Wesley E. Shankland,Ii, Dds, Ms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neck Dissection Using the Fascial Planes Technique
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY NECK DISSECTION USING THE FASCIAL PLANE TECHNIQUE Patrick J Bradley & Javier Gavilán The importance of identifying the presence larised in the English world in the mid-20th of metastatic neck disease with head and century by Etore Bocca, an Italian otola- neck cancer is recognised as a prominent ryngologist, and his colleagues 5. factor determining patients’ prognosis. The current available techniques to identify Fascial compartments allow the removal disease in the neck all have limitations in of cervical lymphatic tissue by separating terms of accuracy; thus, elective neck dis- and removing the fascial walls of these section is the usual choice for management “containers” along with their contents of the clinically N0 neck (cN0) when the from the underlying vascular, glandular, risk of harbouring occult regional metasta- neural, and muscular structures. sis is significant (≥20%) 1. Methods availa- ble to identify the N+ (cN+) neck include Anatomical basis imaging (CT, MRI, PET), ultrasound- guided fine needle aspiration cytology The basic understanding of fascial planes (USGFNAC), and sentinel node biopsy, in the neck is that there are two distinct and are used depending on resource fascial layers, the superficial cervical fas- availability, for the patient as well as the cia, and the deep cervical fascia (Figures local health service. In many countries, 1A-C). certainly in Africa and Asia, these facilities are not available or affordable. In such Superficial cervical fascia circumstances patients with head and neck cancer whose primary disease is being The superficial cervical fascia is a connec- treated surgically should also have the tive tissue layer lying just below the der- neck treated surgically. -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

Appendix B: Muscles of the Speech Production Mechanism
Appendix B: Muscles of the Speech Production Mechanism I. MUSCLES OF RESPIRATION A. MUSCLES OF INHALATION (muscles that enlarge the thoracic cavity) 1. Diaphragm Attachments: The diaphragm originates in a number of places: the lower tip of the sternum; the first 3 or 4 lumbar vertebrae and the lower borders and inner surfaces of the cartilages of ribs 7 - 12. All fibers insert into a central tendon (aponeurosis of the diaphragm). Function: Contraction of the diaphragm draws the central tendon down and forward, which enlarges the thoracic cavity vertically. It can also elevate to some extent the lower ribs. The diaphragm separates the thoracic and the abdominal cavities. 2. External Intercostals Attachments: The external intercostals run from the lip on the lower border of each rib inferiorly and medially to the upper border of the rib immediately below. Function: These muscles may have several functions. They serve to strengthen the thoracic wall so that it doesn't bulge between the ribs. They provide a checking action to counteract relaxation pressure. Because of the direction of attachment of their fibers, the external intercostals can raise the thoracic cage for inhalation. 3. Pectoralis Major Attachments: This muscle attaches on the anterior surface of the medial half of the clavicle, the sternum and costal cartilages 1-6 or 7. All fibers come together and insert at the greater tubercle of the humerus. Function: Pectoralis major is primarily an abductor of the arm. It can, however, serve as a supplemental (or compensatory) muscle of inhalation, raising the rib cage and sternum. (In other words, breathing by raising and lowering the arms!) It is mentioned here chiefly because it is encountered in the dissection. -

Chiropractic Treatment Options for TMJ Disorders
Chiropractic Treatment Options for TMJ Disorders Wendy Varish, DC, FACO, CCSP, CCOHC, MCS-P Wendy Varish, DC, FACO, CCSP, CCOHC, MCS-P Howards Grove Chiropractic 516 S. Wisconsin Drive Howards Grove, WI 53083 (920) 565-3922 fax (920) 565-2142 [email protected] Syllabus- Chiropractic Treatment Options for TMJ Disorders The National Institute of Dental and Craniofacial Research reports that as many as 10 million people have TMJ disorders, often presenting with other conditions such as headaches, neck pain, chronic fatigue syndrome, fibromyalgia, IBS, and other systemic illnesses. This 4 hour program will provide the doctor with practical information and techniques specific to TMJ Disorders that can be integrated into even a busy practice the following day. Advanced therapeutic applications and adjusting techniques will be highlighted • TMJ is a synovial joint • Comprised of a biconcave disk compressed between the mandibular condyle and the mandibular fossa of the temporal bone TMJ Articular Disc • Biconcave -- allows for gliding to occur • Fibrocartilage & viscoelastic • Avascular and non-innervated • Ligaments: Anterior, Posterior & Intermediate Bands • Lateral Pterygoid is attached anteriorly • Bilaminar Zone – posterior • Retrodiscal tissue Nerve Supply • Mandibular nerve (CN V), the facial nerve (CN VII), C 1, C 2 and C 3 • Sensory innervation of the temporomandibular joint is derived from the auriculotemporal and masseteric branches of the mandibular branch of the trigeminal nerve (CN V). • Auriculotemporal nerve leaves the mandibular nerve behind the joint and ascends laterally & superiorly to wrap around the posterior region of the joint. Proprioception of the TMJ • Ruffini Endings • function as static mechanoreceptor –act to position the mandible • Pacinian Corpuscles • dynamic mechanoreceptors which accelerate movement during reflexes. -

