WCCF Notes – 18.10.19 FINAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Policy Forum (NPF) Report 2018
REPORT 2018 @LabPolicyForum #NPFConsultation2018 National Policy Forum Report 2018 XX National Policy Forum Report 2018 Contents NPF Elected Officers ....................................................................................................................4 Foreword ........................................................................................................................................5 About this document ...................................................................................................................6 Policy Commission Annual Reports Early Years, Education and Skills ............................................................................................7 Economy, Business and Trade ............................................................................................. 25 Environment, Energy and Culture ....................................................................................... 39 Health and Social Care ........................................................................................................... 55 Housing, Local Government and Transport ..................................................................... 71 International ............................................................................................................................. 83 Justice and Home Affairs ....................................................................................................... 99 Work, Pensions and Equality ..............................................................................................119 -

MINUTES of the PARISH COUNCIL MEETING HELD on MONDAY 23Rd NOVEMBER 2015 at 7.30Pm RE-SCHEDULED from 16Th NOVEMBER 2015
MINUTES OF THE PARISH COUNCIL MEETING HELD ON MONDAY 23rd NOVEMBER 2015 AT 7.30pm RE-SCHEDULED FROM 16th NOVEMBER 2015 PRESENT; Mr A Marr (Chairman), Mr W Douglas, Mr W Bradley, Mr R Hart, Mr A Jones, Mrs P Jones, Mr J Kendall APOLOGIES: P.C.S.O. Peter Crome ALSO PRESENT; Mr G Proud, Mr L Parker, Mrs E Parker, Councillor A J Markley REQUESTS FOR DISPENSATION; None. DECLARATION OF INTERESTS; None. PUBLIC PARTICIPATION SESSION; Mr G Proud raised the question re. grass cutting at the south end of the village; when it is cut could it be picked up? It was felt that as there are Natterjack Toads in the area this may not be possible. Mr J Kendall said can Chairman ensure matters are strictly enforced unlike the last meeting. At this point Mr & Mrs Parker entered the meeting. Mrs Parker said the Friends of Allonby Green are putting in for a grant for new picnic tables and seats and they want Parish Council to find out what would be in order. These would become the property of the Parish Council she said. It was felt they should be made of re-cycled plastic. The AONB and A.B.C. to be asked what would be in order. Mrs Parker said they also want a couple of seats by the toilets. MINUTES; Minutes of the Parish Council meeting held on 19th October and special meeting on 27th October2015 were agreed and signed as a true record. MATTERS ARISING; Toilets at West End – A meeting with Mr D Bryden, A.B.C. -

THE 422 Mps WHO BACKED the MOTION Conservative 1. Bim
THE 422 MPs WHO BACKED THE MOTION Conservative 1. Bim Afolami 2. Peter Aldous 3. Edward Argar 4. Victoria Atkins 5. Harriett Baldwin 6. Steve Barclay 7. Henry Bellingham 8. Guto Bebb 9. Richard Benyon 10. Paul Beresford 11. Peter Bottomley 12. Andrew Bowie 13. Karen Bradley 14. Steve Brine 15. James Brokenshire 16. Robert Buckland 17. Alex Burghart 18. Alistair Burt 19. Alun Cairns 20. James Cartlidge 21. Alex Chalk 22. Jo Churchill 23. Greg Clark 24. Colin Clark 25. Ken Clarke 26. James Cleverly 27. Thérèse Coffey 28. Alberto Costa 29. Glyn Davies 30. Jonathan Djanogly 31. Leo Docherty 32. Oliver Dowden 33. David Duguid 34. Alan Duncan 35. Philip Dunne 36. Michael Ellis 37. Tobias Ellwood 38. Mark Field 39. Vicky Ford 40. Kevin Foster 41. Lucy Frazer 42. George Freeman 43. Mike Freer 44. Mark Garnier 45. David Gauke 46. Nick Gibb 47. John Glen 48. Robert Goodwill 49. Michael Gove 50. Luke Graham 51. Richard Graham 52. Bill Grant 53. Helen Grant 54. Damian Green 55. Justine Greening 56. Dominic Grieve 57. Sam Gyimah 58. Kirstene Hair 59. Luke Hall 60. Philip Hammond 61. Stephen Hammond 62. Matt Hancock 63. Richard Harrington 64. Simon Hart 65. Oliver Heald 66. Peter Heaton-Jones 67. Damian Hinds 68. Simon Hoare 69. George Hollingbery 70. Kevin Hollinrake 71. Nigel Huddleston 72. Jeremy Hunt 73. Nick Hurd 74. Alister Jack (Teller) 75. Margot James 76. Sajid Javid 77. Robert Jenrick 78. Jo Johnson 79. Andrew Jones 80. Gillian Keegan 81. Seema Kennedy 82. Stephen Kerr 83. Mark Lancaster 84. -

