Five-Year Evaluation of Premarital Screening Program for Hemoglobinopathies in the Province of Mersin, Turkey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ENVIRONMENTAL PRODUCT DECLARATION for Portland
ENVIRONMENTAL PRODUCT DECLARATION for Portland Cement Clinker in accordance with ISO14025 and EN15804:2012+A2:2019 Programme : The International EPD® System www.environdec.com Programme Operator : EPD International AB Stockholm, Sweden EPD Registration Number: S-P-02229 Publication Date: 23.02.2021 Validity Date: 22.02.2026 Geographical Scope: Turkey PROGRAMME INFORMATION EPD Turkey, a fully aligned The International EPD® System regional programme EPD International AB SÜRATAM – Turkish Centre for Sustainable Box 210 60 Production Research & Design SE-100 31 Programme Nef 09 B Blok No:7/15 Stockholm/SWEDEN 34415 Kağıthane-Istanbul/TURKEY www.epdturkey.org www.environdec.com [email protected] [email protected] Product Category Rules (PCR): 2019:14 Version 1.1. 2020-09-14 Construction Products EN 15804:2012 + A2:2019 Sustainability of Construction Works Independent third-party verification of the declaration and data, according to ISO 14025:2006 EPD process certification X EPD verification Third party verifier: Vladimír Kočí, PhD Approved by: The International EPD® System Procedure for follow-up of data during EPD validity involves third party verifier: Yes No The EPD owner has the sole ownership, liability, and responsibility for the EPD. EPDs within the same product category but from different programmes may not be comparable. EPDs of construction products may not be comparable if they do not comply with EN 15804. For further information about comparability, see EN 15804 and ISO 14025. 2 ABOUT THE COMPANY Medcem Cement Factory, a subsidiary of Eren Holding, started production in July 2015 in Akdere/Silifke district of Mersin province. With a daily production capacity of 11,500 tons of clinker, Medcem Çimento is the biggest cement factory of Turkey and Europe with the highest production volume on a single line. -

Analysis of Irrigation Water Quality in Silifke-Mersin Province, Turkey
World Journal of Innovative Research (WJIR) ISSN: 2454-8236, Volume-5, Issue-1, July 2018 Pages 35-39 Analysis of Irrigation Water Quality in Silifke-Mersin Province, Turkey Ahmet Melih Yılmaz, Didem Rabia DEMİR limited under the conditions of water deficiency through the Abstract— This study was performed to identify the root zone [8]. Irrigation is technological practice improving irrigation water quality of groundwater resources used in the crop yield as well as quality under the correct irrigation of some vegetable plants and their effect on soil management [9]. In order to obtain maximum profits from salinity at plastic houses. Water samples were taken from the current water supplies, special cares are needed especially groundwater resources. In addition, soil samples were taken in the water distribution and water use in field level [10]. from the research sites at 0-30 cm soil depth for determination Irrigation is vital important to improve the crop production in of chemical and physical properties of research soils. In results, soil textures varied from Sandy-Clay-Loam (SCL) to Loam (L). arid or semi-arid lands. In most parts of the Turkey such The pH and Electrical Conductivity, EC, of soils within the Konya plain, it is impossible to obtain economical crop yields plastic houses varied from 7.36 to 7.66 and from 375 to 3449 without irrigation even for winter cereals. Therefore, water μmhos/cm, respectively. Those parameters for water samples resources in such regions have to be managed properly for varied from 7.15 to 8.03 and from 437 to 2103 μmhos/cm, sustainable agricultural water management [11]. -
