Style Settings for Minute
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

B23964 SWSI Cover + 15Mm Spine
Growth and Development Growth and Development ST SOCIAL WORK SERVICES FOR THE 21 SOCIAL WORK SERVICES FOR THE 21 CENTURY The Report of the Chief Inspector of Social Work Services for Scotland 2002 ST CENTURY Further copies are available from the Stationery Office Bookshop 71 Lothian Road · Edinburgh EH3 9AZ I SBN 0-7559- 0394- 3 Tel 0870 606 55 66 Astron B23964 11/02 The text pages of this document are produced from 100% Elemental Chlorine Free, environmentally preferred material and is 100% recyclable. 9 780755 903948 www.scotland.gov.uk Making it work together Growth and Development SOCIAL WORK SERVICES FOR THE 21ST CENTURY The Report of the Chief Inspector of Social Work Services for Scotland Laid before the Scottish Parliament by the Scottish Ministers, November 2002. SE/2002/304 1 2 Introduction The Local Reports Growth and Development – Social Work Services for the 21st Century, is the second annual report prepared by the Chief Social Work Inspector. Completed in 2002, it includes a national overview of social work services and short reviews of services in each of the 32 councils. This report contains the reviews of social work services in each of the 32 local authorities with the national overview contained in a separate document. The individual reports are based on an analysis of demographic information, statistical returns to the Scottish Executive and Accounts Commission (Audit Scotland), information provided on visits to the local authorities and other written information provided by them. The introductory section of each report covers the demographic and social features of the area. -

Older People with Functional Mental Illness in Scotland 2019
Good practice guide Advice notes Investigations Service users and carers information Older people'speople’sfunctional functionalmental mentalhealth in healthhospitals: wards in hospitals: themed visitvisitreport report Monitoring and visiting reports Annual statistical monitoring Corporate reports Visiting and monitoring reports 16 April 2020 2020 APS Group. MWCS Brand update. Publication covers 2 Report on a series of visits carried out by the Mental Welfare Commission for Scotland to people admitted to wards for older people with functional mental illness in Scotland 2019. Contents Executive summary ........................................................................................................................ 5 Summary of recommendations ................................................................................................. 5 Introduction ..................................................................................................................................... 7 Functional mental illness in older people .................................................................................. 7 Why we carried out these visits ................................................................................................. 7 How we carried out these visits ..................................................................................................... 9 Where we visited ......................................................................................................................... 9 Patient characteristics -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

NHS Tayside CONSULTANT PSYCHIATRIST
NHS Tayside CONSULTANT PSYCHIATRIST General Adult Psychiatry (sub-specialty: substance misuse psychiatry) VACANCY Consultant in General Adult Psychiatry (sub-specialty: substance misuse psychiatry) Dundee Integrated Substance Misuse Service 40 hours per week £80,653 (GBP) to £107,170 (GBP) per annum Tenure: Permanent We are seeking to recruit an enthusiastic and motivated Consultant Psychiatrist in Addictions to fill a post which has arisen following retirement of the existing post holder. The post is one of four consultant posts within NHS Tayside substance misuse services. This position is based within the Dundee Integrated Substance Misuse Service and you will have responsibility for one of two emerging Dundee locality teams. There will be significant opportunities to lead service development activity both within Dundee and in the wider Tayside area, as well as provide clinical leadership around governance and quality improvement. With strong links to the University