Quintessence Journals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

ADA Statement on Dental Patient Rights and Responsibilities
ADA Statement on Dental Patient Rights and Responsibilities Background: The ADA Council on Ethics, Bylaws and Judicial Affairs (CEBJA) has developed the following template Dental Patient Rights and Responsibilities Statement (DPRR Statement) as a guide and as an aid to be used by constituent and component societies and practitioners in creating their own dental patients rights and responsibilities statements. In the DPRR Statement that follows, the term “rights” is used not in a legal sense, but merely to convey an indication that a patient should have an expectation of experiencing treatment in accordance with the enumerated “rights.” Several other dental and medical related organizations publish patient rights statements; indeed, CEBJA reviewed those statements during the development of the DPRR Statement, as well as Standard 5-3 of the ADA Commission on Dental Accreditation (CODA) Standards for Predoctoral Dental Education Programs, which also refers to a statement of patients’ rights. The DPRR Statement grew out of a collaborative ethics summit conducted in March 2006 by the American College of Dentists (ACD) and the American Dental Association (ADA) on the topic of commercialism in dentistry. Members of CEBJA were invited to attend along with representatives from ADA and ACD leadership, the ADA Council on Dental Education and Licensure, the recognized specialty groups, the National Dental Association, the U.S. Department of Veterans Affairs, the American Dental Education Association, dental school deans and faculty, ethicists, dental editors and leading representatives from the insurance, practice management and dental product manufacturers industry. The summit attendees noted that patients have become more assertive in seeking elective procedures and that the dental profession seeks to be mindful of protecting patient autonomy while balancing the importance of overall dental health and lifelong consequences. -

Dental Implants Placement of Dental Implants Is a Procedure, Not an American Dental Association (ADA) Recognized Dental Specialty
Dental Implants Placement of dental implants is a procedure, not an American Dental Association (ADA) recognized Dental Specialty. Dental implants like all dental procedures require dental education and training. Implant therapy is a prosthodontic procedure with radiographic and surgical components. Using a dental implant to replace missing teeth is dictated by individual patient needs as determined by their dentist. An implant is a device approved and regulated by the FDA, which can provide support for a single missing tooth, multiple missing teeth, or all teeth in the mouth. The prosthodontic and the surgical part of implant care can each range from straightforward to complex. A General Dentist who is trained to place and restore implants may be the appropriate practitioner to provide care for dental implant procedures. This will vary depending on an individual clinician’s amount of training and experience. However, the General Dentist should know when care should be referred to a specialist (a Prosthodontist, a Periodontist or an Oral and Maxillofacial Surgeon). Practitioners should not try to provide care beyond their level of competence. Orthodontists may place and use implants to enable enhanced tooth movement. Some Endodontists may place an implant when a tooth can’t be successfully treated using endodontic therapy. Maxillofacial Prosthodontists may place special implants or refer for placement when facial tissues are missing and implants are needed to retain a prosthesis. General Dentists are experienced in restorative procedures, and many have been trained and know requirements for the dental implant restorations they provide. However, if a patient’s implant surgical procedure is beyond the usual practice of a dentist, this part of the care should be referred to another dentist that is competent in placement of implants. -
Restrictive Diets and Oral Health What Youdo Need to Iknow Need to Floss?
spring/summerwinter 20172018 Vegan Gluten Free Lactose Free Restrictive Diets and Oral Health What YouDo Need to IKnow Need to Floss? PLEASEPLEASE DO DO NOT NOT REMOVE REMOVE FROM FROM RECEPTION RECEPTION AREA. AREA. VisitVisit usus onlineonline youroralhealth.cayouroralhealth.ca A valuable resource for your patients. BROUGHT TO YOU BY THE ONTARIO DENTAL ASSOCIATION CONTENTS Winter 2018 4 WELCOME Publisher Dr. Deborah Saunders Marcus Staviss Editor-In-Chief Dr. Deborah Saunders 5 OUR CONTRIBUTORS Consulting Editor 6 Dr. Ian McConnachie 6 VITAMINS, MINERALS AND NUTRIENTS Editor The impact of restrictive diets Julia Kuipers on your oral health. Creative and Graphic Design Specialist Catherine Solmes Natalia Ivashchenko Graphic Designer SIT TIGHT Ananya Bhattasali 9 The dental chair through the ages. Policy Editor Roberta MacLean Catherine Morana Copy Editor and Proofreader Jennifer D. Foster 12 IMMUNE SYSTEM DISORDERS And their effects on your oral health. Advisory Board 12 President, ODA Bonnie Dean Dr. LouAnn Visconti President-Elect, ODA 14 ASK YOUR DENTIST! Dr. David Stevenson Questions dentists want you to ask about oral health. Vice-President, ODA Donna Paris Dr. Kim Hansen Past-President, ODA 18 DORM DENTAL DANGERS Dr. Jack McLister Why a toothache should never be part of the curriculum. Advertising For more information about advertising or sponsorship Maggie Blood opportunities for YourOralHealth.ca Brought to You by the 18 ODA, please contact Jennifer DiIorio or Gillian Thomas at Dovetail Communications at 905-886-6640 or 20 ORAL MAXILLOFACIAL [email protected] or [email protected]. REHABILITATION PROGRAM Rehabilitating patients from the inside out. Disclaimer The publication of an article or advertisement Sophie Lamoureux should not be construed as an endorsement of or approval by the ODA. -