Elongated Styloid Process
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 13, Issue 5 Ver. IV. (May. 2014), PP 31-33 www.iosrjournals.org Eagle’s Syndrome- Elongated Styloid Process 1Dr. Surekha Teki, 2Dr. D. Asha latha, 3Dr. Srihari babu, 4Dr. K. Lakshmi kumari, 5Dr. G. Siva Prasad, 6Dr. A. Vasanthi. Department Of Anatomy, Andhra Medical College, Visakhapatnam. Abstract: Eagle’s syndrome is a condition in which an elongated styloid process or calcified stylohyoid ligament causes occasional pain in theneck, a feeling of a foreign body (in the pharynx) or some other form of retromandibular-cervical pain. In adults the styloid process is approximately 25 mm long with a tip which is located between the external and internal carotid arteries, lateral to the pharyngeal wall and the tonsillar fossa. Ossification of the stylohyoid and stylomandibular ligament causes prolongation of the styloid process and clinical symptoms. Radiographic finding may show several possible variations: elongated, pseudoarticulated and segmented styloid process, and according to the calcification: peripheral, partial, complete or nodular type calcification. Treatment is primarily surgical.The physician's knowledge of possible clinical variations and diverse symptomatology is important. Key words: Elongated styloid process, Eagle’s syndrome, tonsillar fossa, stylo- hyoid ligament, stylo- mandibular ligament. I. Introduction The styloid process is a bony projection, situated immediately anterior to the stylomastoid foramen, averaging from 20 to 25 mm in length. It is of cylindrical form and projects downwards from the inferior surface of the temporal bone towards the front, downwards and medially narrowing towards the tip. -

AR 31-14 Wong STYLOID AB
1 Temporal headaches and associated symptoms relating to the styloid process and its attachments Annals Academy of Medicine, Singapore January 1995; Vol. 24; No. 1; pp. 124-128 E. Wong, DDS; G Lee, MD; DT Mason, MD KEY POINTS FROM THIS ARTICLE: 1) The styloid process is a thin “spike-like bony process” that is attached to the base of the skull. 2) 5 structures (3 muscles and 2 ligaments) are attached to the styloid process: A)) The styloglossus muscle B)) The stylohyoid muscle C)) The stylopharyngeal muscle D)) The stylomandibular ligament E)) The stylohyoid ligament 3) Trauma (auto accidents, falls, sports injuries, prolonged or excessive mouth opening) can detach any of these 5 structures from the periosteum of the styloid bone. 4) “The detachment of Sharpey's fibers results in the release of noxious chemicals such as kinins, histamines, prostaglandins, etc., which can produce a withdrawal reflex, causing muscle tension, ischaemia, spasm and pain.” 5) Pain transmission from “C” pain fibers induces a host of autonomic responses. [Key Point] 6) These authors have identified 11 common pains and symptoms associated with soft tissue lesions of the styloid process and stylomandibular ligament: A)) Headaches localized in the anterior temporal fossa. This is due to the pain withdrawal reflex and spasm of temporalis muscle fibers. B)) Sore throat and difficulty swallowing in the absence of inflammation. This is due to the pain withdrawal reflex and spasm of all three of the styloid-attached muscles. C)) Pain radiating to the temporomandibular joint and ear. This is due to the pain withdrawal reflex and spasm of the muscles of mastication, particularly the masseter and the medial/lateral pterygoids. -
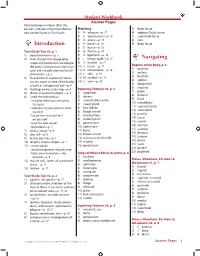
Student Workbook Answer Pages Italicized Page Numbers After the Answers Indicate Where the Informa- Matching 5) Deep Fascia Tion Can Be Found in Trail Guide
Student Workbook Answer Pages Italicized page numbers after the answers indicate where the informa- Matching 5) deep fascia tion can be found in Trail Guide. 1) N adipose—p. 17 6) adipose (fatty) tissue 2) F aponeurosis—p. 13 7) superficial fascia 3) D artery—p. 16 8) skin 4) H bone—p. 10 9) deep fascia Introduction 5) E bursa—p. 16 Tour Guide Tips #1, p. 1 6) B fascia—p. 14 1) bony landmarks—p. 2 7) G ligament—p. 13 2) Even though the topography, 8) I lymph node—p. 17 Navigating shape and proportion are unique, 9) A muscle—p. 11 Regions of the Body, p. 6 the body’s composition and struc- 10) J nerve—p. 17 1) pectoral tures are virtually identical on all 11) K retinaculum—p. 15 2) axillary individuals.—p. 2 12) L skin—p. 10 3) brachial 3) To examine or explore by touch- 13) M tendon—p. 13 4) cubital ing (an organ or area of the body), 14) C vein—p. 16 5) abdominal usually as a diagnostic aid—p. 4 6) inguinal 4) locating, aware, assessing—p. 4 Exploring Textures #1, p. 3 7) pubic 5) directs movement, depth.—p. 4 1) epidermis 8) femoral 6) • read the information 2) dermis 9) facial • visualize what you are trying 3) arrector pili muscle 10) mandibular to access 4) sweat gland 11) supraclavicular • verbalize to your partner what 5) hair follicle 12) antecubital you feel 6) blood vessels 13) patellar • locate the structure first 7) muscle fibers 14) crural on yourself 8) endomysium 15) cranial • read the text aloud 9) perimysium 16) cervical • be patient—p. -