FDN-274688 Disclosure
FDN-274688 Disclosure MP Total Adam Afriyie 5 Adam Holloway 4 Adrian Bailey 7 Alan Campbell 3 Alan Duncan 2 Alan Haselhurst 5 Alan Johnson 5 Alan Meale 2 Alan Whitehead 1 Alasdair McDonnell 1 Albert Owen 5 Alberto Costa 7 Alec Shelbrooke 3 Alex Chalk 6 Alex Cunningham 1 Alex Salmond 2 Alison McGovern 2 Alison Thewliss 1 Alistair Burt 6 Alistair Carmichael 1 Alok Sharma 4 Alun Cairns 3 Amanda Solloway 1 Amber Rudd 10 Andrea Jenkyns 9 Andrea Leadsom 3 Andrew Bingham 6 Andrew Bridgen 1 Andrew Griffiths 4 Andrew Gwynne 2 Andrew Jones 1 Andrew Mitchell 9 Andrew Murrison 4 Andrew Percy 4 Andrew Rosindell 4 Andrew Selous 10 Andrew Smith 5 Andrew Stephenson 4 Andrew Turner 3 Andrew Tyrie 8 Andy Burnham 1 Andy McDonald 2 Andy Slaughter 8 FDN-274688 Disclosure Angela Crawley 3 Angela Eagle 3 Angela Rayner 7 Angela Smith 3 Angela Watkinson 1 Angus MacNeil 1 Ann Clwyd 3 Ann Coffey 5 Anna Soubry 1 Anna Turley 6 Anne Main 4 Anne McLaughlin 3 Anne Milton 4 Anne-Marie Morris 1 Anne-Marie Trevelyan 3 Antoinette Sandbach 1 Barry Gardiner 9 Barry Sheerman 3 Ben Bradshaw 6 Ben Gummer 3 Ben Howlett 2 Ben Wallace 8 Bernard Jenkin 45 Bill Wiggin 4 Bob Blackman 3 Bob Stewart 4 Boris Johnson 5 Brandon Lewis 1 Brendan O'Hara 5 Bridget Phillipson 2 Byron Davies 1 Callum McCaig 6 Calum Kerr 3 Carol Monaghan 6 Caroline Ansell 4 Caroline Dinenage 4 Caroline Flint 2 Caroline Johnson 4 Caroline Lucas 7 Caroline Nokes 2 Caroline Spelman 3 Carolyn Harris 3 Cat Smith 4 Catherine McKinnell 1 FDN-274688 Disclosure Catherine West 7 Charles Walker 8 Charlie Elphicke 7 Charlotte -

(Public Pack)Agenda Document for County Council Local Committee
Corporate, Customer and Community Services Directorate Legal and Democratic Services Cumbria House 117 Botchergate Carlisle CA1 1RD Tel 01228 606060 Email [email protected] 5 November 2018 To: The Chair and Members of the County Council Local Committee for Carlisle Agenda COUNTY COUNCIL LOCAL COMMITTEE FOR CARLISLE A meeting of the County Council Local Committee for Carlisle will be held as follows: Date: Tuesday 13 November 2018 Time: 10.00 am Place: Conference Room A/B, Cumbria House, Botchergate, Carlisle, CA1 1RD Dawn Roberts Executive Director – Corporate, Customer and Community Services NB THERE WILL BE A PRIVATE MEMBER BRIEFING ON THE RISING OF THE COMMITTEE REGARDING S106/DEVELOPER CONTRIBUTIONS Group Meetings: Labour: 9.00am Cabinet Meeting Room Conservative: 9.30am Conservative Group Office Independent: 9.00am Independent Meeting Room Enquiries and requests for supporting papers to: Lynn Harker Direct Line: 01228 226364 / 07825340229 Email: [email protected] This agenda is available on request in alternative formats Serving the People of Cumbria MEMBERSHIP Conservative (7) Labour (8) Independent Councillors (Non Aligned) (2) Mr GM Ellis Mr J Bell Mr RW Betton Mr LN Fisher Mrs C Bowditch Mr W Graham Dr S Haraldsen Ms D Earl Mrs EA Mallinson Dr K Lockney Mr J Mallinson (Vice-Chair) Mr A McGuckin Mr NH Marriner Mr R Watson Mrs V Tarbitt Mr SF Young Mr C Weber (Chair) Liberal Democrat (1) Mr T Allison ACCESS TO INFORMATION Agenda and Reports Copies of the agenda and Part I reports are available for members of the public to inspect prior to the meeting. -

