A Leap Forward for TMC3 P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pursuit of Excellence Published for the Nursing Staff of Miami Children’S Hospital
PURSUIT OF EXCELLENCE PUBLISHED FOR THE NURSING STAFF OF MIAMI CHILDREN’S HOSPITAL Volume 7 • Issue 1 • Spring 2006 Miracles in Haiti By Carolyn Domina, ARNP, MSN, CNOR, CNABC Operating Room se Lea ur de ince 2003, a N r surgical team S from MCH has made multiple trips to Haiti to help children diagnosed with hydrocephalus. With the help of Project Medis- hare, Helping Hands Clinic and from the In t Pavillon Notre Dame th igh des Pauvres, where the e Spotl surgeries are performed in Haiti, we have been Debbie Salani able to make a differ- surgeries as possible before dark. When night Director of ence in the lives of dozens of families. falls, we generally lose power and water. Emergency Services The neurosurgical team has been per- The children that we treat range in age forming a procedure known as a ventricular from a few months to 12 years of age, with peritoneal shunt, which involves placement some being a bit older. Most of these kids Debbie brings to her of a small flexible plastic tube that diverts role more than 25 years excess cerebral spinal fluid from the brain continued on page 6 experience as a pediatric to another part of the body where the fluid nurse practitioner. can be reabsorbed. We also have performed a procedure known as an endoscopic third In this issue ventriculostomy (ETV) in which a small hole Degrees: is made in the floor of the third ventricle of Implementing a Humpty Dumpty FallsTM • Bachelor’s degree in the brain which allows the cerebrospinal fluid Scale & Prevention Program psychology from to bypass the obstruction and flow toward the A Day in the Life of a Nurse Marywood University in area where it can be excreted by the body. -
Quilt Project Index
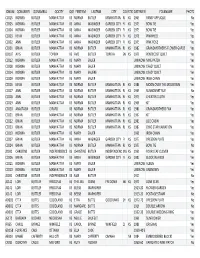
IDNUM QONAMEFI QONAMELA QOCITY QOSTATEFIRSTNM LASTNM CITY COUNTYSTATEDATEMEN FOLKNAME PHOTOS CC015 NORMA BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1965 PANSY APPLIQUE No CC005 NORMA BUTLER MANHATTAN KS ANNA WASINGER GARDEN CITY FI KS 1973 BOW TIE Yes CC004 NORMA BUTLER MANHATTAN KS ANNA WASINGER GARDEN CITY FI KS 1973 BOW TIE Yes CC003 KEVIN BUTLER MANHATTAN KS ANNA WASINGER GARDEN CITY FI KS 1978 PINWHEEL Yes CC002 ANN BUTLER MANHATTAN KS ANNA WASINGER GARDEN CITY FI KS 1975 PINK ROSE Yes CC001 BRIAN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1982 GRANDMOTHER'S FLOWER GARDE Yes DD107 AVIS BUTLER TOPEKA KS AVIS BUTLER TOPEKA SN KS 1979 PENTECOST QUILT Yes CC012 NORMA BUTLER MANHATTAN KS MARY SAUER UNKNOW NINE PATCH Yes CC008 NORMA BUTLER MANHATTAN KS MARY SAUER UNKNOW CRAZY QUILT Yes CC014 NORMA BUTLER MANHATTAN KS MARY SAUERE UNKNOW CRAZY QUILT Yes CC009 NORMA BUTLER MANHATTAN KS MARY SAUER UNKNOW IRISH CHAIN Yes CC016 KEVIN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1986 MOON OVER THE MOUNTAIN Yes CC017 ANN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1969 SUNBONNET SUE No CC018 ANN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1975 CHEATER CLOTH Yes CC019 ANN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1968 KIT Yes CC020 ANASTASIA BUTLER GIRARD KS NORMA BUTLER MANHATTAN RL KS 1980 GRANDMOTHERS FAN Yes CC021 BRIAN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1967 KIT Yes CC022 BRIAN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN RL KS 1983 LOG CABIN Yes CC023 BRIAN BUTLER MANHATTAN KS NORMA BUTLER MANHATTAN -

1:30 Pm TMC Executive Offices Council Members Present