Synovial Joints • Typically Found at the Ends of Long Bones • Examples of Diarthroses • Shoulder Joint • Elbow Joint • Hip Joint • Knee Joint
Chapter 8 The Skeletal System Articulations Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc. Introduction • Bones are designed for support and mobility • Movements are restricted to joints • Joints (articulations) exist wherever two or more bones meet • Bones may be in direct contact or separated by: • Fibrous tissue, cartilage, or fluid © 2015 Pearson Education, Inc. Introduction • Joints are classified based on: • Function • Range of motion • Structure • Makeup of the joint © 2015 Pearson Education, Inc. Classification of Joints • Joints can be classified based on their range of motion (function) • Synarthrosis • Immovable • Amphiarthrosis • Slightly movable • Diarthrosis • Freely movable © 2015 Pearson Education, Inc. Classification of Joints • Synarthrosis (Immovable Joint) • Sutures (joints found only in the skull) • Bones are interlocked together • Gomphosis (joint between teeth and jaw bones) • Periodontal ligaments of the teeth • Synchondrosis (joint within epiphysis of bone) • Binds the diaphysis to the epiphysis • Synostosis (joint between two fused bones) • Fusion of the three coxal bones © 2015 Pearson Education, Inc. Figure 6.3c The Adult Skull Major Sutures of the Skull Frontal bone Coronal suture Parietal bone Superior temporal line Inferior temporal line Squamous suture Supra-orbital foramen Frontonasal suture Sphenoid Nasal bone Temporal Lambdoid suture bone Lacrimal groove of lacrimal bone Ethmoid Infra-orbital foramen Occipital bone Maxilla External acoustic Zygomatic -

Anatomical, Clinical and Radiographic Characteristics of Styloid Syndrome (Eagle Syndrome): a Case Report
Int. J. Morphol., 30(2):701-704, 2012. Anatomical, Clinical and Radiographic Characteristics of Styloid Syndrome (Eagle Syndrome): a Case Report Características Anatómicas, Clínicas y Radiográficas del Síndrome Estiloide (Síndrome de Eagle): un Caso Clínico *Rogério Leone Buchaim; **Daniela Vieira Buchaim; *André Luis Shinohara; *Antonio de Castro Rodrigues; *Jesus Carlos Andreo & * Farooque Jamaluddin Ahmed BUCHAIM, R. L.; BUCHAIM, D. V.; SHINOHARA, A. L.; RODRÍGUES, A. C.; ANDREO, J. C. & AHMED, F. J. Anatomical, clinical and radiographic characteristics of styloid syndrome (Eagle syndrome): a case report. Int. J. Morphol., 30(2):701-704, 2012. SUMMARY: Styloid syndrome is characterized by an elongated styloid process or calcification of the stylomandibular and stylohyoid ligament. This study describes a case of a 65-year-old woman who presented to the Stomatology Clinic, University of Marilia with temporomandibular joint pain, ear ringing and a reduced ability to open the mouth. Panoramic and posteroanterior digital radiographs showed bilateral elongation of the styloid processes, especially of the right side, whose length extended beyond the mandible angle. The diagnosis was confirmed with the association of clinical data and image examinations. The treatment options for styloid Syndrome include clinical follow-up, surgical removal of the styloid process or fracture of the elongated process. The case was managed by providing prosthetic rehabilitation and clinical follow-up, observing the level of discomfort and the benefit that could be achieved by the therapy, and avoiding surgical intervention. KEY WORDS: Eagle syndrome; Elongated styloid process syndrome; Temporal bone. INTRODUCTION The styloid process, located anterior to the stylomastoid approximately 25mm, as described by Eagle (1937), hence foramen, originates in the second brachial arch, namely from any length exceeding that size would be considered elongated. -