![T-PVS/Files(2021)29 [Files29e 2021.Docx]](https://docslib.b-cdn.net/cover/3257/t-pvs-files-2021-29-files29e-2021-docx-1083257.webp)
T-PVS/Files(2021)29 [Files29e 2021.Docx]
Strasbourg, 13 August 2021 T-PVS/Files(2021)29 [files29e_2021.docx] CONVENTION ON THE CONSERVATION OF EUROPEAN WILDLIFE AND NATURAL HABITATS Standing Committee 41st meeting Strasbourg, 29 November – 3 December 2021 __________ Possible File: 2019/05 Habitat destruction in Mersin Anamur Beach (Turkey) - REPORT BY THE GOVERNMENT - Document prepared by Ministry of Agriculture and Forestry, Turkey ____________________________________________________________________ T-PVS/Files(2021)29 REPUBLIC OF TURKEY MINISTRY OF AGRICULTURE AND FORESTRY 06.08.2021 Government Report on the Complaint submitted by Mersin Environment and Nature Association and Medasset Regarding The Activities Done by Anamur Municipality on Anamur Beach of Mersin Province Background: This complaint was first raised in the summer of 2019. As soon as the complaint was reported to the Mersin Provincial Directorate of the Ministry of Agriculture and Forestry, the case was inspected by the Directorate and finally, the municipality was fined about 180.000 Turkish Liras on the basis of Turkish Environmental Law. (No. 2872) The municipality was also obliged to rehabilitate the area. However, the Municipality refused to pay the fine and appealed to the administrative court. The National Court made its decision in January 2021 and it ruled to dismiss the appeal filed by the Municipality with the decision no K.2020/1054. In view of the bilateral interviews between the General Directorate of Nature Conservation and National Parks and the complainant Association, it was decided that the rehabilitation must be done within the scope of the principals determined by a group of experts, so as to mitigate further degradation on the beach due to the heavy machinery activities. -

Beyobasi Enerji Uretim As Otluca Hepp
Public Disclosure Authorized BEYOBASI ENERJI URETIM A.S. OTLUCA HEPP, ANAMUR RIVER IN MERSIN PROVINCE Public Disclosure Authorized REPORTING FORM FOR LAND ACQUISITION / SOCIAL IMPACTS OF PORTFOLIO PROJECTS Public Disclosure Authorized Public Disclosure Authorized Reporting Form for Land Acquisition / Social Impacts of Portfolio Projects. Name & Location of Sub-project: Otluca HEPP, Anamur River in Mersin Province. Project Sponsor: Beyobası Enerji Üretim A.Ş. is the owner of the Otluca HEPP project. Beyobası Enerji Üretim A.Ş., established in 1999, joined Akfen Group in 2007. The company is established to generate electricity with hydroelectric power plants and carrying out Otluca HEPP investment in Mersin/Anamur, Sırma HEPP investment in Aydın, Yuvarlakçay HEPP investment in Muğla and Sekiyaka HEPP in Muğla. Project cost: The investment cost of Otluca HEPP is 48.993.770 € (VAT and interest cost are not included) Installed generation capacity (No. units X MW/unit): Otluca HEPP: a run-of-the river 44,72 MW hydropower plant. Otluca 1 uses the water of the Anamur River and is a medium head plant using a weir structure to divert river water into an intake structure with three de-sanding basins. From there, it enters a tunnel of about 3.896 m length followed by an open canal of about 500 m length and followed again by a tunnel of about 2.209 m length until the water reaches a headpond. An intake from this pond takes it through a 507 m long penstock to the powerhouse with 3 Francis turbines of about 11,9 MW each, i.e. the total capacity with 208,65 m head is 35,62 MW. -
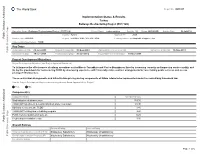