Annual Report 2013
Annual Report 2013 “ Being active and having a positive outlook on life is what keeps me going every day.” Overview of 2013 “ Our performance in 2013 was defined by remarkable &R D output and further delivery of sustained financial performance for our shareholders.” Please go to page 4 for more More at gsk.com Performance highlights £26.5bn £8.0bn £7.0bn £5.2bn Group turnover Core* operating profit Total operating profit Returned to shareholders 6 112.2p 112.5p 13% Major medicines approved Core* earnings per share Total earnings per share Estimated return on R&D investment 10 6 1st 1st Potential phase III study starts in 2014/15 Potential medicines with phase III data in Access to Medicines Index Pharmaceutical company to sign AllTrials expected 2014/15 campaign for research transparency Front cover story Betty, aged 65, (pictured) has Chronic “ Health is important to me, Obstructive Pulmonary Disease (COPD). She only has 25% lung capacity. This means I try to take care of my she finds even everyday tasks difficult, but medicines and inhaled oxygen allow her to health with all the tools live as normal a life as she can. Betty’s mindset I have and do the best is to stay busy and active, so every week she goes to rehab exercise classes. that I can with it.” COPD is a disease of the lungs that leads to Betty, COPD patient, damaged airways, causing them to become North Carolina, USA narrower and making it harder for air to get in and out. 210 million people around the world are estimated to have COPD. -

