Osal Fentanyl St Preferred2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

23 July 2021 Page 1 of 11 SATURDAY 17 JULY 2021 Narrator
Radio 4 Extra Listings for 17 – 23 July 2021 Page 1 of 11 SATURDAY 17 JULY 2021 Narrator ...... James Fleet First broadcast on BBC Radio 4 in July 2013. Beryl Bainbridge ...... Samantha Bond SAT 04:30 To the Manor Born (b007k4vh) SAT 00:00 Charles Chilton - Journey into Space (b007jrdj) Author: Brendan King Sons of the Fathers The World in Peril Abridger: Pete Nichols Clearing out the cellar - Audrey finds more than she'd Episode 5 Producer: Karen Rose bargained for. Jet and Lemmy monitor strange calls coming in on the ship-to- A Sweet Talk production for BBC Radio 4, first broadcast in Starring Penelope Keith and Keith Barron. ship intercom. September 2016. Lady of the manor Audrey fforbes-Hamilton, forced to sell her Completing the sci-fi trilogy of the adventures of Captain Jet SAT 02:15 Shardlake (b09l2299) beloved Grantleigh Estate, has decamped to the tiny Old Lodge Morgan, Mitch, Doc and Lemmy. Heartstone cottage with her butler in tow. Jet Morgan …. Andrew Faulds Episode 10 From this vantage point, Audrey keeps a close and disapproving Stephen ‘Mitch’ Mitchell …. Don Sharp Concluding Colin MacDonald's dramatisation of the Tudor eye on new owner, the nouveau-riche Richard DeVere. Doc Matthews …. Guy Kingsley-Poynter mystery novel by C.J. Sansom. Adapted for radio by Peter Spence from his BBC TV script. Lemmy Barnet …. Alfie Bass Matthew Shardlake is on board the Mary Rose when the Audrey fforbes-Hamilton …. Penelope Keith Various …. Alan Tilvern warship is sunk in battle with the loss of more than four Keith Barron ..... Richard DeVere Various and Announcer …. -

Two Weeks of Inspiring Performances, Workshops and More Fresh from the North West See More, Save Money!
TWO WEEKS OF INSPIRING PERFORMANCES, WORKSHOPS AND MORE FRESH FROM THE NORTH WEST SEE MORE, SAVE MONEY! Can’t decide what to see in PUSH? Save money when you book for two or more festival events. Book two or more theatre shows and save £2 per ticket* Book for two or more workshops, events or discussions and save £1 per ticket* Buy a day ticket for Propel on Sat 13 Jan for just £10 (see p7) *All tickets must be purchased at the same time. Excludes works in progress, rehearsed readings, workshops priced at £3 and free events. Terms and conditions apply. 2 Front cover image from The Political History of Smack and Crack FRI 12 - SAT 27 JAN 2018 Welcome to PUSH 2018! PUSH is HOME’s annual celebration of the North West’s most creative talents. Over two weeks our stages, screens and spaces will be dedicated to showcasing fantastic works originating from our region as well as offering opportunities for creatives to meet industry professionals, share ideas and inspiration and develop skills across a broad range of topics. This year, alongside our usual programme of performances, works in progress, screenings, exhibitions and events we are delighted to also present a whole weekend of informative and inspiring workshops and events in conjunction with Random Acts North as well as the premieres of four brand new theatre pieces commissioned by HOME especially for the festival - The Manchester Project (p6); True Stories (p10); Only Speak When Spoken To (p12) and See Me After (p13). We’re looking forward to meeting you at the festival and hope it will provide you with something that fulfils your PUSH 2018 LAUNCH creative thirst! FRI 12 JAN, FROM 18:00 homemcr.org/push-2018 Free #Push2018 Come and celebrate the start of PUSH 2018 with the preview of Jez Dolan’s exhibition Anders Als Die Andern (see p5), followed by celebratory music with a global influence with Manchester International Roots Orchestra from 21:00 (see p6). -
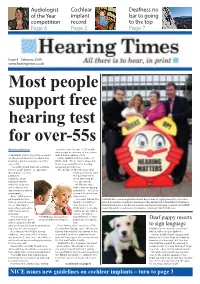
NICE Issues New Guidelines on Cochlear Implants – Turn to Page 3 2 News Hearing Times February 2009
Audiologist Cochlear Deafness no of the Year implant bar to going competition record to the top Page 6 Page 2 Page 7 Issue 4 February 2009 www.hearingtimes.co.uk Most people support free hearing test for over-55s By Gemma Davidson everyone over the age of 55 would give people an average of nine years A LEADING charity is putting pressure with a better quality of life. on the government to introduce free Jackie Ballard, chief executive of hearing tests for everyone over the RNID, said: ‘These figures show that age of 55. there is an appetite for a hearing The RNID (Royal National Institute screening programme. for the Deaf) and the Co-Operative ‘The people of the UK value their Group have recently hearing and they want published the government to research, which show that they do, indicates that the too,’ she added. majority of people Ms Ballard says are in favour of a that – with an ageing nationwide screening population – the UK is programme. facing a ‘hearing loss Over 1,000 people time-bomb’. participated in the The news follows the ALARM CALL: Former England footballer Bryan Robson (right) joined (l-r) actors Alan survey, which showed launch of a partner- Halsall (Coronation Street) and Sue Jenkins (Brookside) and Jackie Ballard of the Royal an overwhelming ship between the National Institute for the Deaf to launch a fundraising campaign on behalf of the RNID percentage agreeing RNID and The Co-Op- to get the public to wake up to hearing loss. See page 3 for the full story. -