VOLUNTEER SERVICES COUNCIL September 26, 2017 12 – 1:30 p.m. TMC Executive Offices Council Members Present: Courtney Hoyt, Harris Health System Jessica Segal, Harris Health System Estelle Luckenbach, San Jose Clinic Marion Schoeffield, Harris County Long-Term Care Ombudsman Program Millicent Lacy, Texas Children’s Hospital Ian Todd, Harris Health System Sarah King, Ronald McDonald House Houston Helen Villaseñor, Shriner’s Hospital for Children Cheronda Rutherford, Houston Methodist Hospital Kellye Moran, LifeGift Organ Donation Center Jacquelyn Jones, Memorial Hermann Mayra Cantu, Memorial Hermann Irma Almaguer, TIRR Memorial Hermann Frankie Duenes, Gulf Coast Regional Blood Center Guests Present: Esmerelda Soria- Mabin Armand Viscarri TMC Members Present: Carter Fitts, Marketing Associate Tatum Boatwright, Marketing Manager Shelby Wolfenberger, Office Manager MEETING HIGHLIGHTS: I. Welcome & Introductions: Frankie Duenes, Gulf Coast Regional Blood Center • The meeting commenced shortly after noon with everyone going around the table and introducing themselves. We started off on an uplifting note sharing a few stories about our community coming together during Hurricane Harvey. II. Volunteer Workshop Planning: • The council will be hosting their second annual volunteer services workshop on October 24th from 8:30am-2:00pm at Ben Taub Hospital. • This half-day program will provide all attendees with three informational sessions that relate to volunteering. Lunch will be provided and the opportunity to tour the facility will conclude the program. We hope to see you all there! • The planned agenda is as follows: • 8:30 - 9 a.m. Check in and Coffee/Drinks • 9 - 9:45 a.m. - Session 1: Empathetic Communication – Harris Health Team • 10 - 10:45 a.m. -

Casa De Amigos: Where Dreams Become Realities Connie Myer 26 Middle East Mosaic: an Egyptian Pope Harold S
SEPTEMBER 1979 "Mission Means" entries 11111 New Series Vol. XXXX No. 1 • Whole Series Vol. LXVIX No. 8 • September 1979 3 Mission Memo 7 Editorials 8 Mission Means .. 9 Promises to Keep Nancy Veglahn 11 Call and Response Velma Mitchell 13 That of God in Every Man Dorothy A. Stickel! 13 Poem: Senility 15 A Selection of Posters 20 Mission on Friendship Square Natalie Barber 22 Casa de Amigos: Where Dreams Become Realities Connie Myer 26 Middle East Mosaic: An Egyptian Pope Harold S. Vogelaar 29 Bob Nakata Organizes the Home Folks Alex Vergara 33 The Cross Over Kujyo Community Jack Mcintosh 35 A New Kind of Hispanic Church Charley Lerrigo 37 Kamala Edwards Goes Home Ruth Dinkins Rowan 38 Recruiting Blacks for the Ministry Dwight Stewart 39 A Report to Our Readers Beverly J. Chain 41 Special Report: Faith, Science and the Future Arthur J. Moore 43 Books 44 Letters 45 The Moving Finger Writes COVER Detail from "Mission Means Mending Mankind," Poster by Irene Roderick, Austin, Texas Editor, Arthur J. Moore; Managing Editor, Charles E. Brewster Associate Editor, Ellen Clark; Art Director, Roger C. Sadler Administrative Assistant, Florence J. Mitchell 475 Riverside Drive, New York, New York 10027 Published Monthly (bimonthly, July-August) by the Board of Global Ministries of the United Methodist Church, Education and Cultivation Division, in association with the United Presbyterian Church, USA. Second-class Mail Privileges Authorized at New York, N.Y. Additional Entry at Nashville, Tennessee. Copyright 1979 by Board of Global Ministries of the United Methodist Church. No part of New World Outlook may be reproduced in any form without written permission from Editors. -
Bmc Stands with You
TheThe Official Official MagazineMagazine ofof thethe GreaterGreater Houston Builders AssociationAssociation • • www.ghba.orgwww.ghba.org DECEMBER 2018 HOUSTON DECEMBER 2018 Builder BMC STANDS WITH YOU Never Leave Your Jobsite Millwork Express Delivery – 4 Hour Guarantee – Details Inside Photo by JAK Photography New FiberCraft Composite Doors & More! “Looks so good, you’ll think it’s wood.” TM Why GlassCraft Doors? FiberCraft® Composite® BarnCraft ThermaPlus® • FiberCraft Composite Arch Lite Double Doors are premium in features, yet priced as standard orders, not custom. • Multiple glass options for both impact and non-impact units. • No unsightly plugs around the glass frames. • ThermaPlus steel doors are thermally broken and trimmable in the field for easy installation. • Priced 40% less than other premium steel doors. Innovative product lines and designs. See more online. • 18 gauge steel doors that are built strong and secure. • Windstorm rated options available (80 DP Ratings). GlassCraft products are available at your leading millwork distributors and dealers nationwide. Contact us for details: Visit