Implementation Status & Results
The World Bank Report No: ISR5357 Implementation Status & Results Turkey Railways Restructuring Project (P077328) Operation Name: Railways Restructuring Project (P077328) Project Stage: Implementation Seq.No: 12 Status: ARCHIVED Archive Date: 08-Jul-2012 Country: Turkey Approval FY: 2005 Public Disclosure Authorized Product Line:IBRD/IDA Region: EUROPE AND CENTRAL ASIA Lending Instrument: Adaptable Program Loan Implementing Agency(ies): TCDD Key Dates Board Approval Date 09-Jun-2005 Original Closing Date 30-Sep-2009 Planned Mid Term Review Date Last Archived ISR Date 19-Nov-2011 Public Disclosure Copy Effectiveness Date 19-Jun-2006 Revised Closing Date 30-Jun-2012 Actual Mid Term Review Date 10-Nov-2008 Project Development Objectives Project Development Objective (from Project Appraisal Document) To (a) improve the effectiveness of railway operations on the Mersin-Toprakkale and Yenice-Bogazkopru lines by increasing capacity and improving service quality, and (b) lay the groundwork for restructuring TCDD by developing experience with financially viable contract arrangements for loss making public services and access pricing of infrastructure. These contractual arrangements and infrastructure pricing are key components of future reform to be implemented under the new railway framework law. Public Disclosure Authorized Has the Project Development Objective been changed since Board Approval of the Project? ● Yes No Component(s) Component Name Component Cost Modernization of infrastructure 159.30 TCDD staff adjustment & social mitigation -

Identification of Banana Accessions Sampled from Subtropical Region of Turkey Using Srap Markers
270 Bulgarian Journal of Agricultural Science, 21 (No 2) 2015, 270–276 Agricultural Academy IDENTIFICATION OF BANANA ACCESSIONS SAMPLED FROM SUBTROPICAL REGION OF TURKEY USING SRAP MARKERS H. PINAR,1 A. UZUN2*, M. UNLU1, M. BIRCAN1, O. GULSEN2, C. YILMAZ3 and H. GUBBUK4 1 Alata Horticultural Research Station, Mersin, Turkey 2 Erciyes University Department of Horticulture, Kayseri, Turkey 3 Osmangazi University Department of Horticulture, Eskisehir, Turkey 4 Akdeniz University Department of Horticulture, Antalya, Turkey Abstract PINAR, H., A. UZUN, M. UNLU, M. BIRCAN, O. GULSEN, C. YILMAZ and H. GUBBUK, 2015. Identifi cation of banana accessions sampled from subtropical region of Turkey using srap markers. Bulg. J. Agric. Sci., 21: 270–276 This study was conducted to estimate genetic relationships and natural somatic mutations among selected banana geno- types from different region of Turkey via SRAP molecular markers. Ninety-six banana genotypes including 39 ‘Dwarf Caven- dish’, 18 ‘Grande Nain’, 28 ‘Azman’ and 11 other bananas were evaluated. A total of 102 bands were obtained from 19 SRAP primer combinations and 86 (85.5%) of them were polymorphic. Number of bands per primer combination was 5.3 whereas polymorphic bands per primer combinations were 4.5. Genetic similarity of 96 accessions varied between 0.63–1.00. It was determined genetic variation among the accessions which may allow new selections for breeding programs. Considerable variation was also found among genotypes within the same banana cultivar and it was very important for banana breeding and germplasm evaluation. It can be concluded that SRAP markers could readily be used to estimate genetic relationhips among banana genotypes and natural somatic mutations. -

The Effect of Organic Waste Potential of Mersin Province on Biogas Energy Production Mersin Ilinin Organik Atık Potansiyelinin Biyogaz Enerji Üretimine Etkisi