7 October 2011 Page 1 of 7 SATURDAY 01 OCTOBER 2011 £2,000,000 Yacht
Radio 4 Extra Listings for 1 – 7 October 2011 Page 1 of 7 SATURDAY 01 OCTOBER 2011 £2,000,000 yacht. SAT 18:00 Terry Pratchett (b00rkm9p) But you can't keep anything quiet with Mum around... Nation SAT 00:00 Arthur C Clarke Stories (b008h36w) Bernard Cribbins and Frank Thornton star in Andrew Palmer’s Episode 8 All the Time in the World sitcom It looks like decision time for Daphne - can she face leaving Professional thief Robert Ashton receives an unexpected visit... Jimmy Bright ...... Bernard Cribbins Mau? South Seas adventure read by Matt Addis and Charlie Time is altered so the world's treasures can be stolen - but who Russell Farrow ...... Frank Thornton Norfolk. is behind it? Nan Forbes ...... Annette Crosbie SAT 18:30 The House on the Borderland by William Hope Arthur C Clarke's 1952 short story read by Nicholas Boulton. Sue Plant ...... Annee Blott Hodgson (b007wxhs) Somerset-born author Arthur C Clarke (1917-2008) achieved Griselda Bright ...... Patricia Hayes 4. The Wound his greatest fame in 1968 when his short story The Sentinel was Written by Andrew Palmer. Back from his voyage, the narrator sees a sinister green hand at turned into the film 2001: A Space Odyssey. His visions of Producer: Edward Taylor his window... space travel and computing sparked the imagination of readers First broadcast on BBC Radio 2 in January 1988. First published in 1908, William Hope Hodgson's fantasy and scientists alike. SAT 05:30 The Little World of Don Camillo (b00tfbf5) novella is now seen as a classic of early, Edwardian sci-fi. -
Two Weeks of Inspiring Performances, Workshops
TWO WEEKS OF INSPIRING PERFORMANCES, WORKSHOPS AND MORE FRESH FROM THE NORTH WEST FRI 12 - SAT 27 JAN 2018 Welcome to PUSH 2018! PUSH is HOME’s annual celebration of the North West’s most creative talents. Over two weeks our stages, screens and spaces will be dedicated to showcasing fantastic works originating from our region as well as offering opportunities for creatives to meet industry professionals, share ideas and inspiration and develop skills across a broad range of topics. This year, alongside our usual programme of performances, works in progress, screenings, exhibitions and events we are delighted to also present a whole weekend of informative and inspiring workshops and events in conjunction with Random Acts North as well as the premieres of four brand new theatre pieces commissioned by HOME especially for the festival - The Manchester Project (p6); True Stories (p10); Only Speak When Spoken To (p12) and See Me After (p13). SEE MORE, SAVE MONEY! We’re looking forward to meeting you at the festival and hope it will provide Can’t decide what to see in PUSH? Save money when you you with something that fulfils your PUSH 2018 LAUNCH creative thirst! book for two or more festival events. FRI 12 JAN, FROM 18:00 Book two or more theatre shows and save £2 per ticket* homemcr.org/push-2018 Free #Push2018 Book for two or more workshops, events or discussions and save £1 per ticket* Come and celebrate the start of PUSH 2018 with the preview of Jez Dolan’s Buy a day ticket for Propel on Sat 13 Jan for just £10 (see p7) exhibition Anders Als Die Andern (see p5), *All tickets must be purchased at the same time. -