of Dundee Medical School and the University`s Division of Neuroscience research facilities, there are opportunities for both under and post graduate teaching as well involvement in addiction related research activity. You will be joining a well-established clinical service consisting of experienced substance misuse nurses, an expanding Non-Medical Prescribing nurse workforce, dedicated pharmacist input, substance misuse psychology, a Specialty Doctor, and General Practitioners with Special Interests. Higher Specialty Trainees are regularly placed with the service. There is access to a Substance Misuse Inpatient facility for patients requiring Tier 4 interventions. You will be working alongside Social Work colleagues and this partnership working will be enhanced with the further development of integrated teams within the Dundee Health and Social Care Partnership. -
Scottish ECT Accreditation Network Annual Report 2015
National Services Scotland Scottish ECT Accreditation Network Annual Report 2015 A summary of ECT in Scotland for 2014 Scottish ECT Accreditation Network Annual Report 2015; A summary of ECT in Scotland for 2014 © NHS National Services Scotland/Crown Copyright 2015 First published October 2009 Brief extracts from this publication may be reproduced provided the source is fully acknowledged. Proposals for reproduction of large extracts should be addressed to: PHI Graphics Team NHS National Services Scotland Gyle Square 1 South Gyle Crescent Edinburgh EH12 9EB Tel: +44 (0)131 275 6233 Email: [email protected] Designed and typeset by: Chris Dunn, PHI Graphics Team Translation Service If you would like this leaflet in a different language, large print or Braille (English only), or would like information on how it can be translated into your community language, please phone 0845 310 9900 quoting reference 287407. Scottish ECT Accreditation Network Annual Report 2015; A summary of ECT in Scotland for 2014 Summary Hospital Activity Table 20141 Hospital Patients Episodes Treatments All Stimulations Median Median for episodes Treatments Treatments Stimulations commencing Delivered per Episode per Episode in 20148 in 20149 Ailsa & Crosshouse 23 30 271 285 289 9 11 Argyll & Bute * * 41 45 50 5 6 Carseview 13 16 138 157 150 9 10 Forth Valley Royal 14 15 160 181 198 11 14 Hairmyres2 15 18 151 160 182 9 12 Huntlyburn House 15 16 127 119 157 8 9 Inverclyde 14 14 140 242 149 10 11 Leverndale3 27 29 312 339 354 12 12 Midpark Hospital 18 27 190 219 198 6 7 Murray Royal 18 26 233 226 252 10 10 New Craigs * * 51 51 57 12 13 Queen Margaret4 20 24 255 315 289 12 12 Royal Cornhill 58 69 519 602 637 7 8 Royal Edinburgh5 38 47 510 632 664 10 12 St John's 24 31 239 245 272 8 9 Stobhill6 37 43 329 349 381 7 8 Susan Carnegie * * 69 68 83 8 12 Wishaw7 * * 59 67 81 5 10 Total 357 434 3,794 4,302 4,443 8 10 Notes: * Indicates values that have been suppressed because of the risk of disclosure. -

Moredun Ward, Murray Royal Hospital, Muirhall Road, Perth PH2 7BH Date of Visit: 22 February 2018
Mental Welfare Commission for Scotland Report on announced visit to: Moredun Ward, Murray Royal Hospital, Muirhall Road, Perth PH2 7BH Date of visit: 22 February 2018 Where we visited Moredun Ward is a mixed sex adult acute admission ward with 24 beds. We last visited this service on a local visit on 22 October 2015, and made recommendations about care planning and patient involvement in multidisciplinary reviews. We also visited Moredun Ward on 3 August 2016, as part of a themed visit to adult acute wards across Scotland. On the day of this visit we wanted to look generally at the care and support provided in the ward, because it was over two years since our previous local visit Who we met with We met with and/or reviewed the care and treatment of seven patients and met with one relative. We also met one patient who had recently been discharged from the ward, but wanted to meet us and tell us about their care and treatment while they were in the ward. We spoke with the acting charge nurse, with the psychiatrist who is currently working in the ward, with other members of the nursing team, and with the pharmacist, who was in the ward during our visit. Commission visitors Ian Cairns, Social Work Officer and visit coordinator Alison Thomson, Executive Director (Nursing) Claire Lamza, Nursing Officer What people told us and what we found Care, treatment, support and participation Most patients we met spoke positively about their care and treatment in the ward, and about the support they received from staff. -
