Psychology-Internship-Program-Intern
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2017 Match Day Results by Program
Class of 2017 Match Results Anesthesiology New York Presbyterian Hospital-Columbia University Medical Center University of Illinois College of Medicine-Chicago University of Texas Medical School-Houston Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Florida College of Medicine-Shands Hospital New York Presbyterian Hospital-Weill Cornell Medical Center Einstein/Montefiore Medical Center (New York) New York Presbyterian Hospital-Columbia University Medical Center Dermatology University at Buffalo School of Medicine (New York) University of Buffalo School of Medicine (New York) Cleveland Clinic Foundation (OH) Emergency Medicine Einstein/Montefiore Medical Center (New York) University of Massachusetts Medical School Staten Island University Hospital (New York) Stanford University Programs (California) Stony Brook Teaching Hospitals (New York) New York Hospital Medical Center Queens (New York) Eastern Virginia Medical School University of Washington Affiliated Hospitals Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Connecticut School of Medicine Rhode Island Hospital/Brown University Wake Forest Baptist Medical Center (North Carolina) Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) Einstein/Montefiore Medical Center (New York) Oregon Health and Science University Dartmouth-Hitchcock Medical Center (New Hampshire) Einstein/Montefiore Medical Center (New York) University of Washington Affiliated Hospitals Einstein/Montefiore Medical Center -

New York City Health and Hospitals Corporation New York City Health and Hospitals Corporation
NEW YORK CITY HEALTH AND HOSPITALS CORPORATION NEW YORK CITY HEALTH AND HOSPITALS CORPORATION Bronx Kings County Hospital Center Metropolitan Hospital Center Jacobi Medical Center 451 Clarkson Avenue 1901 First Avenue 1400 Pelham Parkway South Brooklyn, New York 11203 New York, New York 10029 Bronx, New York 10461 718-245-3131 212-423-6262 212-918-5000 Woodhull Medical and Mental Renaissance Health Care Lincoln Medical and Mental Health Center Network Diagnostic Health Center 760 Broadway & Treatment Center 234 East 149th Street Brooklyn, New York 11206 215 West 125th Street Bronx, New York 10451 718-963-8000 New York, New York 10027 718-579-5000 212-932-6500 Manhattan Morrisania Diagnostic Bellevue Hospital Center Queens & Treatment Center 462 First Avenue Elmhurst Hospital Center 1228 Gerard Avenue New York, New York 10016 79-01 Broadway Bronx, New York 10452 212-562-4141 Elmhurst, New York 11373 718-960-2777 Coler Goldwater Specialty 718-334-4000 North Central Bronx Hospital Hospital Queens Hospital Center 3424 Kossuth Avenue Roosevelt Island 82-70 164th Street Bronx, New York 10467 New York, New York 10044 Jamaica, New York 11432 718-519-5000 212-848-6000 718-883-3000 Segundo Ruiz Belvis Diagnostic Gouverneur Healthcare Services & Treatment Center 227 Madison Street Staten Island 545 East 142nd Street New York, New York 10002 Sea View Hospital Bronx, New York 10454 212-238-7000 Rehabilitation Center & Home 718-579-4000 460 Brielle Avenue Harlem Hospital Center Staten Island, New York 10314 506 Lenox Avenue Brooklyn 718-317-3000 New York, New York 10037 Coney Island Hospital 212-939-1000 2601 Ocean Parkway Brooklyn, New York 11235 718-616-30000 Cumberland Diagnostic & Treatment Center 100 North Portland Avenue Brooklyn, New York 11205 718-260-7500 Dr. -