www.glasscraft.com / 713-690-8282 Visit www.glasscraft.com® strucsure_houstonbuilder_1118.pdf 1 11/23/18 8:49 AM New FiberCraft Composite Doors & More! C M Y CM MY CY “Looks so good, you’ll think it’s wood.” CMY TM K As another year comes to a close, I, along with the StrucSure Home Warranty sta, want to thank the Texas builders who trusted us with their warranty and risk management needs Why GlassCraft Doors? during 2018. We wish you prosperity and continued success in the new year! FiberCraft® Composite® BarnCraft ThermaPlus® • FiberCraft Composite Arch Lite Double Doors are premium Contact me to learn more about StrucSure’s in features, yet priced as standard orders, not custom. -
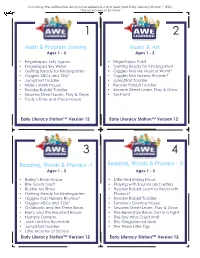
Math & Problem Solving Music & Art Reading, Words
Cut along the dotted line and place reference cards near your Early Literacy Station™ (ELS). *Title not included on ELS Tablet 1 2 Math & Problem Solving Music & Art Ages 1 - 3 Ages 1 - 3 • Fingertapps Jelly Jigsaw • Fingertapps Paint • Fingertapps Sky Writer • Getting Ready for Kindergarten • Getting Ready for Kindergarten • Giggles Kids My Musical World* • Giggles ABCs and 123s* • Giggles Kids Nursery Rhymes* • JumpStart Toddler • JumpStart Toddler • Millie’s Math House • Reader Rabbit Toddler • Reader Rabbit Toddler • Sesame Street Learn, Play & Grow • Sesame Street Learn, Play & Grow • Tux Paint • Trudy’s Time and Place House Early Literacy Station™ Version 12 Early Literacy Station™ Version 12 3 4 Reading, Words & Phonics -1 Reading, Words & Phonics - 2 Ages 1 - 3 Ages 1 - 3 • Bailey’s Book House • Little Red Riding Hood • Billy Goats Gruff • Playing with Sounds and Letters • Buckle My Shoe • Reader Rabbit Learn to Read with • Getting Ready for Kindergarten Phonics* • Giggles Kids Nursery Rhymes* • Reader Rabbit Toddler • Giggles ABCs and 123s* • Sammy’s Science House • Goldilocks and the Three Bears • Sesame Street Learn, Play & Grow • Harry and the Haunted House • The Berenstain Bears Get in a Fight • Humpty Dumpty • The Boy Who Cried Wolf • Jack and the Beanstalk • The Gingerbread Man • JumpStart Toddler • The Three Little Pigs • Little Monster at School Early Literacy Station™ Version 12 Early Literacy Station™ Version 12 Cut along the dotted line and place reference cards near your Early Literacy Station™ (ELS). *Title not included -

BOARD of TRUSTEES Board Meeting AGENDA
BOARD OF TRUSTEES Board Meeting 8:00 A.M. Thursday, June 24, 2021 Please note the Board meeting time change. Agenda item presentation may be taken out of order. – NOTICE – TO: HARRIS COUNTY RESIDENTS AND ALL OTHER INTERESTED PERSONS DATE: JUNE 20, 2021 Notice is hereby given that the Board of Trustees of the Harris Health System (Harris County Hospital District d/b/a Harris Health System) will convene at 8:00 a.m. on Thursday, June 24, 2021. This meeting will be conducted by videoconference. Per temporary meeting suspension rules issued by Governor Greg Abbott due to the COVID-19 pandemic, the meeting may be viewed online: http://harrishealthtx.swagit.com/live. The Board of Trustees will consider the following matters: Mission Harris Health is a community-focused academic healthcare system dedicated to improving the health of those most in need in Harris County through quality care delivery, coordination of care, and education. AGENDA I. Call to Order and Record of Attendance Dr. Arthur Bracey II. Approval of the Minutes of Previous Meeting Dr. Arthur Bracey • Board Meeting – May 27, 2021 III. Announcements / Special Presentations Dr. Arthur Bracey A. CEO Report Including Updates on COVID-19, Vaccinations and Special Announcements [Strategic Pillar 2: People] • Dr. Jackie Brock, Named Chief Nursing Executive, Effective May 17, 2021 B. Board Member Announcements Regarding Board Member Advocacy and Community Engagements IV. Public Comment Dr. Arthur Bracey V. Consent Agenda Items Dr. Arthur Bracey A. Recommended Committee Approvals 1. Consideration of Acceptance of Harris Health’s Quality Manual – Dr. Ann Barnes & Dr. Yashwant Chathampally [Strategic Pillar 1: Quality and Patient Safety] 2. -

Agenda/Itinerary