General Arthrology (Joints)
General arthrology (Joints) 2 types of joints : 1. Synarthrosis 2. Diarthrosis 1. Synarthrosis (connective tissue, cartilage, bone) -connection by some kind of connective tissue : fibrous tissue, cartilage or bone A. fibrous joint (articulatio fibrosa, syndesmosis) - (sutures, ligaments, Gomphosis) a) 3 types of sutures sutura serrata - sutura squamosa – squamous suture sutura plana – flat suture b) membrana interossea antebrachii, various ligaments c) gomphosis (socket) – dentoalveolar syndesmosis B. cartilaginous joint (articulatio cartilaginea, synchondrosis) – bones are linked by cartilage, nearly immobile continuous connection of bones C. synostosis (by bone tissue, origin of the bones was isolated) 2. Diarthrosis (articulatio synovialis) - Synovial joint Movable connection of 2 or more bones by touch or contact Art. surfaces covered by articular cartilage General features of a joint. Facies articulares- articular surfaces Caput articulare – articular head Fossa (fovea) articularis – articular fossa Cartilago articularis – articular cartilage Capsula articularis – articular capsule (joint capsule) Membrana fibrosa, stratum fibrosum– fibrous membrane, layer Membrana synovialis, stratum synoviale – synovial membrane, inner layer Plicae synoviales Villi synoviales Synovia – synovial fluid Rete articulare – articular network of arteries Cavitas articularis – articular cavity, joint cavity Additional joint structures, features of the joint Labrum articulare - Disci et menisci – articular discs and meniscs (difference) Ligamenta - ligaments -

Nettersanatomyflashcards Sa
Study smart with Student CONSULT Elsevier / StudentConsult.com Transform the way you learn. Compatible with PC, Mac®, most mobile devices, and eReaders, Student Consult allows you to browse, search, and interact with this title – online and offline. Redeem your PIN at studentconsult.com today! PIN REDEMPTION INSTRUCTIONS Start using these innovative features today: • Seamless, real-time integration 1. Login or Sign Up at between devices StudentConsult.com • Straightforward navigation and search 2. Scratch off your PIN code • Notes and highlights sharing with below other users through social media 3. Enter PIN into the “Redeem • Self-assessment tools such as a Book Code” box questions embedded within the text 4. Click “Redeem” and multiple-format quizzes * 5. Go to “My Library” * some features vary by title Use of the current edition of the electronic version of this book (eBook) is subject to the terms of the nontransferable, limited license granted on StudentConsult.com. Access to the eBook is limited to the first individual who redeems the PIN, located on the inside cover of this book, at StudentConsult.com and may not be transferred to another party by resale, lending, or other means. For technical assistance: Email: [email protected]; Call: within the US and Canada: 800-401-9962; outside the US and Canada: +1-314-447-8200 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 NETTER’S ANATOMY FLASH CARDS, FOURTH EDITION ISBN: 978-0-323-18595-0 Copyright © 2014, 2011, 2007, 2002 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers. -

Anatomical and Congenital Variations of Styloid Process of Temporal Bone in Indian Adult Dry Skull Bones
IJAE Vol. 124, n. 3: 509-516, 2019 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Original research article Anatomical and Congenital Variations of Styloid Process of Temporal Bone in Indian Adult Dry Skull Bones 1, 2 3 Kalyan Chakravarthi Kosuri *, Venumadhav Nelluri , Siddaraju KS 1 Associate Professor, Department of Anatomy, Varun Arjun Medical College, Banthra-Shajahanpur - 242307, Uttar Pradesh, India 2 Assistent professor, Department of Anatomy, Melaka Manipal Medical College (MMMC), Manipal University, Manipal, and Karnataka, India 3 Lecturer, Department of Anatomy, KMCT Medical College, Manassery, Calicut, Kerala, India Abstract Background: Styloid process of temporal bone is clinically significant, because of anatomical or congenital variations in length, number, angulations as well as close proximity to many of the vital neurovascular structures in the neck. Abnormal or congenital variations of the sty- loid process may compress adjacent neurovascular structures and leads to symptoms of sty- lalgia (Eagle’s syndrome). Aim: Accordingly this study was aimed to evaluate the anatomical and congenital variations of styloid process of temporal bone in Indian adult dry skull bones. Materials and Methods: This study was carried out on 110 dry human skulls irrespective of age and sex at Varun Arjun medical college- Banthra,-UP, Melaka Manipal Medical College- Manipal and KMCT Medical College, Manassery- Calicut. All the skulls were macroscopi- cally inspected for the anatomical and congenital variations of styloid process of temporal bone. Photographs of the anatomical and congenital variations were taken for proper docu- mentation. Results: Out of 110 dry human skull bones we noted very rare unusual unilateral triple styloid processes in one skull bone, unusual bilateral double styloid processes in one skull bone and unilateral double styloid processes in right side of one skull bone.