University of Florida Thesis Or Dissertation Formatting Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of the Binding Partners for Hspb2 and Cryab Reveals
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2013-12-12 Identification of the Binding arP tners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non- Redundant Roles for Small Heat Shock Proteins Kelsey Murphey Langston Brigham Young University - Provo Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Microbiology Commons BYU ScholarsArchive Citation Langston, Kelsey Murphey, "Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins" (2013). Theses and Dissertations. 3822. https://scholarsarchive.byu.edu/etd/3822 This Thesis is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston A thesis submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Master of Science Julianne H. Grose, Chair William R. McCleary Brian Poole Department of Microbiology and Molecular Biology Brigham Young University December 2013 Copyright © 2013 Kelsey Langston All Rights Reserved ABSTRACT Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactors and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston Department of Microbiology and Molecular Biology, BYU Master of Science Small Heat Shock Proteins (sHSP) are molecular chaperones that play protective roles in cell survival and have been shown to possess chaperone activity. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
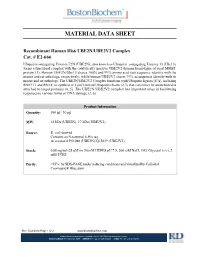
Material Data Sheet
MATERIAL DATA SHEET Recombinant Human His6 UBE2N/UBE2V2 Complex Cat. # E2666 Ubiquitin conjugating Enzyme E2N (UBE2N), also known as Ubiquitin conjugating Enzyme 13 (Ubc13), forms a functional complex with the catalytically inactive UBE2V2 (human homologue of yeast MMS2) protein (1). Human UBE2N/Ubc13 shares 100% and 99% amino acid (aa) sequence identity with the mouse and rat orthologs, respectively, while human UBE2V2 shares 99% aa sequence identity with its mouse and rat orthologs. The UBE2N/UBE2V2 Complex functions with Ubiquitin ligases (E3s), including RNF111 and RNF8, to synthesize Lys63linked Ubiquitin chains (2,3) that can either be unanchored or attached to target proteins (4, 5). The UBE2N/UBE2V2 complex has important roles in facilitating responses to various forms of DNA damage (2, 6). Product Information Quantity: 100 µg | 50 µg MW: 18 kDa (UBE2N), 17 kDa (UBE2V2) Source: E. coliderived Contains an Nterminal 6His tag Accession # P61088 (UBE2N)/Q15819 (UBE2V2) Stock: 0.88 mg/ml (25 μM) in 50 mM HEPES pH 7.5, 200 mM NaCl, 10% Glycerol (v/v), 2 mM TCEP Purity: >95%, by SDSPAGE under reducing conditions and visualized by Colloidal Coomassie® Blue stain. Rev. 5/22/2014 Page 1 of 2 www.bostonbiochem.com Boston Biochem products are available via the R&D Systems distributor network. USA & CANADA Tel: (800) 343-7475 EUROPE Tel: +44 (0)1235 529449 CHINA Tel: +86 (21) 52380373 Use & Storage Use: Recombinant Human His6UBE2N/UBE2V2 Complex is a member of the Ubiquitin conjugating (E2) enzyme family that receives Ubiquitin from a Ubiquitin activating (E1) enzyme and subsequently interacts with a Ubiquitin ligase (E3) to conjugate Ubiquitin to substrate proteins. -