Jacobi Medical Center
. June 10, 2015 Dear Manufacturers, I am writing on behalf of Jacobi Medical Center, 340B ID DSH330127, to inform manufacturers that Jacobi Medical Center recently underwent an audit by the Health Resources and Services Administration (HRSA) of Jacobi Medical Center’s compliance with 340B Drug Pricing Program (340B) requirements. As background, Jacobi Medical Center qualified for the 340B Program as a Disproportionate Share Hospital at 1400 Pelham Parkway South, Bronx, New York 10461 and has participated in the 340B Program since 1992. Through the audit process, Jacobi Medical Center was found to have non-compliance within their 340B Program and responsible for repayment as a result of the following findings: Jacobi Medical Center dispensed 340B drugs to ineligible providers, as prohibited by 42 USC 256b(a)(5)(B). The sample revealed that Jacobi’s contract pharmacies deemed two prescriptions 340B-eligible even though they should not have been eligible. The prescriptions were written by providers at ineligible sites (private offices which were not reimbursable on Jacobi’s Medicare cost report) without an arrangement demonstrating that responsibility of care provided remained at Jacobi. In addition, the auditor found that the 12 month eligibility period did not screen the patient-provider relationship or the patient referral process. It was also noted that the electronic medical record system did not update the billing software, thus allowing the third party pharmacy benefits manager to consider deactivated providers as eligible prescribers. Jacobi Medical Center reversed the 2 prescriptions from contract pharmacies that should not have been eligible, and removed the ineligible providers from Jacobi medical Center’s list of eligible providers. -

Patient Care Delivery
HEALTHCARE BUSINESS INSIGHTS PATIENT CARE DELIVERY Cost & Quality Academy Journal January 2017 Expediting Oncology Care Through Nurse Navigation to Alleviate Patient Challenges Many oncology and cancer programs can be fragmented due to the length of time Greenville Health System South Carolina between patients’ appointments and the number of healthcare professionals they • Number of Licensed Beds: 1,662 need to see before a consensus can be • Hospital Discharges: 51,895 reached about treatment plans. This may cause patients to become anxious and • Number of Cancer Institute Offces: 8 frustrated with their overall experience with oncology care. To help alleviate these navigators’ role in bridging gaps in oncology calm those fears. The nurse navigator is negative care experiences, some health care, The Academy spoke with Julia Yates, critical for a successful visit for the patient systems have expedited the cancer treat- MSN, RN, OCN, Clinical Nurse Manager for and families because they’re procuring ment process with nurse navigators. the multidisciplinary clinic and oncology records, including pathology and imaging Greenville Health System (GHS) Cancer support services, which include nurse navi- studies, and being available to the patient Institute—which has the largest cancer gation services. for education and support.” program in South Carolina and provides Identifying Patient Needs The initial workup for a suspected malig- services to five counties in the state— nancy can involve numerous exams and implemented the use of nurse navigators to “The patient may become very anxious, tests. Waiting for a final diagnosis plan of act as liaisons between patients and treat- especially when they are newly diagnosed care can be a very high-anxiety time for ment providers. -