POLİTEKNİK DERGİSİ JOURNAL of POLYTECHNIC ISSN: 1302-0900 (PRINT), ISSN: 2147-9429 (ONLINE) URL: http://dergipark.org.tr/politeknik The effect of organic waste potential of Mersin province on biogas energy production Mersin ilinin organik atık potansiyelinin biyogaz enerji üretimine etkisi Yazar(lar) (Author(s)): Bekir YELMEN1, Metin DAĞTEKİN2, M.Tarık ÇAKIR3 ORCID1: 0000-0001-7655-530X ORCID2: 0000-0002-1397-1725 ORCID3: 0000-0002-0107-594X Bu makaleye şu şekilde atıfta bulunabilirsiniz (To cite to this article): Yelmen B., Dağtekin M. ve Çakır M.T., “Mersin ilinin organik atık potansiyelinin biyogaz enerji üretimine etkisi”, Politeknik Dergisi, 23(2): 587-595, (2020). Erişim linki (To link to this article): http://dergipark.org.tr/politeknik/archive DOI: 10.2339/politeknik.645309 Politeknik Dergisi, 2020; 23(2) : 587-595 Journal of Polytechnic, 2020; 23 (2): 587-595 Mersin İlinin Organik Atık Potansiyelinin Biyogaz Enerji Üretimine Etkisi Araştırma Makalesi / Research Article Bekir YELMEN1*, Metin DAGTEKİN2, Tarık M. ÇAKIR3 1Adana Büyükşehir Belediyesi, Çevre Koruma Kontrol Dairesi Bşk., AAT, Türkiye 2Çukurova Üniversitesi, Ceyhan Meslek Yüksekokulu, Türkiye 3T.C.Sağlık Bakanlığı,TUSEB, Türkiye (Geliş/Received : 11.04.2019 ; Kabul/Accepted : 06.06.2019) ÖZ Bu çalışmanın amacı; Mersin ilinde bitkisel, hayvansal, mutfak ve endüstriyel arıtma çamuru tesislerinden elde edilen organik atıkların mevcut durumu ve biyogaz enerji üretim potansiyelini belirlemek ve konuya ilişkin yerel ölçekte sürdürülebilir çözümler oluşturmaktır. Çalışmada hayvan ve bitkilere ait veriler Mersin İl Tarım ve Orman Müdürlüğünden, mutfak ve endüstriyel atıklara ilişkin veriler ise Mersin Büyükşehir Belediyesinden alınmıştır. Çalışma sonucunda, Mersin ilinde hayvansal, bitkisel, mutfak ve arıtma çamuru tesisinde üretilen günlük organik madde miktarının 16801.48 ton olduğu ve bu atıklardan üretilen biyogaz miktarının 557432.47 m3, metandan üretilen elektrik enerjisi ise 2619.93 MWh olarak elde edilebilecektir. -
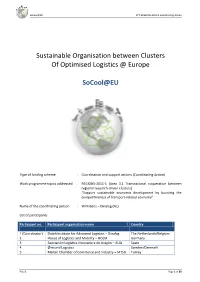
Socool@EU FP7-REGIONS-2011-1 Coordinating Action
SoCool@EU FP7-REGIONS-2011-1 Coordinating Action Sustainable Organisation between Clusters Of Optimised Logistics @ Europe SoCool@EU Type of funding scheme : Coordination and support actions (Coordinating Action) Work programme topics addressed : REGIONS-2011-1 (Area 3.1 Transnational cooperation between regional research-driven clusters) “Support sustainable economic development by boosting the competitiveness of transport-related economy” Name of the coordinating person : Wim Bens – Dinalog (NL) List of participants Participant no. Participant organisation name Country 1 (Coordinator) Dutch Institute for Advanced Logistics – Dinalog The Netherlands/Belgium 2 House of Logistics and Mobility – HOLM Germany 3 Asociación Logística Innovadora de Aragón – ALIA Spain 4 Øresund Logistics Sweden/Denmark 5 Mersin Chamber of Commerce and Industry – MTSO Turkey Part B Page 1 of 80 SoCool@EU FP7-REGIONS-2011-1 Coordinating Action Table of contents B1 Scientific and/or technical quality ......................................................................................................... 3 B1.0 Executive summary ............................................................................................................................ 3 B1.1 Concept and objectives ..................................................................................................................... 3 B1.1.1 Concept and main ideas ............................................................................................................ 3 B1.1.2 Objectives ................................................................................................................................. -

