Hospital Coxwell Ave / Mortimer Ave) 825 Coxwell Avenue, Toronto ON HRH Assessment Centre Humber River Hospital Assessment 2111 Finch Ave West Phone 416‐747‐6740 Toronto Centre Former HRH Finch Site 2111 Finch Ave West, Toronto ON St Michael's Hospital Site Toronto, ON Toronto St. Michaels Hospital Site (Unity) Li Ka Shing Knowledge Institute 209 Victoria Street ‐ ENTER at Shuter Street Door Toronto St. Joseph's Health Centre (Unity) St. Joseph's Health Centre Site 30 The Queensway Toronto M6R 1B5 Toronto Scarborough Health Network Scarborough Health Network 3030 Birchmount Rd Scar M1W3W3 Sunnybrook Health Sciences Centre Toronto U G round Sunnybrook Health Sciences Centre U G round 2075 Bayview Ave, Toronto, ON West St. Mary's General St. Mary's General 911 Queen's Boulevard, Kitchener, ON N2M 1B2 West Grand River Grand River 835 King St. W., Kitchener, ON N2G 1G3 1245 Lakeshore Rd. West Joseph Brant Hospital Joseph Brant Hospital Burlington, ON L7S 0A2 153 Christina Street West Bluewater Health Sarnia Bluewater Health Sarnia Sarnia ON N7T2M9 West St. -

Six Hospitals to Deliver Enhanced Care to Patients in Unique Restorative Care Facility
FOR IMMEDIATE RELEASE Six hospitals to deliver enhanced care to patients in unique restorative care facility May 6, 2019 (TORONTO, ON) – Six Greater Toronto Area hospitals are working side by side under one roof to provide specialized care for patients who no longer require acute hospital services. Thanks to funding from the Ministry of Health and Long-Term Care, the Reactivation Care Centre – Church Site has been newly refurbished and modernized for patients who can benefit from specialized restorative services. Following ten weeks of extensive preparations, starting May 5, patients from Trillium Health Partners, Southlake Regional Health Centre, William Osler Health System, and St. Joseph’s Health Centre Toronto began moving into the newly renovated site, which has capacity for 214 beds. As owner of the site, Humber River Hospital, has led the complex redevelopment of the building and overseen all aspects of the plan to bring the latest four hospitals into the building. Ninety-two patients from Humber and Sunnybrook Health Sciences Centre have been receiving care in the Reactivation Care Centre since December 2018. At the Reactivation Care Centre, patients receive the specialized care and support they need, including occupational therapy, recreational therapy and physiotherapy, to improve their health outcomes and patient experience. Each hospital operates its own standalone unit within a wing or floor of the building and employs its own nursing staff and therapists, among others. The initiative is making use of existing infrastructure to provide patients with safe, high quality care in the most suitable location. At the same time, it is addressing the challenge of hallway health care by improving access to services and reducing wait times in these hospitals’ acute care sites. -

Mount Sinai Hospital
Toronto Invasive Bacterial Diseases Network INFORMATION ABOUT A RESEARCH STUDY – STAFF and CAREGIVERS TIBDN CO-ORDINATING INVESTIGATOR: Dr. Allison McGeer Study Title: Immunogenicity of COVID-19 Vaccines in Long Term Care (CovidAB) 416-586-3123 Study Doctors: Dr. Anne Claude Gingras, Sinai Health System COVIDAB RESEARCH COORDINATOR: Dr. Allison McGeer, Sinai Health System Ms. Lois Gilbert Dr. Jen Gommerman, University of Toronto 416-586-4800, 2767 Dr. Sharon Straus, Unity Health Toronto Dr. Mario Ostrowski, Unity Health RESEARCH ASSOCIATES: Mr. Agron Plevneshi Ms. Nadia Malik What is the purpose of this study? Ms. Mare Pejkovska Ms. Asfia Sultana The purpose of this study is to better understand how vaccines work against COVID-19. We Ms. Amna Faheem wish to describe: Ms. Saman Khan 1. how much antibody people make when they are vaccinated against the virus that Mr. Kazi Hassan Ms. Tamara Vikulova causes COVID-19 Ms. Gloria Crowl 2. how long the antibody lasts Ms. Zoe Zhong Ms. Lubna Farooqi 3. whether people who have had COVID-19 before make more antibody, or have antibody that lasts longer RESEARCH TECHNOLOGISTS: 4. whether residents of long term care homes make less antibody than other adults Ms. Aimee Paterson 5. whether antibodies can be detected in saliva of individuals vaccinated against Ms. Angel Xin Liu COVID19 , how it compares to antibody levels detected in blood, and how long does it last in the saliva MAIN OFFICE: Mount Sinai Hospital Who can participate? Anyone who works, or is an essential caregiver at a long term care 600 University Avenue home in south central Ontario, and who is planning to be vaccinated against COVID-19. -

2018 FCMS Brochure V6
CONFERENCE OBJECTIVES SUNDAY, OCTOBER 21, 2018 W1: Mental Health Workshop • Participants will be able to identify ethno- 800-900 Breakfast Why ACT? How to ACT? Thinking and cultural differences that affect prevalence, ACTing Differently When Treating symptom presentation, investigation, and Poster Session/Abstracts Review Addictions Dr. Vincent Lam treatment of common health problems among Exhibits North American Chinese A Primer on Responding to Patient • Participants will be able to identify emergent or 900-1030 Plenary II Chinese Canadian Medical Society unmet healthcare needs among North American Requests for Medical Assistance in Dying Chinese Viral Hepatitis and Fatty Liver Disease (MAID) (Ontario) • Participants will be able to develop a cultural among the Chinese Dr. Madeline Li Federation of Chinese American & competent approach towards addressing Dr. David HK Wong Chinese Canadian Medical Societies important differences in common health issues 1455-1510 Break facing North American Chinese I Robot – High Tech Comes to Medicine Dr. Peter Lin 1510-1700 CONCURRENT SESSIONS II Presents Registration Required SATURDAY, OCTOBER 20, 2018 1030-1130 HENRY B. WOO & BESSIE K. WOO (Please choose one) th 1300-1350 Lunch FOUNDATION LECTURE 19 International Conference S2: Stroke Symposium: Different Financial Talk Stroke for Different Folks – on Health Care of the Ron Choo The Art and Science on the Practice of Cerebrovascular Diseases amongst Medicine Chinese living in North America Chinese in North America 1350-1400 Opening Remarks & Introduction Dr. Herbert Ho-Ping Kong Awareness of Warning Symptoms of Heart Disease and Stroke: Follow-Up 1400-1500 DR. HARRY LEE MEMORIAL LECTURE 1130-1300 Lunch Study of the Chinese Canadian Cardiovascular Health Project (CCCVHP) Optimizing Health CV Disease Amongst North American 1145-1225 Satellite Symposia Dr.