HOSPITAL SHARPS COLLECTION SITES in NEW YORK STATE As of July 11, 2016
HOSPITAL SHARPS COLLECTION SITES in NEW YORK STATE as of July 11, 2016 No. County Facility Name Address Phone Number Additional information about this site Albany Medical Center Hospital- 43 New Scotland Avenue Saturday 1 ALBANY 518-262-8700 E Building Basement Main Campus Albany, NY 12208 9:00 AM - 1:00 PM Albany Medical Center - South 25 HACKETT BLVD No public drop-off at this site. Drop off site is at Albany Med 2 ALBANY 518-262-1200 Clinical Campus Albany, NY 12208 Main Campus 600 Northern Blvd Albany, NY 12204 3 ALBANY Albany Memorial Hospital 518-471-3221 24/7 Laboratory The community sharps drop box is accessible 24 hrs a day 7 315 South Manning Blvd. 4 ALBANY St Peters Hospital 518-525-1163 24/7 days a week. The drop box is accessible if you park in the Albany, NY 12208 receiving dock and use the walkway to enter the hospital. Monday to Friday 140 West Main Street 5 ALLEGANY Cuba Memorial Hospital Inc 585-968-2000 8:00 AM - 4:00 PM Registration Area Cuba, NY 14727 191 N. Main Street Monday to Friday Memorial Hospital Jones Lobby, Emergency Department , Infection Prevention 6 ALLEGANY Box 72 585-593-1100 8:00 AM-5:00 PM Memorial Hospital Department or at each MD's Practice Andover, NY 14806 Monday to Friday Memorial Hospital Jones 15 Loder Street 9:00 AM - 12:00 PM 7 ALLEGANY 585-596-4101 Main Entrance Memorial Hospital Welsville, NY 14895 1:00 PM - 4:00 PM Monday to Friday 5877 Old State Route 19 Memorial Hospital Jones 9:00 AM - 12:00 PM 8 ALLEGANY Belmont, Wellsville 585-596-2051 Main Entrance Memorial Hospital 1:00 PM - 5:00 -

Directions to Jacobi Medical Center by SUBWAY AND
Directions to Jacobi Medical Center BY SUBWAY AND BUS: IRT EAST SIDE No. 5 Dyre Avenue train to E. 180th Street No. 2 White Plains Road/241st Street train to Pelham Parkway Any No.12 bus directly to Jacobi Medical Center (eastbound) IRT WEST SIDE No. 2 White Plains Road/241st Street train to Pelham Parkway Any No.12 bus directly to Jacobi Medical Center (eastbound) IND 6th AVENUE D train to Fordham Road (Grand Concourse) Any No.12 bus directly to Jacobi Medical Center (eastbound) AMBULATORY CARE PAVILION IRT EAST SIDE No. 5 Dyre Avenue train to E. 180th Street No. 21 bus (Morris Park Avenue) to Seminole Avenue IRT WEST SIDE No. 2 White Plains Road/241st Street train to E. 180th Street No. 21 bus (Morris Park Avenue) to Seminole Avenue BY CAR From Brooklyn: Brooklyn-Queens Expressway to Triborough Bridge to the Bronx. Bear right for the Bruckner Expressway. Follow signs for New Haven (I-95) on the Bruckner and get off at Bronx River Parkway exit. Take Bronx River Parkway north to Pelham Parkway exit. Follow Pelham Parkway east to Jacobi Medical Center, Main Gate. From Queens: Same as Brooklyn or Whitestone Bridge to Hutchinson River Parkway to Pelham Parkway West exit. Take Pelham Parkway west to Eastchester Road. Turn left at Eastchester Road to Morris Park Avenue. Turn right at Morris Park Avenue to Seminole Avenue. -OR- Throggs Neck Bridge to New England Thruway to Pelham Parkway West exit. From Manhattan: F.D.R. to Triborough Bridge to the Bronx bear right for the Bruckner Expressway. -

Residency Appointments 1981-2017