The Ubiquitination Enzymes of Leishmania Mexicana
The ubiquitination enzymes of Leishmania mexicana Rebecca Jayne Burge Doctor of Philosophy University of York Biology October 2020 Abstract Post-translational modifications such as ubiquitination are important for orchestrating the cellular transformations that occur as the Leishmania parasite differentiates between its main morphological forms, the promastigote and amastigote. Although 20 deubiquitinating enzymes (DUBs) have been partially characterised in Leishmania mexicana, little is known about the role of E1 ubiquitin-activating (E1), E2 ubiquitin- conjugating (E2) and E3 ubiquitin ligase (E3) enzymes in this parasite. Using bioinformatic methods, 2 E1, 13 E2 and 79 E3 genes were identified in the L. mexicana genome. Subsequently, bar-seq analysis of 23 E1, E2 and HECT/RBR E3 null mutants generated in promastigotes using CRISPR-Cas9 revealed that the E2s UBC1/CDC34, UBC2 and UEV1 and the HECT E3 ligase HECT2 are required for successful promastigote to amastigote differentiation and UBA1b, UBC9, UBC14, HECT7 and HECT11 are required for normal proliferation during mouse infection. Null mutants could not be generated for the E1 UBA1a or the E2s UBC3, UBC7, UBC12 and UBC13, suggesting these genes are essential in promastigotes. X-ray crystal structure analysis of UBC2 and UEV1, orthologues of human UBE2N and UBE2V1/UBE2V2 respectively, revealed a heterodimer with a highly conserved structure and interface. Furthermore, recombinant L. mexicana UBA1a was found to load ubiquitin onto UBC2, allowing UBC2- UEV1 to form K63-linked di-ubiquitin chains in vitro. UBC2 was also shown to cooperate with human E3s RNF8 and BIRC2 in vitro to form non-K63-linked polyubiquitin chains, but association of UBC2 with UEV1 inhibits this ability. -

WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/079361 Al 25 April 2019 (25.04.2019) W 1P O PCT (51) International Patent Classification: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, C12Q 1/68 (2018.01) A61P 31/18 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, C12Q 1/70 (2006.01) HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/US2018/056167 OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (22) International Filing Date: SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 16 October 2018 (16. 10.2018) TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, (30) Priority Data: UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, 62/573,025 16 October 2017 (16. 10.2017) US TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, ΓΕ , IS, IT, LT, LU, LV, (71) Applicant: MASSACHUSETTS INSTITUTE OF MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, TECHNOLOGY [US/US]; 77 Massachusetts Avenue, TR), OAPI (BF, BJ, CF, CG, CI, CM, GA, GN, GQ, GW, Cambridge, Massachusetts 02139 (US). -

Monoclonal Anti-Human Adipon
monocl AAD0602 Monoclonal anti-adiponectin antibody (clone 1G12) 100ul 311-Eur ATGen onal monocl AAD0602 Monoclonal anti-adiponectin antibody (clone 1G12) 50ul 227-Eur ATGen onal monocl AAD0614 Monoclonal anti-human adiponectin antibody (clone 5H7) 100ul 311-Eur ATGen onal monocl AAD0614 Monoclonal anti-human adiponectin antibody (clone 5H7) 50ul 227-Eur ATGen onal monocl AAK0604 Monoclonal anti-human AK3 antibody (clone SJB3-36) 100ul 354-Eur ATGen onal monocl AAK0604 Monoclonal anti-human AK3 antibody (clone SJB3-36) 50ul 252-Eur ATGen onal monocl AAP0501 Monoclonal anti-human ANGPTL3 antibody (clone 1D10 ) 100ul 284-Eur ATGen onal monocl AAP0501 Monoclonal anti-human ANGPTL3 antibody (clone 1D10 ) 50ul 191-Eur ATGen onal monocl AAP0501 Monoclonal anti-human ANGPTL3 antibody (clone 1D10) 100ul 311-Eur ATGen onal monocl AAP0501 Monoclonal anti-human ANGPTL3 antibody (clone 1D10) 50ul 227-Eur ATGen onal monocl AAP0836 Monoclonal anti-human APP antibody (clone J4H9) 100ul 311-Eur ATGen onal monocl AAP0836 Monoclonal anti-human APP antibody (clone J4H9) 50ul 227-Eur ATGen onal monocl ABH0708 Monoclonal anti-human BHMT antibody (clone 3D6 ) 100ul 284-Eur ATGen onal monocl ABH0708 Monoclonal anti-human BHMT antibody (clone 3D6 ) 50ul 191-Eur ATGen onal monocl ABH0708 Monoclonal anti-human BHMT antibody (clone 3D6) 100ul 311-Eur ATGen onal monocl ABH0708 Monoclonal anti-human BHMT antibody (clone 3D6) 50ul 227-Eur ATGen onal monocl ABI0923 Monoclonal anti-human BID antibody (clone 4D3) 100ul 284-Eur ATGen onal monocl ABI0923 Monoclonal anti-human -