Communicating Risk Guidance
COMMUNICATING RISK Managing risk is increasingly central to the business of Government. An essential part of this is risk communication - communication in terms of openness and transparency, understanding and engaging stakeholders, as well as providing balanced information to allow the public make decisions on how to deal with risk. So, if you are; involved in policy planning and development, policy implementation or operational planning, information staff in communications directorates, or involved in providing information to the public, responsible for risk management and business continuity planning, these guidelines are for you. You can access the tool-kit by clicking any of the icons below Introduction Full Contents The Tool-Kit Checklists and Frameworks Annexes Contents Page 1. Introduction - Why this toolkit could be useful to you 4 2. What is risk and why is communication about risk important? 5 2.1 What is risk? 5 2.2 What types of risk do the public face? 5 2.3 Why is good communication important in dealing with risk? 7 2.4 Why has communicating about risk become more important? 8 2.5 What principles does the Government want Departments to adopt? 9 2.6 How can Departments put these principles into practice? 10 3. Understanding how the public reacts to risk 14 3.1 Why is it important to understand how the public views risk? 14 3.2 How do people form judgements about risks? 14 3.3 What factors are likely to increase public concern about risks? 15 3.4 How do attitudes towards risk vary? 16 3.5 What things do people expect from Government when it communicates with them about risk? 17 4. -

WLPCT PT 03 06.Qxd
succ_0306_004.qxd:succ_0206.qxd 22/11/06 16:30 Page 1 A Christie’s Christmas Gift This Christmas, the Christie Hospital has just one wish – s better treatment for people living with cancer. What we want for Christmas is a specialised computer which would mean that people facing cancer get more accurate – and T more effective – radiotherapy treatment in the New Year. More of them will make a full recovery; and we will be able to go on treating patients for years to come. The computer we’re wishing for costs £93,610 and will treat at least 5,000 patients in the next five years. Simply put, the new system will show us the exact size and shape of the tumour, at the time of treatment. That means that we can target the tumour precisely, giving stronger doses of radiation, confident that surrounding healthy tissue won’t be harmed. And those stronger doses will mean that more tumours are totally eradicated, and more people will be cured of cancer. The Christie Hospital has an international reputation for leading the way in cancer treatment and if our Christmas wish comes true, we will be the first hospital in the country to fully implement this life-saving technology. If you would like to make a donation towards our Christimas appeal, contact us on 0161 446 3988 or use the form directly below. Wishing you a very happy Christmas. ¢ WHAT CAN YOU DO? Please help us give more people real hope of surviving cancer by giving what you can. Anything you can give will be very much appreciated. -