Women's Oral Health Issues
ORAL HEALTH CARE SERIES Women’s Oral Health Issues November 2006 American Dental Association Council on Access, Prevention and Interprofessional Relations success.ada.org FOREWORD Women’s Oral Health Issues has been developed by the American Dental Association’s Council on Access, Prevention and Interprofessional Relations (CAPIR) Women’s Oral Health Issues is one volume in the Oral Health Care Series that has been developed to assist in the treatment of individuals with complex medical conditions. The Oral Health Care Series began in 1986 and was based on Clinical Care Guidelines for the Dental Management of the Medically Compromised Patient (1985, revised in 1990) developed by the Veterans Health Administration, Department of Veterans Affairs. Since that time, the Oral Health Care Series Workgroup enhanced the documents to provide information on treating the oral health of patients with complex medical conditions. Disclaimer Publications in the Oral Health Care Series, including Women’s Oral Health Issues, are offered as resource tools for dentists and physicians, as well as other members of the health care team. They are not intended to set specific standards of care, or to provide legal or other professional advice. Dentists should always exercise their own professional judgment in any given situation, with any given patient, and consult with their professional advisors for such advice. The Oral Health Care Series champions consultation with a patient’s physician as indicated, in accordance with applicable law. success.ada.org 2 ACKNOWLEDGEMENTS The Council acknowledges the pioneering efforts of the original Ad Hoc Committee of 1986: William Davis, DDS, MS; Ronald Dodson, DDS; Leon Eisenbud, DDS; Martin Greenberg, DDS; Felice O’Ryan, DDS, MS; David A. -
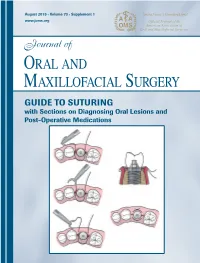
GUIDE to SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications
Journal of Oral and Maxillofacial Surgery Journal of Oral and Maxillofacial August 2015 • Volume 73 • Supplement 1 www.joms.org August 2015 • Volume 73 • Supplement 1 • pp 1-62 73 • Supplement 1 Volume August 2015 • GUIDE TO SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications INSERT ADVERT Elsevier YJOMS_v73_i8_sS_COVER.indd 1 23-07-2015 04:49:39 Journal of Oral and Maxillofacial Surgery Subscriptions: Yearly subscription rates: United States and possessions: individual, $330.00 student and resident, $221.00; single issue, $56.00. Outside USA: individual, $518.00; student and resident, $301.00; single issue, $56.00. To receive student/resident rate, orders must be accompanied by name of affiliated institution, date of term, and the signature of program/residency coordinator on institution letter- head. Orders will be billed at individual rate until proof of status is received. Prices are subject to change without notice. Current prices are in effect for back volumes and back issues. Single issues, both current and back, exist in limited quantities and are offered for sale subject to availability. Back issues sold in conjunction with a subscription are on a prorated basis. Correspondence regarding subscriptions or changes of address should be directed to JOURNAL OF ORAL AND MAXILLOFACIAL SURGERY, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Telephone: 1-800-654-2452 (US and Canada); 314-447-8871 (outside US and Canada). Fax: 314-447-8029. E-mail: journalscustomerservice-usa@ elsevier.com (for print support); [email protected] (for online support). Changes of address should be sent preferably 60 days before the new address will become effective. -

Dental Erosion and GORD - Gastro Oesophageal Reflux Disorder
Clinical Dental erosion and GORD - Gastro Oesophageal Reflux Disorder Louis Z G Touyz, 1 Antoni Anouf, Amirfirooz Borjian, Claudia Ferrari Abstract Acid erosion of teeth from extrinsic sources, such as acidic beverages, renders damage to teeth with characteristic erosive patterns developing. Gastro Oesophageal Reflux Disorder (GORD) is frequently cited as a stand alone condition causing dental palatal erosion. It is often referred to as Gastro Oesophageal Reflux Disease GORD or GERD. GORD is a patho- physiological disorder rather than a disease, as GORD is not contagious, infectious or transmissible through contact. GORD is a common condition universally affecting many people, mainly young females. Etiologies embrace eating disorders including bulimia and anorexia nervosa, dysfunctional oesophageal sphincters allowing acid gastric juice migration into the mouth, chronic alcoholism and pregnancy. GORD is also responsible for tooth erosion, but generally manifests destruction on the palatal side of dental crowns. This article describes cases of typical tooth erosion deriving from GORD and acid beverages, compares the two and principles of therapy are outlined. Introduction Tooth erosion from acids may be caused by intrinsic and Intrinsic factors causing dental erosion extrinsic factors. Gastro Oesophageal Reflux Disorder Eating disorders (GORD) with Erosion is prime among intrinsic factors. Prime among common eating disorders that manifest Hydrochloric acid (HCl) is produced in the gastric mucosa GORD are bulimia, anorexia, alcoholism, rumination and by parietal cells. Etiologies of GORD include eating alcoholism. disorders like bulimia and anorexia nervosa, rumination, Bulimia nervosa, a common eating disorder mainly chronic alcoholism, pregnancy and other conditions with among young women, in which affected people routinely dysfunctional oesophageal sphincters, which allow acid and regularly induce post-prandial emesis, has long been gastric juices to migrate into the mouth. -