RESIDENCY APPOINTMENTS CLASS OF 1981 Harvey Finkelstein Robert Jacobson Anesthesiology OB-GYN Steven Abrams SUNY at Stony Brook, Mt. Sinai M. C., NY, NY Surgery Teaching Hosp., Stony Brook, Douglas Kahn Montefiore M. C., Bronx, NY NY Surgery Norman Back Barry Gach Buffalo General Hosp., OB-GYN Internal Medicine Buffalo, NY Maimonides M. C., Brooklyn, Washington Hosp. Ctr., Gary Maniloff NY Washington, D.C. Internal Medicine Andrea Bizar-Schneebaum Jay Gewolb Long Island Jewish Hosp., Internal Medicine Anesthesiology New Hyde Park, NY Waterbury Hosp., Waterbury, Yale New Haven Hosp., New Mark Melzer CT Haven, CT Pediatrics/Adolescent David Burton Benjamin Goldman Medicine Pediatrics Internal Medicine Montefiore M. C., Bronx, NY Northwestern University Cleveland Clinic Hosp., Michael Mogerman Children’s Memorial Hosp., Cleveland, OH Psychiatry Chicago, ILL Norman Heching Institute of Living Hosp., Lawrence Cytryn Internal Medicine Hartford, CT Internal Medicine Veterans Administration David Nierman Roosevelt Hosp., NY, NY Hosp., Hines, ILL Internal Medicine Marc Ehrenpreis Gerard Igel Long Island Jewish Hosp., Anesthesiology Pediatrics New Hyde Park, NY Long Island Jewish Hosp., Bronx Municipal Hosp. Ctr., Philip Orbuch New Hyde Park, NY Bronx, NY Dermatology David Ettinger Joseph Irrera NYU M. C., NY, NY Surgery Anesthesiology Dan Orron Buffalo General Hosp., Millard Fillmore Hosp., Radiology Buffalo, NY Buffalo, NY Beth Israel M. C., NY, NY Marc Palter Hallie Weiss Michael Dourmashkin Surgery Internal Medicine Urology Boston University Affiliated V.A. Hosp., NY, NY Montefiore M. C., Bronx, NY Hosp., Boston, MA Bruce Wenig Susan Drucker Lynne Quitell Pathology Pediatrics Pediatrics Mt. Sinai M. C., NY, NY University of MA M. C., Long Island Jewish Hosp., Worcester, MA Kenneth Werner New Hyde Park, NY Family Practice Gary Friedman Lonny Reisman St. -

Art of Caring Brochure:Layout 7.Qxd
Jacobi Medical Center Always the best of care. Now in the best of places. HHC - NYC Health & Hospitals Corporation (nyc.gov) A teaching hospital of the Albert Einstein College of Medicine Sutures, bandages and medicine are the tools that our physicians and caregivers use to restore the body. However, as physicians and caregivers we cannot ignore the power of the mind and the stimulating effect of art in the curative process. Our art...inspires the soul, which in turn heals and rejuvenates the body. Excerpt from The Medicine Of Art A Retrospective of Public Art in the New York City Health and Hospitals Corporation, 1977 For more information on the Art of Caring Campaign, please call 718.918.3827 or e-mail [email protected] Jacobi Medical Center Auxiliary, Inc. 1400 Pelham Parkway South Building 4, 7N5 Bronx, New York 10461 The Art of Caring he Art of Caring Campaign Suggested wording for recognition and dedicatory plaques affixed recognizes that medicine is an on individual pictures includes: Made Possible Through The Tart as much as a science; pays Generosity Of; Donated By; In Honor Of; In Recognition Of; In homage to an extraordinary array of Loving Memory Of; and, Dedicated To. caregivers whose interventions make the critical difference in both saving WAYS TO GET INVOLVED lives and optimizing recovery; and Jacobi Medical Center is supported by the Jacobi Medical Center acknowledges the power of the mind Auxiliary, Inc. a group of very special volunteers that helps to in the curative process, bringing art support and enhance the care provided at our hospital. -