Government Communications
HOUSE OF LORDS Select Committee on Communications 1st Report of Session 2008–09 Government Communications Report with Evidence Ordered to be printed 10 December 2008 and published 26 January 2009 Published by the Authority of the House of Lords London : The Stationery Office Limited £price HL Paper 7 The Select Committee on Communications The Select Committee on Communications was appointed by the House of Lords with the orders of reference “to consider communications”. Current Membership Baroness Bonham Carter of Yarnbury Lord Corbett of Castle Vale Baroness Eccles of Moulton Lord Fowler (Chairman) Lord Hastings of Scarisbrick Baroness Howe of Idlicote Lord Inglewood Lord King of Bridgwater Lord Macdonald of Tradeston Baroness McIntosh of Hudnall Bishop of Manchester Lord Maxton Baroness Scott of Needham Market Publications The report and evidence of the Committee are published by The Stationery Office by Order of the House. All publications of the Committee are available on the intranet at: http://www.parliament.uk/parliamentary_committees/communications.cfm General Information General information about the House of Lords and its Committees, including guidance to witnesses, details of current inquiries and forthcoming meetings is on the internet at: http://www.parliament.uk/about_lords/about_lords.cfm Contact details All correspondence should be addressed to the Clerk of the Select Committee on Communications, Committee Office, House of Lords, London SW1A 0PW The telephone number for general enquiries is 020 7219 8662. The Committee’s -

Lstm Annual Report
LSTM ANNUAL REPORT 2019/20 2019/2020 Vision To save lives in resource poor countries through research, education and capacity strengthening Mission To reduce the burden of sickness and mortality in disease endemic countries through the delivery of effective interventions which improve human health and are relevant to the poorest communities Values • Making a difference to health and wellbeing • Excellence in innovation, leadership and science • Achieving and delivering through partnership • An ethical ethos founded on respect, accountability and honesty • Creating a great place to work and study 2 2019/2020 Contents Chair’s Foreword 4 Director’s Foreword 5 Treasurer’s Report 6 LSTM’s response to the COVID-19 pandemic 7 Introduction to the Feature Articles 14 FEATURE ARTICLE: Neglected Tropical Diseases 15 Department of Tropical Disease Biology 19 FEATURE ARTICLE: Malaria and other Vector Borne Diseases 22 Department of Vector Biology 26 FEATURE ARTICLE: Resistance Research and Management 28 Department of Clinical Sciences 30 FEATURE ARTICLE: Lung Health and TB 33 Department of International Public Health 36 FEATURE ARTICLE: HIV 39 Partnerships 41 FEATURE ARTICLE: Maternal, Newborn and Child Health 46 Public Engagement 50 FEATURE ARTICLE: Innovation, Discovery and Development 51 Going Virtual 54 FEATURE ARTICLE: Health Policy and Health Systems Research 56 LSTM’s Top Research Funders 58 Research Governance and Ethics 59 Finance, Procurement and Research Services (FPRS) 60 Education 61 Students & Courses 63 Clinical Diagnostic Parasitology -