THE CENTRE FOR NATIONAL SECURITY AND COUNCIL ON EMERGENCY MANAGEMENT Executive Study Tour: Building Resilience Learning from Hurricane Harvey Agenda/Itinerary Tour Objectives: LEARN how the Houston and various stakeholders responded to Hurricane Harvey. UNDERSTAND the progress being made at all levels of government in responding to catastrophic hurricanes. EXPERIENCE how emergency management practitioners, government officials at all levels, communities, volunteers, and critical infrastructure operators responded to this event. DISCUSS the implications of lessons identified during the study tour for Canada. NETWORK and learn with peers – share new approaches, insights and challenges and exchange experiences and ideas with leading world experts. MONDAY, APRIL 22ND HOUSTON Participant Arrival Individuals will be arriving into Houston Accommodation: Le Méridien Houston Downtown 1121 Walker St., Houston, TX (713) 222-7777 (approximate 30-minute drive from the airport You should know: Check in time is after 3 p.m. and check out is at 12:00 p.m. (noon) Room service is available 24 hours with limited service after 11:00 a.m. Fitness Centre is located on the 23rd floor and is available 24 hours – there is no pool Business Centre is located on the second floor (located near the front desk) and is available 24 hours Restaurant: Zutro is located on the main floor – open from 6:00 a.m. – 10:00 p.m. (breakfast, lunch and dinner) Coffee: Starbucks, 914 Dallas St. (6 minute walk from hotel) 6:00 p.m. Casual Networking Dinner For those of you available that want to meet for a casual dinner, let’s meet in the lobby for 6:00 p.m. -

Department of Drama ® Presents
Paris Junior College Department of Drama ® presents Free Virtual Production on Zoom 7:30 p.m., Dec. 3, 4, 5 • 2:30 p.m., Dec. 6 Message from the Department of Drama Paris Junior College’s Department of Drama would like to ex- tend our warmest welcome to all in the 2020-21 theatre sea- son. Our Department has a tradition of exceptional students who have graced our stages, learned in our classrooms, and worked in our studios. As a student of theatre at PJC they are joining an accom- plished faculty of artists and scholars who are committed to creating, researching, and teaching exciting theatre and dra- ma. Our students develop skills both on and offstage while preparing to join the growing network of PJC Alumni in the professional and educational world of theatre arts. Whether students are a major, or just a curious student taking classes, we encourage them to become involved in the many activities of our department; this is an essential way to chal- lenge themselves and discover new insights as a part of their undergraduate education and experience. Students looking to venture into both music and drama have the option of a concentration in Musical Theatre here at Paris Junior College. On behalf of the students and faculty of the PJC Department of Drama we welcome you to our home. The Drama Faculty Alice in Cyberspace SCENES Scene 1: Alice’s Gaming Party Scene 2: The Kingdoms of the Red and White Queens Scene 3: Humpty Dumpty’s Wall Scene 4: The Lake of Tears with the Mock Turtle and Gryphon Scene 5: The Mad Tea Party Scene 5.5 / Scene -

Using Date Specific Searches on Google Books to Disconfirm Prior
social sciences $€ £ ¥ Article Using Date Specific Searches on Google Books to Disconfirm Prior Origination Knowledge Claims for Particular Terms, Words, and Names Mike Sutton and Mark D. Griffiths * ID Department of Social Sciences, Nottingham Trent University, 50 Shakespeare Street, Nottingham NG1 4FQ, UK; [email protected] * Correspondence: mark.griffi[email protected] Received: 2 March 2018; Accepted: 12 April 2018; Published: 16 April 2018 Abstract: Back in 2004, Google Inc. (Menlo Park, CA, USA) began digitizing full texts of magazines, journals, and books dating back centuries. At present, over 25 million books have been scanned and anyone can use the service (currently called Google Books) to search for materials free of charge (including academics of any discipline). All the books have been scanned, converted to text using optical