Social Diary Workington
Activities and Social Groups in the Workington Area ‘Part of the Cumbria Health and Social Wellbeing System’ supported by Cumbria County Council This social diary provides information on opportunities in the local community and on a wide range of services. It is listed by days activities. Arts and Crafts Clubs: Art Class Lamplugh Village Hall, Lamplugh, weekly Thursdays 3.00-5.30pm, Water colour and Drawing classes for all abilities, NEED TO BOOK. Contact Sandra Cooper: 01946 861416 Art Class Harrington Youth Club, Church Road, weekly Thursdays 10.00am- 12.00pm (term-time only). Contact Sheila Fielder: 01946 831199 or [email protected] Art Class Distington Community Centre, Church Road, Distington, weekly Tuesdays 6.15-8.15pm. Contact the centre: 01946 834297 Craft and Chat The Oval Centre, Salterbeck. Everyone is welcome. Every Friday 11am –3:00pm. For more information contact Oval Centre: 01946 834713 Craft Club Distington Community Centre, Church Road, Distington, weekly Tuesdays 1.00-3.00pm. Contact: Distington Community Centre: 01946 834297 Crafty Corner Moorclose Library, Moorclose campus, Needham Drive, Workington, fortnightly alternate Tuesdays 2.00-4.00pm. Contact the Library: 01900 602736 Craft Night Knitting, crochet, Helena Thompson Museum, Park End Road, Workington, monthly 1st Thursday of month 7.00-9.00pm, £3. Contact the Museum: 01900 64040 Embroidery Helena Thompson Museum, Park End Road, Workington, weekly Mondays 10.00am - 3.00pm. Contact The museum: 01900 64040 Knit & Natter Moorclose Community Centre, Workington, weekly Monday 1.00- 3.00pm, Social and crafts. Contact the Centre: 01900 871789 Knit & Natter Distington Community Centre, Church Road, Distington, weekly Fridays 1.00-3.00pm. -

Labour Party General Election 2017 Report Labour Party General Election 2017 Report
FOR THE MANY NOT THE FEW LABOUR PARTY GENERAL ELECTION 2017 REPORT LABOUR PARTY GENERAL ELECTION 2017 REPORT Page 7 Contents 1. Introduction from Jeremy Corbyn 07 2. General Election 2017: Results 11 3. General Election 2017: Labour’s message and campaign strategy 15 3.1 Campaign Strategy and Key Messages 16 3.2 Supporting the Ground Campaign 20 3.3 Campaigning with Women 21 3.4 Campaigning with Faith, Ethnic Minority Communities 22 3.5 Campaigning with Youth, First-time Voters and Students 23 3.6 Campaigning with Trade Unions and Affiliates 25 4. General Election 2017: the campaign 27 4.1 Manifesto and campaign documents 28 4.2 Leader’s Tour 30 4.3 Deputy Leader’s Tour 32 4.4 Party Election Broadcasts 34 4.5 Briefing and Information 36 4.6 Responding to Our Opponents 38 4.7 Press and Broadcasting 40 4.8 Digital 43 4.9 New Campaign Technology 46 4.10 Development and Fundraising 48 4.11 Nations and Regions Overview 49 4.12 Scotland 50 4.13 Wales 52 4.14 Regional Directors Reports 54 4.15 Events 64 4.16 Key Campaigners Unit 65 4.17 Endorsers 67 4.18 Constitutional and Legal services 68 5. Labour candidates 69 General Election 2017 Report Page 9 1. INTRODUCTION 2017 General Election Report Page 10 1. INTRODUCTION Foreword I’d like to thank all the candidates, party members, trade unions and supporters who worked so hard to achieve the result we did. The Conservatives called the snap election in order to increase their mandate. -