Article1380804221 Son.Pdf
African Journal of Agricultural Research Vol. 5(10), pp. 1144-1146, 18 May, 2010 Available online at http://www.academicjournals.org/AJAR DOI: 10.5897/AJAR09.556 ISSN 1991-637X © 2010 Academic Journals Short Communication Determination on quality characteristics of some important Japanese plum (Prunus Salicina Lindl.) cultivars grown in Mersin-Turkey Levent Son Department of Horticulture, High School of Mut, University of Mersin33600, Mut-Mersin, Turkey. E-mail: [email protected]. Accepted 20 April, 2010 This experiment was conducted in Mut-Mersin from 2008 to 2009 to determine the phenological and pomological characteristics of ‘Angeleno’, ‘Autumn Giant’, ‘Bella Di Barbiano’, ‘Black Amber’, ‘Black Beauty’, ‘Black Diamond’, ‘Fortune’, ‘Globe Sun’, ‘Obilnaja’, ‘October Sun’, ‘Original Sun’ ‘President’, ‘Queen Rosa’ and ‘T.C Sun’ Japanese plum (Prunus salicina Lindl) cultivars. In the experimental years, flowering periods, harvesting date, fruit dimensions, fruit weight, seed weight, flesh/seed ratio, total soluble solid contents (TSS%) and acidity were determined. Fruit weight (g) ranged from 46.71 g (Obilnaja) to 91.26 g (Black Diamond). Among the cultivars tested, ‘Black Diamond’, ‘Queen Rosa’ and ‘October Sun’ had the biggest fruits. Date of full bloom ranged from 13 March for ‘Black Diamond’ to 4 April for ‘T. Sun’. From the results of this research the following conclusions were determined: 1) Fruit maturation were earlier on ‘Black Beauty’ and ‘Obilnaja’ cultivars than the other cultivars. 2) In terms of fruit weights ‘Black Diamond’, ‘Queen Rosa’, ‘October Sun’ and ‘Autumn Giant’ were bigger than the other cultivars. Key words: Japanese plum, fruit quality, fruit weight INTRODUCTION Prunus cerasifera, P. -

Page De Garde Etudes De Cas Turkie Mersin
SILVA MEDITERRANEA Projet «Forêts méditerranéennes et développement durable » CASE STUDY ASSESSMENT OF SOCIO-ECONOMIC STRUCTURE AND FORESTRY ACTIVITIES IN FOREST VILLAGES IN MERSIN PROVINCE FROM THE POINT OF MEDITERRANEAN FORESTRY Villages : Olukkoyagi, Inköy, Ardiçli, Kesli, Emirler, Eminlik & Kusçular Melekber SULUSOGLU November 2004 SILVA MEDITERRANEA PLAN BLEU/ FAO PROJECT CONTRIBUTION OF FOREST RESOURCES TO SUSTAINABLE DEVELOPMENT A CASE STUDY CONDUCTED IN TURKEY, MERSIN (Villages: Olukkoyagi, Inköy, Ardiçli, Kesli, Emirler, Eminlik and Kusçular ) By Dr.Melekber SÜLÜSOGLU Dr.Ahmet SENYAZ Dr.Ersin YILMAZ CASE STUDY IN TURKEY SUMMARY A case study has been conducted in 7 forest villages of Mersin Province, Tarsus town in Turkey in order to determine contribution of Mediterranean forestry to sustainable development, in particular, livelihoods of forest villagers under the auspices of FAO and Blue Plan. With this study, forest resources and their impacts on forest villagers located in Mediterranean Region were investigated. To this end, opinion of local people, forestry staff and other stakeholders who have interest in forest resource management have been collected by using a participatory method. At the end of the survey sample scenarios for sustainable forestry practices have been formulated for the Region. In addition, attention of local authorities, ministries and related institutions have been drawn in order to build partnership and promote dialogue among them. FRENCH SUMMARY (Villages forestiers de Mersin) Résumé de l’étude : L’étude de cas a été conduite, sous les auspices de la FAO et le plan bleu, dans 7 villages forestiers de la province de Mersin, ville de Tarse en Turquie. L’objectif de l’étude est de déterminer la contribution de la forêt méditerranéenne au développement durable, en particulier, la vie des populations des villages forestiers. -