Graduate Program in Dental Public Health
GRADUATE PROGRAM IN DENTAL PUBLIC HEALTH Advanced Training Program The Department of Preventive and Community Dentistry offers an advanced training program in dental public health. The specialty of dental public health is one of the nine dental specialties formally recognized by the American Dental Association. The dental public health training program at the College of Dentistry fulfills all of the educational requirements for dentists wishing to complete the board-certifying examination given by the American Board of Dental Public Health. The graduate program in dental public health offers advanced training for both dentists and dental hygienists who are interested in careers in dental academic settings or dental public health administration. The program requires two years of full-time study and culminates in the awarding of a Master of Science (M.S.) degree in dental public health. The training program places an emphasis on research and includes the preparation and defense of a master's thesis. A minimum of 40 semester hours of coursework is required, including several electives. Most required courses are taken within the College of Dentistry, but some required courses and elective courses are taken through the Colleges of Public Health, Medicine, Education, Business Administration or Liberal Arts. The program provides instruction in the 10 competency areas defined by the American Board of Dental Public Health. (See Altman, D. and Mascarenhas, A. K. (2016), New competencies for the 21st century dental public health specialist. Journal of Public Health Dentistry, 76: S18–S28. doi:10.1111/jphd.12190): 1. Manage oral health programs for population health. 2. Evaluate systems of care that impact oral health. -

Orthodontics and Surgery
When Treatment Calls For A Specialized Partnership: Orthodontics And Surgery 401 North Lindbergh Boulevard Saint Louis, Missouri 63141-7816 www.braces.orgwww.braces.org 401© 2009 North American Lindbergh Association of Orthodontists Boulevard Saint Louis, Missouri 63141-7816 The American Association1-800-STRAIGHT of Orthodontists thanks the faculty and staff representing Orthodontics, Center for Advanced Dental Education, Saint Louis University for their invaluable guidance, generosity, and the use of© their American facilities Association during the of production Orthodontists, of this 19992000 brochure. The upper and lower About the AAO: jaws are the foundations by which teeth are Founded in 1900, the American supported. Sometimes, Association of Orthodontists (AAO) when the jaws are has more than 15,500 members. Active too short or long, AAO members limit their practices to the too wide or narrow, braces dental specialty of Orthodontics and alone can’t completely correct Dentofacial Orthopedics. Orthodontists a bad bite. And, in addition to affecting are dental specialists with at least a person’s appearance, an improper bite can lead to serious problems, such as abnormal tooth wear, two years of advanced orthodontic periodontal disease, and possible joint pain. education after dental school. Orthodontists correct crooked teeth and bad bites. For problems related to jaw formation and misalignment (skeletal problems), an oral surgeon may be needed. The purposes of the American When both conditions come into play, it’s common for an orthodontist and oral surgeon to work together. Association of Orthodontists and Some severe cases can only be corrected with a its member orthodontists are: combination of orthodontics and surgery. -

Dental Implants
dental implants for tooth replacement be a confident you smile big why replace missing teeth? Losing one or more of your teeth creates a gap in your smile, affects your ability to chew properly, and can alter your diet and nutrition. In addition to these serious issues, tooth loss also causes bone loss. Anyone missing one or more teeth understands how tooth loss can make you feel uncomfortable about smiling or eating in tooth loss causes bone loss public. You may avoid social situations and as a result begin to feel isolated. This could impact your daily life and your self-confidence. When a tooth is lost, the jawbone beneath it shrinks from lack of stimulation. Not only does losing teeth affect your smile, it also changes the shape of your face causing you to look prematurely aged. Current dental implant treatments can change your life. From a single missing tooth to an entire set of teeth, dental implants restore your appearance, speech, nutrition, oral health, comfort, and self-esteem. So smile big, eat what you want, and be a confident you! smile big, eat what you want, be a confident you! bone loss ages your face why choose dental implants? Crowns, bridges and dentures address the short-term cosmetic problem of missing teeth but do nothing to stop bone loss. Crown & bridge dentistry requires grinding down healthy teeth leaving them at much greater risk for cavities and tooth failure. Bridges do not stop bone loss. Dentures become uncomfortable and unstable over time as the jawbone shrinks causing eating and speech problems.