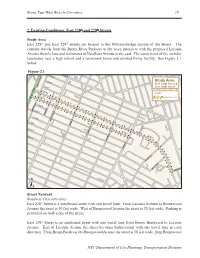
Bronx East-West Bicycle Corridors: Existing Conditions: East 228Th And
Bronx East-West Bicycle Corridors 19 2. Existing Conditions: East 228th and 229th Streets Study Area East 228th and East 229th streets are located in the Williamsbridge section of the Bronx. The corridor travels from the Bronx River Parkway at the west, intersects with the proposed Laconia Avenue bicycle lane and terminates at Needham Avenue to the east. The eastern end of the corridor terminates near a high school and a retirement home and assisted living facility. See Figure 2.1 below. Figure 2.1 E. 232 ST E. 233 ST E. 231 ST Study Area East 228th Street & E. 230 ST BRONX BOULEVARD East 229th Street E. 229 ST LEGEND E. 228 ST Study Corridors E. 227 ST E. 226 ST CARPENTER AV LOWERRE PL E. 225ST WHITE PLAINS RD E. 224 ST BARNES AV E. 223 ST E. 229 RD E. 228 ST BRONXWOOD AV E. 229 ST E. 222 ST PAULDING AV LACONIA AV SCHIEFFELIN AV SCHIEFFELIN PL NEEDHAM AV ± Street Network Roadway Characteristics East 228th Street is a westbound street with one travel lane. From Laconia Avenue to Bronxwood Avenue the street is 30 feet wide. West of Bronxwood Avenue the street is 25 feet wide. Parking is permitted on both sides of the street. East 229th Street is an eastbound street with one travel lane from Bronx Boulevard to Laconia Avenue. East of Laconia Avenue the street becomes bidirectional with one travel lane in each direction. From Bronx Boulevard to Bronxwood Avenue the street is 30 feet wide, from Bronxwood NYC Department of City Planning, Transportation Division 20 Bronx East-West Bicycle Corridors Avenue to Laconia Avenue the street is 33 feet wide, and from Laconia Avenue to Needham Avenue the street is 50 feet wide. -

Carrier Hospital Guide
2021 Carrier Hospital Guide EmblemHealth EmblemHealth EmblemHealth Oscar Oxford Oxford Hospital Name Healthfirst County Prime Select Care Millenium Circle Metro Liberty Albert Einstein College of Medicine √ √ √ √ √ Bronx BronxCare Health System √ √ √ √ Bronx Calvary Hospital √ √ √ √ Bronx Jacobi Medical Center √ √ √ √ √ Bronx Lincoln Medical & Mental Health Center √ √ √ √ √ Bronx Montefiore Medical Center √ √ √ √ Bronx Montefiore Westchester Square √ √ Bronx North Central Bronx Hospital √ √ √ √ √ Bronx St. Barnabas Hospital √ √ √ √ √ √ Bronx Total Hospitals in Bronx County 9 4 4 7 2 7 7 Midhudson Regional Hospital √ √ √ Dutchess Northern Dutchess Hospital √ √ √ √ Dutchess Vassar Brothers Medical Center √ √ √ √ Dutchess Total Hospitals in Dutchess County 3 2 0 0 0 3 3 Brookdale University Hospital Medical Center √ √ √ √ √ Kings Brooklyn Hospital Center √ √ √ √ √ √ √ Kings Coney Island Hospital Center √ √ √ √ √ Kings Interfaith Medical Center √ √ √ √ √ Kings Kings County Hospital Center √ √ √ √ √ Kings Kingsbrook Jewish Medical Center √ √ √ √ √ Kings Maimonides Medical Center √ √ √ Kings Mount Sinai Brooklyn √ √ √ √ √ √ √ Kings NYC Health + Hospitals √ √ √ √ √ Kings New York Community Hospital of Brooklyn √ √ √ √ Kings New York Presbyterian Methodist √ √ √ √ √ Kings NYU Lutheran Medical Center √ √ √ √ Kings SUNY Downstate Medical Center √ √ √ √ Kings Woodhull Medical and Mental Health Center √ √ √ √ √ Kings Wyckoff Heights Medical Center √ √ √ √ Kings Total Hospitals in Kings County 15 6 11 10 3 13 15 Cohen Children's Medical Center √ √ -

Edition of the Norwood News