UBE2V2 Rabbit Pab
Leader in Biomolecular Solutions for Life Science UBE2V2 Rabbit pAb Catalog No.: A6998 Basic Information Background Catalog No. Ubiquitin-conjugating enzyme E2 variant proteins constitute a distinct subfamily within A6998 the E2 protein family. They have sequence similarity to other ubiquitin-conjugating enzymes but lack the conserved cysteine residue that is critical for the catalytic activity of Observed MW E2s. The protein encoded by this gene also shares homology with ubiquitin-conjugating 16kDa enzyme E2 variant 1 and yeast MMS2 gene product. It may be involved in the differentiation of monocytes and enterocytes. Calculated MW 16kDa Category Primary antibody Applications WB, IHC Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 7336 Q15819 IHC 1:50 - 1:200 Immunogen Recombinant fusion protein containing a sequence corresponding to amino acids 1-145 of human UBE2V2 (NP_003341.1). Synonyms UBE2V2;DDVIT1;DDVit-1;EDAF-1;EDPF-1;EDPF1;MMS2;UEV-2;UEV2 Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using UBE2V2 antibody (A6998) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 90s. Immunohistochemistry of paraffin- embedded rat spleen using UBE2V2 antibody (A6998) at dilution of 1:100 (40x lens). -

In Silico Analysis of Regulatory Networks Underlines the Role of Mir-10B-5P and Its Target BDNF in Huntington’S Disease Sören Müller
Müller Translational Neurodegeneration 2014, 3:17 http://www.translationalneurodegeneration.com/content/3/1/17 Translational Neurodegeneration SHORT REPORT Open Access In silico analysis of regulatory networks underlines the role of miR-10b-5p and its target BDNF in huntington’s disease Sören Müller Abstract Non-coding RNAs (ncRNAs) play various roles during central nervous system development. MicroRNAs (miRNAs) are a class of ncRNAs that exert their function together with argonaute proteins by post-transcriptional gene silencing of messenger RNAs (mRNAs). Several studies provide evidence for alterations in miRNA expression in patients with neurodegenerative diseases. Among these is huntington‘s disease (HD), a dominantly inherited fatal disorder characterized by deregulation of neuronal-specific mRNAs as well as miRNAs. Recently, next-generation sequencing (NGS) miRNA profiles from human HD and neurologically normal control brain tissues were reported. Five consistently upregulated miRNAs affect the expression of genes involved in neuronal differentiation, neurite outgrowth, cell death and survival. We re-analyzed the NGS data publicly available in array express and detected nineteen additional differentially expressed miRNAs. Subsequently, we connected these miRNAs to genes implicated in HD development and network analysis pointed to miRNA-mediated downregulation of twenty-two genes with roles in the pathogenesis as well as treatment of the disease. In silico prediction and reporter systems prove that levels of BDNF,a central node in the miRNA-mRNA regulatory network, can be post-transcriptionally controlled by upregulated miR-10b-5p and miR-30a-5p. Reduced BDNF expression is associated with neuronal dysfunction and death in HD. Moreover, the 3’UTR of CREB1 harbors a predicted binding site for these two miRNAs. -