Contract Between the Scottish Ministers and Reliance Secure
Contract between The Scottish Ministers and Reliance Secure Task Management Ltd for the Provision of Prisoner Escort & Court Custody Services in Scotland Contract No. 00339 3 November 2003 Confidentiality No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of the Authority and will be returned upon request. Scottish Prison Service Form Of Contract Contract No. 00339 Contract Between The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service whose Headquarters are Calton House 5 Redheughs Rigg EDINBURGH EH12 9HW (hereinafter called “the Authority”), of the first part and Reliance Secure Task Management Ltd (Company number 2057887) whose Registered Office is Boundary House Cricketfield Road Uxbridge Middlesex UB8 1QL (hereinafter called “Service Provider”), of the second part The Authority hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Authority, the Services (as hereinafter defined) on the terms and conditions set out in this Contract. The Authority agrees to pay to the Service Provider the Charges due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Authority for the due performance of the Contract and the Authority will be entitled to enforce this Contract on behalf of the Scottish Ministers. The Contract shall consist of this Form of Contract (comprising this and the following page) and the six Schedules annexed hereto which shall be deemed to form, and to be read, and to be construed, as part of the Contract, declaring that references in the Contract to a Schedule shall, unless the context otherwise requires, be held to be references to the relevant Schedule forming part of this Contract. -

Deliverable D6 FAMS Trials Report: Testing and Evaluation
EUROPEAN COMMISSION INFORMATION SOCIETIES TECHNOLOGY (IST) PROGRAMME FAMS IST-2001-34347 FLEXIBLE AGENCY FOR COLLECTIVE, DEMAND RESPONSIVE MOBILITY SERVICES Deliverable D6 FAMS Trials Report: Testing and Evaluation Document Type: Deliverable Deliverable Number: D6 Deliverable Title: FAMS Trials Report: Testing and Evaluation Work Package WP5 Comparative Evaluation & Business Case Assessment Editor Pekka Eloranta, Mobisoft Dissemination Level Public Version 1.2 Circulation FAMS Consortium Commission Services Contractual date 29th July 2003 of Delivery Planned date 12thth November 2003 of Delivery Keywords Validation, Trial, Testing, Evaluation, Take-up Action, Telematics, Demand Responsive Transport Services, Multimodal, Public Transport DOCUMENT HISTORY Version Date Initials Revised Short description sections 0.1 31/07/03 PE, BM, All Structure of the Deliverable and the first draft AF, MB, established. NdV, CB 0.2 21/10/03 PE, BM, All Site inputs added, revised and shortened AF, MB, NdV, CB 1.0 29/10/03 PE All Deliverable shortened 1.1 03/11/03 JFM All UNEW comments 1.2 12/11/03 BM, JFM, 1, 4.1, 7.1 Minor revisions PE 2 Version number 1.2 Date 12th November 2003 Editors Pekka Eloranta Contributors to this report Giorgio Ambrosino, ATAF Claudia Binazzi, ATAF Marco Boero, Softeco Sismat Neri di Volo, ATAF Andrea Ferrari, SITA Jarno Kanninen, Mobisoft Brian Masson, Angus Transport Forum Brendan Finn, ETTS Jenny Mageean, UNEW 3 TABLE OF CONTENTS EXECUTIVE SUMMARY..................................................................................................6 -

Mark Richards
70 stories for #NHS70: Celebrating Mental Health Nursing’s Contribution in Scotland - #70mhnursingstories Name: Mark Richards Current Job: Director of Nursing and AHPs/Deputy CEO NHS Board Area/Trust: The State Hospitals Board for Scotland Your Story What was your journey in to mental health nursing? (700 words max) Growing up in Perth, I had no family history or connection to nursing, in fact, I was brought up in and around the family bike shop and had always thought that my working life would have had some connection to the bike trade. I also had a neighbour (Ian), who was a good friend of the family, and who was a Mental Health Nurse. I can remember as a wee boy during the school summer holidays being told to keep the noise down because Ian was sleeping and wondering what on earth he did staying up all night! And how could a man be a nurse? Perhaps some natural curiosity at an early age. Looking back at leaving school, I really had no idea on career choice as a 16 year old. I thought I would follow in my Dad’s footsteps (who was a tool maker to trade) and pursue a career that was focused on the mechanical side of things. I applied for an apprenticeship with the Royal Navy as an aeronautical engineer, focused on helicopter engines. Having been through the recruitment selection process, I was asked to apply back again the following year, which necessitated a complete rethink of what career options were in front of me. Cue a chance conversation with Ian, who spoke to me about a career in Mental Health Nursing. -