South Yorkshire Police 39
Fear and Fashion Awards 2009 Shortlisted entries Project Page No. 198 Contemporary Arts and Learning 2 Avon & Somerset Constabulary and Avon St John Ambulance 5 Dorset Police, Safe Schools & Communities Team 8 Eternal Life Support Centre (ELSC) 10 Football Foundation 13 Lancashire Constabulary 16 Leap Confronting Conflict 19 Liverpool Housing Trust 22 Liverpool Youth Offending Service 25 London Borough of Tower Hamlets, Community Safety Service 28 Reading Youth Offending Service 31 Recre8 34 Redthread Youth Ltd 38 South Yorkshire Police 39 South Yorkshire Police – Firearms Support Group 41 Sowerby Bridge High School 44 1 Organisation: 198 Contemporary Arts and Learning Submitted by: Lucy Davies Project description Please describe this project in one sentence: A peer to peer media campaign produced by young people to promote messages aimed at preventing the use of guns, knives and involvement in gang culture. What was the name of the project? Different Endz. What were the project’s objectives? The project aimed to develop young people’s skills in digital media and give them a platform to voice their ideas and opinions on the issue of gang culture and gun and knife crime. The posters and T Shirts produced by them aimed to relay messages to their peers in the community and they achieved this by distributing products and exhibiting their work publicly. The young people involved were NEET and the creative outcomes of the project were used to help get them into creative courses at college and achieve accreditation through Arts Awards. What were the project activities? 198 worked with Connexions, Lambeth YOS and a pupil referral unit to engage a group of hard to reach and NEET young people. -
Pine Needles
Hid/mk'^ 1 The Woman's College of The University of North Carolina LIBRARY COLLEGE COLLECTION Gift of Senior Class, 1961 Digitized by the Internet Archive in 2010 with funding from University of North Carolina at Chapel Hill http://www.archive.org/details/pineneedlesseria1961nort . IT'S giving us the time to determine our goals in life . _ the directions we take, where we WOMAN'S ffUKLI) pause for emphasis, are mainly individual— sometimes forgotten after approaching suc- cess. We will retain the influence of W.C., but this 1961 Pine Needles records the steps taken toward awareness— of each other and of ourselves. 227435 WOMEN ...And time seeing fully sex. Living and sharing campus-wide bond, belonging and the world . maybe for the first the potentials of our with women, creating a a feeling of loyalty for our school. Woman is woman's natural ally." Living and learning, working and playing—we adventure through every door, to the world belonging to us . ¥tm~M^ WWW ^5 \ w w w V n\ w w w v \ \WWWW? ¥$'*&* w \ ¥&$> \ - . \ www WW ' ' \ \ : \ !y. W " . \ v ^ . \- ^ \ \ WWW \ \ * Happy >^ 'Hi eyes tell the secret the only way it can ever he told ... under the facade created by the practical world a real and vibrant truth exists. We know that we as young students possess the greatest seeds of progress — curiosity, idealism, and hope ... A \ .. 1961 Y. D. C. and Y. R. C. rise to support the election . a toast to Kennedy . South Pacific breaks a leg . new sidewalks and the Thruway". rat day as friendship day...hlue lights for Mclver.. -

Spring & Summer 2008 on ITV1
Spring & Summer 2008 Click below to visit: > Drama > Comedy & Entertainment > Factual > Daytime > Sport > CITV > ITV.com and ITV Mobile Drama Tender Loving Care Pushing Daisies Agatha Christie’s Marple Spring & Summer 2008 Drama new new Tender Loving Care Pushing Daisies A CARNivaL FILM & TELevisiON PRODUctiON A LiviNG Dead GUY AND THE JINKS/COHEN FOR ITV1 COMPANY IN assOciatiON witH WARNER BROS TELevisiON PRODUctiON PAUL NICHOllS, SURAnnE JONES AND SHAUN PARKES staR IN FROM BRYAN FULLER (HeROes) AND BARRY SONNENfeLD (MEN IN BLacK) TENDER LOVING CARE, A CONtemPORARY AND ORIGINAL medicaL COmes PUSHING DAISIES, THE Hit US seRies staRRING LEE PACE AND DRama set IN LONDON’S famOUS medicaL distRict OF HARLEY stReet. AnnA FRIEL abOUT A maN WHO BRINGS THE dead bacK TO Life. With an ethos of providing first-rate, ‘wraparound’ health care, the private Featuring a blend of romance, fantasy and mystery, the Golden Globe- practice is run by three partners, general medical practitioners Robert nominated series is narrated by Jim Dale and follows Ned (Pace), a (Nicholls), Martha (Jones) and Ekkow (Parkes). Each is dynamic and young man with a special gift. As a boy, Ned discovered that he could passionate about delivering the best standards of care, round the clock. briefly resurrect the dead with one touch. But his gift isn’t without deadly consequences, as he soon finds out. Created by Marston Bloom, Tender Loving Care features a world in Press Contact which doctors are with their patients every step of the medical journey The adult, pie-shop owning Ned puts his talent to good use by Press Contact - from lifestyle surgery through everyday care to often life-threatening rejuvenating dead fruit, and at the same time giving it a delicious Tracey Gallagher Ian Johnson / Roxie Maskall conditions.