(Public Pack)Agenda Document for Scrutiny Management Board, 23/01
Resources Legal and Democratic Services The Lonsdale Building The Courts Carlisle Cumbria CA3 8NA Fax 01228 226372 Tel 01228 606060 Email [email protected] To: The Chair and Members of the Scrutiny Management Board Agenda SCRUTINY MANAGEMENT BOARD A meeting of the Scrutiny Management Board will be held as follows: Date: Friday, 23 January 2015 Time: 10.00 am Place: Committee Room 2, The Courts, Carlisle NB A PRE-MEETING OF THE BOARD WILL BE HELD AT 9.30AM IN COMMITTEE ROOM 2 TO WHICH ALL MEMBERS ARE ENCOURAGED TO ATTEND. Dawn Roberts Assistant Director – Corporate Governance Enquiries and requests for supporting papers to: Glynis Andrews Direct Line: 01228 226361 Email: [email protected] This agenda is available on request in alternative formats Serving the People of Cumbria 1 MEMBERSHIP Conservative (5) Labour (6) Mr DS Fairbairn Mr KR Hamilton Mr J Lister Mr M Hawkins Mr D Roberts Mrs S Hayman Mrs V Tarbitt Mr J Murphy (Vice-Chair) Mr WJ Wearing (Chair) Ms C Wharrier Mr M Wilson Liberal Democrat (3) Mr D Fletcher Mrs BC Gray Mr R Wilson ACCESS TO INFORMATION Agenda and Reports Copies of the agenda and Part I reports are available for members of the public to inspect prior to the meeting. Copies will also be available at the meeting. The agenda and Part I reports are also available on the County Council’s website – www.cumbria.gov.uk Background Papers Requests for the background papers to the Part I reports, excluding those papers that contain exempt information, can be made to Legal and Democratic Services at the address overleaf between the hours of 9.00 am and 4.30 pm, Monday to Friday. -

Review of Workington Community Action Plan
Review of Workington Community Action Plan January 2002 to August 2003 Covering the Neighbourhood Forum areas of Harrington & Salterbeck Moorclose & Westfield Workington Central Review of Workington Community Action Plan Contents Section I Introduction Page 2 Section II Workington Regeneration Strategy Page 4 Section III Neighbourhood Forum Structure Page 5 Section IV Community Action Plans Page 6 Section V Forum Priorities Page 8 Section VI Community Chest Grants Page 9 Section VII Role of the Healthy Communities Page 12 Focus Group Diagrams and tables 4.9 Review of Community Action Plans Page 7 6.8 Process for Application to the Page 10 Community Chest Fund 6.9 Summary of Grants made by the Page 11 Community Chest Appendices Appendix 1 Discussion of forum priorities in; Pages Harrington & Salterbeck Forum 13 Moorclose & Westfield Forum 16 Workington Central Forum 19 Appendix 2 Information on Grants to; Pages Harrington & Salterbeck Forum 21 Moorclose & Westfield Forum 26 Workington Central Forum 30 1 Section I I. Introduction 1.1 This document is an update of the 2002 Workington Community Action Plan, and covers the period from January 2002 to August 2003. The Community Action Plan reflects the views of local people who are involved in the three Neighbourhood Forums that cover the Workington area which are Workington Central, Harrington & Salterbeck, Moorclose & Westfield. 1.2 Community Action Plans were developed as a means of informing the Regeneration Programme in Workington. The Workington Partnership successfully applied for £7.5 million from the Single Regeneration Budget (SRB) in June 2000 to address the problems of; Long term and consistently high levels of unemployment and joblessness Significant inequalities in both health and education attainment in the most disadvantaged wards The fear of crime, levels of poverty and the widespread environmental deficit throughout the urban area Low levels of community engagement and available support so that local groups have the capacity and leadership to revive their own neighbourhoods. -
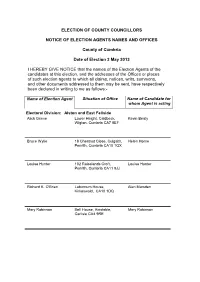
Notice of Election Agents Names and Offices
ELECTION OF COUNTY COUNCILLORS NOTICE OF ELECTION AGENTS NAMES AND OFFICES County of Cumbria Date of Election 2 May 2013 I HEREBY GIVE NOTICE that the names of the Election Agents of the candidates at this election, and the addresses of the Offices or places of such election agents to which all claims, notices, writs, summons, and other documents addressed to them may be sent, have respectively been declared in writing to me as follows:- Name of Election Agent Situation of Office Name of Candidate for whom Agent is acting Electoral Division: Alston and East Fellside Alick Grieve Lower Height, Caldbeck, Kevin Beaty Wigton, Cumbria CA7 8EF Bruce Wylie 18 Chestnut Close, Culgaith, Helen Horne Penrith, Cumbria CA10 1QX Louisa Hunter 102 Raiselands Croft, Louisa Hunter Penrith, Cumbria CA11 9JJ Richard K. O'Brien Laburnum House, Alan Marsden Kirkoswald, CA10 1DQ Mary Robinson Bell House, Ainstable, Mary Robinson Carlisle CA4 9RE Name of Election Agent Situation of Office Name of Candidate for whom Agent is acting Electoral Division: Appleby Paul M. Trollope Acland House, Yard 2, Denise Bell Stricklandgate, Kendal LA9 4ND Alick Grieve Lower Height, Caldbeck, Martin Stephenson Wigton, Cumbria CA7 8EF Michael E.L. Williams Castle Bank, Appleby-in- Michael Williams Westmorland, Cumbria CA16 6SN Electoral Division: Aspatria Clive Jefferson. British National Party, PO Chris Barnett Box 213, Wigton CA7 7AL Barbara Cannon Workington Labour Party, Denise Coe Room 1, Trades Hall Centre, 39 Brow Top, Workington CA14 2DP William Finlay 2 East Crescent, Aspatria, Bill Finlay CA7 3EF Joseph Cowell Fionaville, Lowmoor Road, Jim Lister Wigton CA7 9QP Paul M. -