Lessons from the Naked Mole Rat
International Journal of Molecular Sciences Review DNA Homeostasis and Senescence: Lessons from the Naked Mole Rat Harvey Boughey 1,†, Mateusz Jurga 2,† and Sherif F. El-Khamisy 1,2,* 1 The Healthy Lifespan Institute and the Institute of Neuroscience, University of Sheffield, Sheffield S10 2TN, UK; hboughey1@sheffield.ac.uk 2 The Institute of Cancer Therapeutics, University of Bradford, Bradford BD7 1DP, UK; [email protected] * Correspondence: s.el-khamisy@sheffield.ac.uk; Tel.: +44-(0)-114-2222-791; Fax: +44-(0)-114-222-2850 † These authors contributed equally. Abstract: As we age, our bodies accrue damage in the form of DNA mutations. These mutations lead to the generation of sub-optimal proteins, resulting in inadequate cellular homeostasis and senescence. The build-up of senescent cells negatively affects the local cellular micro-environment and drives ageing associated disease, including neurodegeneration. Therefore, limiting the accumulation of DNA damage is essential for healthy neuronal populations. The naked mole rats (NMR) are from eastern Africa and can live for over three decades in chronically hypoxic environments. Despite their long lifespan, NMRs show little to no biological decline, neurodegeneration, or senescence. Here, we discuss molecular pathways and adaptations that NMRs employ to maintain genome integrity and combat the physiological and pathological decline in organismal function. Keywords: naked mole rat; senescence; neurodegeneration; ageing; DNA damage; DNA repair; oxidative stress; reactive oxygen species Citation: Boughey, H.; Jurga, M.; El-Khamisy, S.F. DNA Homeostasis and Senescence: Lessons from the 1. Introduction Naked Mole Rat. Int. J. Mol. Sci. 2021, An exposure to low oxygen conditions (hypoxia) perturbs oxidative phosphorylation, 22, 6011. -

S41467-019-12388-Y.Pdf
ARTICLE https://doi.org/10.1038/s41467-019-12388-y OPEN A tri-ionic anchor mechanism drives Ube2N-specific recruitment and K63-chain ubiquitination in TRIM ligases Leo Kiss1,4, Jingwei Zeng 1,4, Claire F. Dickson1,2, Donna L. Mallery1, Ji-Chun Yang 1, Stephen H. McLaughlin 1, Andreas Boland1,3, David Neuhaus1,5 & Leo C. James1,5* 1234567890():,; The cytosolic antibody receptor TRIM21 possesses unique ubiquitination activity that drives broad-spectrum anti-pathogen targeting and underpins the protein depletion technology Trim-Away. This activity is dependent on formation of self-anchored, K63-linked ubiquitin chains by the heterodimeric E2 enzyme Ube2N/Ube2V2. Here we reveal how TRIM21 facilitates ubiquitin transfer and differentiates this E2 from other closely related enzymes. A tri-ionic motif provides optimally distributed anchor points that allow TRIM21 to wrap an Ube2N~Ub complex around its RING domain, locking the closed conformation and promoting ubiquitin discharge. Mutation of these anchor points inhibits ubiquitination with Ube2N/ Ube2V2, viral neutralization and immune signalling. We show that the same mechanism is employed by the anti-HIV restriction factor TRIM5 and identify spatially conserved ionic anchor points in other Ube2N-recruiting RING E3s. The tri-ionic motif is exclusively required for Ube2N but not Ube2D1 activity and provides a generic E2-specific catalysis mechanism for RING E3s. 1 Medical Research Council Laboratory of Molecular Biology, Cambridge, UK. 2Present address: University of New South Wales, Sydney, NSW, Australia. 3Present address: Department of Molecular Biology, Science III, University of Geneva, Geneva, Switzerland. 4These authors contributed equally: Leo Kiss, Jingwei Zeng. 5These authors jointly supervised: David Neuhaus, Leo C. -