Proudly Serving Bronx Communities Since 1988 3URXGO\6HUYLQJ%URQ[&RPPXQLWLHV6LQFHFREE 3URXGO\6HUYLQJ%URQ[&RPPXQLWLHV6LQFHFREE 0UQ\YLK*VUZ[Y\J[PVU>VYRLYZ - 5.875” wideORWOOD by 7.0568”Q high EWSQ 3/4 Page NVol. 27, No. 8 PUBLISHED BY MOSHOLU PRESERVATION CORPORATION N April 17–30, 2014 ORWOODQ EWSQ Vol 33, No 3 • PUBLISHED BY MOSHOLU PRESERVATION CORPORATION • JANUARY 30-FEBRUARY 12, 2020 NVol. 27, No. 8 PUBLISHED BY MOSHOLU PRESERVATION CORPORATION N April 17–30, 2014 FREE HSSV[OLY(JJPKLU[=PJ[PTZ We Fight for the Money You Deserve COHEN:Regardless EXPAND of Your Immigration RIGHT Status *VUZ[Y\J[PVU >VYRWSHJL(JJPKLU[Z*HY ;Y\JR(JJPKLU[Z ,SL]H[VY,ZJHSH[VY(JJPKLU[Z5LNSPNLU[)\PSKPUN:LJ\YP[`:SPW;YPW -HSSZ More rentersTO facing4LKPJHS4HSWYHJ[PJL5\YZPUN/VTL5LNSPNLUJL COUNSELeviction could be given representation LAW in Housing Court 7VSPJL)Y\[HSP[`*P]PS9PNO[Z=PVSH[PVUZ Our GUARANTEEBP Diaz Jr. Bows Out Of Mayor’s Race 1/2 Page - 5.875” wide by 4.6875”7KHUHLV1 high O FEE 8QOHVV:H:LQ1/4 Pagepg 2 - Vertical 2XU¿UPKDVUHFRYHUHGRYHU2.8542” wide by 4.6875” high One Hundred Million Dollars LQYHUGLFWVDQGVHWWOHPHQWV IRURXUVDWLV¿HGFOLHQWVNYPD Releases 52nd Precinct-Involved FREE CONSULTATIONShooting Video | pg 6 &DOO+RXUVD'D\'D\VD:HHN Photo by José A. Giralt COUNCILMAN ANDREW COHEN (pictured) speaks Recentat a town hall meetingRecoveries organized by the for Community Clients Action for Safe Apartments (CASA), NorthwestConstruction Bronx Clergy and Coalition Accident (NWBCCC), and Right to Counsel (RTCNYC) in theTruck Mt. Eden sectionAccident of the Bronx on Jan. 15. The event seeks to build support for bills Intro 1529 and Intro 1104 which expand the rights of tenants to receive free legal representation in eviction proceedings.Police Misconduct Elevator Accident 1/8 Page 1/4 ByPage JOSÉ A. -

A Guide to Fitness and Nutrition Programs in the South Bronx
8 Habits of Healthy Kids 1. Spend at least one hour a day being A Guide to Fitness physically active. 2. Limit TV, computer games and the Internet and Nutrition to no more than one hour a day. Programs in the 3. Don’t eat in front of the TV. 4. Drink water instead of soda. South Bronx 5. Eat more fruits and vegetables. 6. Eat less fast food (no more than once a week). Choose smaller portions if you do eat out. 7. Snack on healthy foods and eat less junk food and sweets. 8. Switch to 1% or fat-free dairy products. “The 8 Habits of Healthy Kids” adapted and printed with permission from the Strang Cancer Prevention Center’s “Healthy Children Healthy Futures” program. HPD1X25-22 4.09 The New York City Department of Health & Mental Hygiene Prepared by the New York City Bronx District Public Health Office Bronx, New York 10457 Department of Health & Mental Hygiene ٠ Arthur Avenue 1826 Fax: (718) 299-3334 ٠ Phone: (718) 466-9178 Bronx District Public Health Office For more information about health services and resources available citywide, call 311 Updated Spring 2009 A Guide to Fitness & Nutrition Programs in the South Bronx Physical Activity & Nutrition Resources on the Web Web Resources Action for Healthy Kids Kids Health for Parents www.actionforhealthykids.org http://kidshealth.org/parent/nutrition_fit/ center/nutrition_center.html American Alliance for Health, Table of Contents National Association for Sport Introduction Introduction Phys. Education, Recreation & Dance www.aahperd.org & Physical Education www.aahperd.org American Cancer