Tc Süleyman Demirel Üniversitesi Fen Bilimleri Enstitüsü Mersin Ilinin Bazı
T.C. SÜLEYMAN DEMİREL ÜNİVERSİTESİ FEN BİLİMLERİ ENSTİTÜSÜ MERSİN İLİNİN BAZI İLÇELERİNDEKİ ANIT VE ANITSAL NİTELİKLİ AĞAÇLAR Hasan ASLAN Danışman Doç. Dr. İsmail DUTKUNER YÜKSEK LİSANS TEZİ ORMAN MÜHENDİSLİĞİ ANABİLİM DALI ISPARTA ‐ 2016 © 2016 [Hasan ASLAN] İÇİNDEKİLER Sayfa İÇİNDEKİLER ........................................................................................................................... i ÖZET ............................................................................................................................................ ii ABSTRACT ................................................................................................................................ iii TEŞEKKÜR ................................................................................................................................ iv ŞEKİLLER DİZİNİ ................................................................................................................... v ÇİZELGELER DİZİNİ .............................................................................................................. vi SİMGELER VE KISALTMALAR DİZİNİ ........................................................................... viii 1. GİRİŞ ....................................................................................................................................... 1 2. MATERYAL VE METOD .................................................................................................. 5 3. ANIT AĞAÇ SEÇİMİ İÇİN AĞAÇLARDA YAPILAN ÖLÇÜMLER ...................... -

Mersin Province
REPUBLIC OF TURKEY MINISTRY OF FORESTRY AND WATER AFFAIRS (Nature Conservation and National Parks) 7th Regional Directorate - Mersin Branch Office MERSİN PROVINCE MEDITERRANEAN MONK SEAL Monachus monachus SPECIES CONSERVATION ACTION PLAN 2014-2018 DECEMBER 2012 / ANKARA Revision Date: April 2014 REPUBLIC OF TURKEY MINISTRY OF FORESTRY AND WATER AFFAIRS (Nature Conservation and National Parks) 7th Regional Directorate - Mersin Branch Office MERSİN PROVINCE MEDITERRANEAN MONK SEAL / Monachus monachus SPECIES CONSERVATION ACTION PLAN 2014 - 2018 DECEMBER 2012 / ANKARA Revision Date: April 2014 Republic of Turkey Ministry of Forestry and Water Affairs (Nature Conservation Name of Project Owner and National Parks) 7th Regional Directorate - Mersin Branch Office Address Yeni Mah. 33191. Sok. No:31 Mezitli / MERSİN Phone: 0 (324) 3570820 Fax: 0 (324)3570823 Phone and Fax Numbers Preparing Species Conservation Action Plan for Mediterranean Monk Seal (Monachus monachus) and Service Project Name Procurement Work Project Location Mersin Province Turunç Peyzaj Tasarım Planlama Uygulama Proje İnşaat Organizasyon ve Danışmanlık Hizm. Reporting Institution Ltd. Şti. Plan Revision: Mersin Branch Office Address GMK Bulvarı Onur İşhanı 12/143 Kızılay Çankaya/ANKARA Phone and Fax Numbers Phone: 0 (312)4183949 Fax: 0 (312)4183949 Report Submittal Date 26 / 12 / 2012 Plan Revision Date: 16 - 17 April 2014 PREFACE Mediterranean monk seal (Monachus monachus) is a species under conservation by international conventions and national legislations. Various methods are utilized in order to conserve and prevent extinction of Mediterranean monk seal, which is referred to as seal by local people, in many countries. Although it does not have any natural predators on our coasts, Mediterranean monk seal population gradually diminishes due to irresponsible and unplanned human activities.