Antigens STAT1, 1-712Aa, Human, His Tag, E.Coli, Recombinant Monoclonal Antibody Anti-CD34 Polyclonal Antibody Anti-Decorin
Antigens STAT1, 1-712aa, Human, His tag, E.coli, 01-0102 Recombinant 10 193-Eur ARP 01-0395M Monoclonal antibody Anti-CD34 200 μl 237-Eur ARP 01-1001G Polyclonal antibody Anti-Decorin, Mouse 200 237-Eur ARP 01-1001M Monoclonal antibody Anti-Decorin, human 50 270-Eur ARP 01-1002 Antigens Decorin, mouse 100 237-Eur ARP 01-1002R Monoclonal antibody Anti-Decorin, Mouse 200 270-Eur ARP 01-1244 Polyclonal antibody Anti-Presenilin 1, C-terminal 100 237-Eur ARP 01-1245 Polyclonal antibody Anti-Presenilin 1, N-terminal 200 237-Eur ARP Polyclonal antibody Anti- Hepatocyte Growth Factor alpha 01-1358 (HGF alpha) 200 237-Eur ARP 01-1541 Polyclonal antibody Anti-SHMT1 (Cytoplasma) 200 237-Eur ARP Antigens Thiosulfate sulfurtransferase, 1-297 aa, Human, 01-1742 E.coli, Recombinant 50 215-Eur ARP Antigens GAMT, 1-236aa, Human, His tag, E.coli, 01-1743 Recombinant 20 193-Eur ARP Antigens Stress-induced-phosphoprotein 1, 1- 01-1744 543aa,Human, His tag, E.coli, Recombinant 10 215-Eur ARP 01-1745 Antigens SKP1, 1- 160aa, Human, E.coli, Recombinant 20 193-Eur ARP Antigens Alcohol dehydrogenase, 1-325aa, Human, E.coli, 01-1746 Recombinant 10 193-Eur ARP Antigens ATOX1, 1-68aa, Human, His tag, E.coli, 01-1747-1 Recombinant 10 193-Eur ARP Antigens Ketohexokinase, 1-298aa, Human, E.coli, 01-1748 Recombinant 20 193-Eur ARP Antigens BAALC, 1-145aa, Human, His tag, E.coli, 01-1749 Recombinant 20 281-Eur ARP 01-1750 Antigens CAPG, 1-348aa, Human, E.coli, Recombinant 10 193-Eur ARP 01-1751-1 Antigens BAG1, 1-230aa, Human, E.coli, Recombinant 10 226-Eur ARP Antigens -

Comparative Analysis of the Ubiquitin-Proteasome System in Homo Sapiens and Saccharomyces Cerevisiae
Comparative Analysis of the Ubiquitin-proteasome system in Homo sapiens and Saccharomyces cerevisiae Inaugural-Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultät der Universität zu Köln vorgelegt von Hartmut Scheel aus Rheinbach Köln, 2005 Berichterstatter: Prof. Dr. R. Jürgen Dohmen Prof. Dr. Thomas Langer Dr. Kay Hofmann Tag der mündlichen Prüfung: 18.07.2005 Zusammenfassung I Zusammenfassung Das Ubiquitin-Proteasom System (UPS) stellt den wichtigsten Abbauweg für intrazelluläre Proteine in eukaryotischen Zellen dar. Das abzubauende Protein wird zunächst über eine Enzym-Kaskade mit einer kovalent gebundenen Ubiquitinkette markiert. Anschließend wird das konjugierte Substrat vom Proteasom erkannt und proteolytisch gespalten. Ubiquitin besitzt eine Reihe von Homologen, die ebenfalls posttranslational an Proteine gekoppelt werden können, wie z.B. SUMO und NEDD8. Die hierbei verwendeten Aktivierungs- und Konjugations-Kaskaden sind vollständig analog zu der des Ubiquitin- Systems. Es ist charakteristisch für das UPS, daß sich die Vielzahl der daran beteiligten Proteine aus nur wenigen Proteinfamilien rekrutiert, die durch gemeinsame, funktionale Homologiedomänen gekennzeichnet sind. Einige dieser funktionalen Domänen sind auch in den Modifikations-Systemen der Ubiquitin-Homologen zu finden, jedoch verfügen diese Systeme zusätzlich über spezifische Domänentypen. Homologiedomänen lassen sich als mathematische Modelle in Form von Domänen- deskriptoren (Profile) beschreiben. Diese Deskriptoren können wiederum dazu verwendet werden, mit Hilfe geeigneter Verfahren eine gegebene Proteinsequenz auf das Vorliegen von entsprechenden Homologiedomänen zu untersuchen. Da die im UPS involvierten Homologie- domänen fast ausschließlich auf dieses System und seine Analoga beschränkt sind, können domänen-spezifische Profile zur Katalogisierung der UPS-relevanten Proteine einer Spezies verwendet werden. Auf dieser Basis können dann die entsprechenden UPS-Repertoires verschiedener Spezies miteinander verglichen werden.