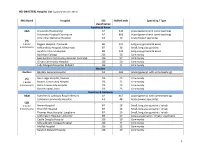
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Mental Welfare Commission for Scotland Report on Announced Visit To: Moredun Ward, Murray Royal Hospital, Muirhall Road, Perth P
Mental Welfare Commission for Scotland Report on announced visit to: Moredun Ward, Murray Royal Hospital, Muirhall Road, Perth PH2 7BH Date of visit: 27 November 2019 V5 – 08.19 Where we visited Moredun Ward is a 22-bedded mixed-sex adult acute admission ward. All rooms in the ward are single and en-suite, with male and female patients in rooms at different sides of the ward. There are enclosed gardens around the ward. We last visited this service on 13 February 2019, when we made a recommendation about care planning. We received a clear action plan in relation to this recommendation, which described the improvement actions the service was taking to develop the approach to care planning in the ward. On the day of this visit we wanted to meet with patients, look generally at how care and treatment is being provided, and to follow up on the previous recommendation. Who we met with We met with and/or reviewed the care and treatment of 11 patients, and spoke to one relative. We spoke with the senior charge nurse, the nurse manager, and with the consultant psychiatrist responsible for care and treatment in the ward. We also met and spoke with a number of members of the nursing team during the day. Commission visitors Ian Cairns, Social Work Officer Alison Thomson, Executive Director (Nursing) Philip Grieve, Nursing Officer Dr Juliet Brock, Medical Officer 1 What people told us and what we found Care, treatment, support and participation Most patients we met spoke positively about their care and treatment in Moredun Ward and about their interaction with staff. -
Scottish ECT Accreditation Network Annual Report 2012
National Services Scotland Scottish ECT Accreditation Network Annual Report 2012 A summary of ECT in Scotland for 2011 SD SC TLAND Scottish ECT Accreditation Network Annual Report 2012; A summary of ECT in Scotland for 2011 © NHS National Services Scotland/Crown Copyright 2012 First published October 2009 Brief extracts from this publication may be reproduced provided the source is fully acknowledged. Proposals for reproduction of large extracts should be addressed to: ISD Scotland Publications Information Services Division NHS National Services Scotland Gyle Square 1 South Gyle Crescent Edinburgh EH12 9EB Tel: +44 (0)131-275-6233 Email: [email protected] Designed and typeset by: ISD Scotland Publications Translation Service If you would like this leaflet in a different language, large print or Braille (English only), or would like information on how it can be translated into your community language, please phone 0131 275 6665. Scottish ECT Accreditation Network Annual Report 2012; A summary of ECT in Scotland for 2011 Summary Hospital Activity Table 20111 Median Median Treatments Stimulations Hospital Patients Episodes Treatments Stimulations per Episode per Episode Ailsa & Crosshouse 35 48 445 478 10.5 11.0 Argyll & Bute * * 27 29 6.0 7.0 Carseview 17 20 195 216 10.0 10.5 Dunnikier * * 68 82 9.0 10.0 Forth Valley Royal2 * * 39 45 4.0 5.0 Hairmyres3 13 15 111 136 8.0 9.0 Huntlyburn, Borders General * 12 144 164 10.5 12.0 Inverclyde 13 13 118 126 8.0 9.0 Leverndale4 25 32 257 289 8.5 10.0 Midpark Hospital5 17 20 151 193 7.0 8.5 Murray Royal 13 14 107 122 7.5 8.5 New Craigs * * 79 90 12.0 12.0 Queen Margaret6 14 17 189 215 10.0 10.0 Royal Cornhill 63 77 556 798 6.0 9.0 Royal Edinburgh7 50 64 773 938 8.0 11.5 St John’s 20 24 197 228 8.0 8.5 Stobhill8 36 41 298 349 7.0 8.0 Susan Carnegie9 * * 62 75 7.0 9.5 Wishaw10 17 19 151 182 7.0 10.0 Total 370 451 3,967 4,755 8.0 9.5 Notes: * Indicates values that have been suppressed because of the potential risk of disclosure.