character recognition and stored in its digital database. The present paper describes a very precise six-stage Boolean date-specific research method on Google, referred to as Internet Date Detection (IDD) for short. IDD can be used to examine countless alleged facts and myths in a systematic and verifiable way. Six examples of the IDD method in action are provided (the terms, words, and names ‘self-fulfilling prophecy’, ‘Humpty Dumpty’, ‘living fossil’, ‘moral panic’, ‘boredom’, and ‘selfish gene’) and each of these examples is shown to disconfirm widely accepted expert knowledge belief claims about their history of coinage, conception, and published origin. The paper also notes that Google’s autonomous deep learning AI program RankBrain has possibly caused the IDD method to no longer work so well, addresses how it might be recovered, and how such problems might be avoided in the future. -

Texasaim Current Hospitals As of February 14, 2019
TexasAIM Current Hospitals as of February 14, 2019 The following hospitals are enrolled in TexasAIM as of February 14, 2019.* - Abilene Regional Medical Center - CHI St. Luke's Health Memorial Medical Center- - Baptist Hospitals of Southeast Texas-Beaumont Livingston Campus - CHI St. Luke's Health Memorial Medical Center- - Baptist Medical Center Lufkin - Baylor Scott & White All Saints Medical Center- - CHI St. Luke's Health–Sugar Land Hospital Fort Worth - CHI St. Luke's Health–The Vintage Hospital - Baylor Scott & White Medical Center-Brenham - CHI St. Luke's Health–The Woodlands Hospital - Baylor Scott & White Medical Center- - Children's Memorial Hermann Hospital Centennial - Childress Regional Medical Center - Baylor Scott & White Medical Center–College - CHRISTUS Good Shepherd Medical Center- Station Longview - Baylor Scott & White Medical Center–Frisco - CHRISTUS Mother Frances Hospital-Sulphur - Baylor Scott & White Medical Center– Springs Grapevine - CHRISTUS Santa Rosa Hospital-New Braunfels - Baylor Scott & White Medical Center–Hillcrest - CHRISTUS Santa Rosa Hospital-Westover Hills - Baylor Scott & White Medical Center–Irving - CHRISTUS Santa Rosa-The Children's Hospital of - Baylor Scott & White Medical Center–Lake San Antonio Pointe - CHRISTUS Southeast Texas-St. Elizabeth - Baylor Scott & White Medical Center–Lakeway - CHRISTUS Spohn Hospital Corpus Christi-South - Baylor Scott & White Medical Center–Marble - CHRISTUS Spohn Hospital-Beeville Falls - CHRISTUS Spohn Hospital-Kleberg - Baylor Scott & White Medical Center– -

Let Their Story Inspire You
LET THEIR STORY INSPIRE YOU THE 37TH ANNUAL TEXAS BUSINESS HALL OF FAME LEGENDS INDUCTION DINNER OCTOBER 16, 2019 LET THEIR STORY INSPIRE YOU With special thanks to our presenting sponsor since 2017 RICHARD W. FISHER THE 37TH ANNUAL TEXAS BUSINESS FORMER PRESIDENT AND CEO HALL OF FAME Federal Reserve Bank of Dallas Dallas GEORGE C. “TIM” HIXON (Posthumously) DIRECTOR EMERITUS LEGENDS Hixon Properties Incorporated San Antonio BILL MILLER FAMILY INDUCTION Bill Miller Bar-B-Q 2019 San Antonio PRESENTING SPONSOR KENDRA SCOTT DINNER LEGENDS CEO AND FOUNDER Kendra Scott Austin WEDNESDAY, OCTOBER 16, 2019 ROBERT F. SMITH FOUNDER HENRY B. GONZÁLEZ CONVENTION CENTER • SAN ANTONIO, TEXAS Vista Equity Partners Reception 6:00 PM • Induction Dinner 7:00 PM Austin GRAHAM WESTON MASTER OF CEREMONIES CEO Dr. Henry G. Cisneros Weston Ventures San Antonio Black Tie • Reservations will be held at the door TEXAS BUSINESS LEGENDS 2002 1997 1988 1984 2012 2007 1993 Robert J. Allison, Jr. J.S. Abercrombie John S. Justin, Jr. Monroe Anderson Donald Adam Tom Benson Aron S. Gordon Louis A. Beecherl, Jr. Lamar Hunt Herbert D. Kelleher William Clayton Frank A. Bennack, Jr. Dr. James R. Leininger The Kruse Family HALL OF FAME William E. “Bill” Greehey Robert C. McNair, Sr. Robert M. Luby George Kozmetsky J.M. Haggar, Sr. Douglas L. Foshee Paul J. Sarvadi Lee William “Bill” McNutt, Jr. Fayez Sarofim Frank W. Mayborn Oveta Culp Hobby John L. Nau, III Clayton W. Williams, Jr. Robert R. Onstead Robert D. Rogers Edward E. Whitacre, Jr. Henry S. Miller, Jr. Stanley Marcus Todd Wagner Ambassador Robert S.