Green Shoots
FABIAN REVIEW The quarterly magazine of the Fabian Society Summer 2019 / fabians.org.uk / £4.95 GREEN SHOOTS Ideas for greening Labour from Ed Miliband, Sue Hayman, Judith Blake, Nadia Whittome and more p / Harriet Harman on a national scandal p / Stephen Carter gets to grips with our Brexistential crisis p Fabian membership + donation For members who are in a position to give more to the society we offer three tiers of membership plus donation: COLE membership plus donation – £10 / month All the benefits of standard membership plus: a Fabian Society branded canvas bag; a free ticket to either our new year or summer conference; invitation to an annual drinks reception; and regular personal updates from the general secretary. CROSLAND membership plus donation – £25 / month All the benefits of COLE plus: free tickets to all Fabian events; a printed copy of every Fabian report, sent to your home; and invitations to political breakfasts with leading figures on the left. WEBB membership plus donation – £50 / month All the benefits of CROSLAND plus: regular personal updates from leading Fabian parliamentarians; an annual dinner with the general secretary and Fabian parliamentarians; and special acknowledgement as a patron in our annual report and on our website. For more information & to donate visit fabians.org.uk/donate Contents FABIAN REVIEW Volume 131 —No.2 Leader Andrew Harrop 4 Feeling blue Shortcuts Sara Hyde and Paula Harriott 5 A just cause Lloyd Russell-Moyle MP 6 Cuts and closures Chaitanya Kumar 6 Secularism’s last stand Stephanie -

News in CHARM -‐ September 2016 Cumbrian Health Centres Welcome
News in CHARM - September 2016 Cumbrian Health Centres welcome visit from lead Politician Parliamentary under secretary of state for community health and care, David Mowat, visited Morecambe Bay on Tuesday to learn more about the Better Care Together strategy. He was travelling to Millom for a tour of the community hospital and GP surgery. He had a first-hand experience of a teleconsultation appointment using a high-definition camera and monitor which is linked to the facility in the emergency department. Mr Mowat was impressed by the facilities available and paid tribute to the determination of Millom residents. He said: "It's all about creating new models of care in the NHS. We have established around 40 or 50 vanguard sites that are trying things which are a bit different. They are exemplars of practice and Millom is one of them." Mr Mowat got to meet representatives of the Millom Alliance community group known as the Millom Health Action Group who told him about their community-led initiatives over a working lunch. Read more Campaign group vow never to stop the fight to save hospital CAMPAIGNERS fighting to save Ringwood's community hospital vow that they "will never give up." And the Friends of St Leonards Hospital are amassing an army of volunteers to do battle and help save the hospital from closing. It was revealed that St Leonards, Alderney and Westhaven hospitals have been recommended for closure by NHS Dorset Clinical Commissioning Group (CCG). Chairman of the Friends of St Leonards, Jacqueline Moss expressed her fury that members only learned about the closure plans via Facebook.