Palliative Care.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Word Definitions
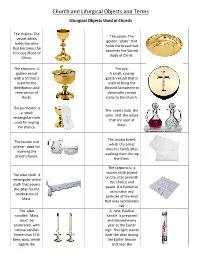
PAGE 1 OF 12 WORD DEFINITIONS The Catholic Words Memory Match Card Game, a fun way for the entire family—or classroom— to learn new Catholic vocabulary words! Instilling a love and reverence for the faith should begin at an early age. This game was borne out of my own desire to do just that for my own children. The Catholic Words Memory Match Card Game will provide parents, grandparents, teachers, homeschoolers, Dan Gonzalez, his wife Elisa and their catechists and youth ministers a fun way to help teach Catholic vocabulary words. two children Matthew and Zoe. A FUN WAY TO LEARN Watch your little one’s excitement at Mass when they recognize the vessels, objects and vestments With these free printable definitions, the game used in the liturgy. Introducing these words will cards become flash cards. help prepare them to receive the Sacraments and Show a card and read its definition. Let the inaugurate a lifelong journey of learning about the child see the picture of the real-world object. wonders of their Catholic faith. Discuss where the object is seen at your local May God bless you and those entrusted to your care. parish or in the home. Take the cards with you to church and point out the items before or after Mass. Then, let the games begin! Catholic Words Memory Match is an addictive way to learn new Catholic vocabulary words! Dan Gonzalez Advent Wreath: A wreath usually made Alb: A white robe with long sleeves worn by the Altar Bells: A bell or set of bells rung of holly or evergreen branches that hold three priest under his chasuble and the deacon under immediately after the consecration of each purple candles and a rose one. -

Pope Addresses Vatican Reforms Aimed at Curbing Corruption, Abuse
Pope addresses Vatican reforms aimed at curbing corruption, abuse VATICAN CITY (CNS) — While financial reforms in the Vatican are progressing steadily, cases involving corruption and malfeasance in the Eternal City are “a disease that we relapse into,” Pope Francis said. In a wide-ranging interview broadcast Sept. 1 by COPE, the Spanish radio station owned by the Spanish bishops’ conference, Pope Francis said changes made in the Vatican’s financial laws have allowed prosecutors to “become more independent” in their investigations. “Let’s hope that these steps we are taking … will help to make these events happen less and less,” he said. During the interview, the pope was asked about the Vatican trial against 10 individuals and entities, including Cardinal Angelo Becciu, former prefect of the Congregation for Saints’ Causes, on charges ranging from embezzlement to money laundering and abuse of office. The charges stemmed from a Vatican investigation into how the Secretariat of State used $200 million to finance a property development project in London’s posh Chelsea district and incurred millions of dollars in debt. At the time, then- Archbishop Becciu served as “sostituto,” the No. 3 position in the Vatican Secretariat of State. Cardinal Becciu was forced to offer his resignation to the pope in September 2020, after he was accused of embezzling an estimated 100,000 euros of Vatican funds and redirecting them to Spes, a Caritas organization run by his brother, Tonino Becciu, in his home Diocese of Ozieri, Sardinia. The pope told COPE he authorized the Vatican’s investigation into the property deal as a sign that he was “not afraid of transparency or the truth.” “Sometimes it hurts a lot, but the truth is what sets us free,” he said. -
Church and Liturgical Objects and Terms
Church and Liturgical Objects and Terms Liturgical Objects Used in Church The chalice: The The paten: The vessel which golden “plate” that holds the wine holds the bread that that becomes the becomes the Sacred Precious Blood of Body of Christ. Christ. The ciborium: A The pyx: golden vessel A small, closing with a lid that is golden vessel that is used for the used to bring the distribution and Blessed Sacrament to reservation of those who cannot Hosts. come to the church. The purificator is The cruets hold the a small wine and the water rectangular cloth that are used at used for wiping Mass. the chalice. The lavabo towel, The lavabo and which the priest pitcher: used for dries his hands after washing the washing them during priest's hands. the Mass. The corporal is a square cloth placed The altar cloth: A on the altar beneath rectangular white the chalice and cloth that covers paten. It is folded so the altar for the as to catch any celebration of particles of the Host Mass. that may accidentally fall The altar A new Paschal candles: Mass candle is prepared must be and blessed every celebrated with year at the Easter natural candles Vigil. This light stands (more than 51% near the altar during bees wax), which the Easter Season signify the and near the presence of baptismal font Christ, our light. during the rest of the year. It may also stand near the casket during the funeral rites. The sanctuary lamp: Bells, rung during A candle, often red, the calling down that burns near the of the Holy Spirit tabernacle when the to consecrate the Blessed Sacrament is bread and wine present there. -
Great Cloud of Witnesses.Indd
A Great Cloud of Witnesses i ii A Great Cloud of Witnesses A Calendar of Commemorations iii Copyright © 2016 by The Domestic and Foreign Missionary Society of The Protestant Episcopal Church in the United States of America Portions of this book may be reproduced by a congregation for its own use. Commercial or large-scale reproduction for sale of any portion of this book or of the book as a whole, without the written permission of Church Publishing Incorporated, is prohibited. Cover design and typesetting by Linda Brooks ISBN-13: 978-0-89869-962-3 (binder) ISBN-13: 978-0-89869-966-1 (pbk.) ISBN-13: 978-0-89869-963-0 (ebook) Church Publishing, Incorporated. 19 East 34th Street New York, New York 10016 www.churchpublishing.org iv Contents Introduction vii On Commemorations and the Book of Common Prayer viii On the Making of Saints x How to Use These Materials xiii Commemorations Calendar of Commemorations Commemorations Appendix a1 Commons of Saints and Propers for Various Occasions a5 Commons of Saints a7 Various Occasions from the Book of Common Prayer a37 New Propers for Various Occasions a63 Guidelines for Continuing Alteration of the Calendar a71 Criteria for Additions to A Great Cloud of Witnesses a73 Procedures for Local Calendars and Memorials a75 Procedures for Churchwide Recognition a76 Procedures to Remove Commemorations a77 v vi Introduction This volume, A Great Cloud of Witnesses, is a further step in the development of liturgical commemorations within the life of The Episcopal Church. These developments fall under three categories. First, this volume presents a wide array of possible commemorations for individuals and congregations to observe. -

Deconsecration Rites of Roman Catholic Church Buildings
religions Article Ritual Void or Ritual Muddle? Deconsecration Rites of Roman Catholic Church Buildings Kim de Wildt Transformation of Sacred Space: Function and Use of Religious Places in Germany (FOR 2733), University of Bonn, 53113 Bonn, Germany; [email protected] Received: 29 August 2020; Accepted: 6 October 2020; Published: 10 October 2020 Abstract: The decrease in people who regularly celebrate liturgy in western Europe has led to the question of what to do with so-called obsolete church buildings. This question not only refers to whether or not a church building will be converted, reused or demolished, but also to the question of whether or not such a building needs to be deconsecrated, and if so, what does deconsecration of a church building actually entail? In this contribution, I will consider the role deconsecration rites play in the Roman Catholic church when a church building is taken out of liturgical use. In Roman Catholic liturgy, there are no prescribed, official deconsecration rites that are mandatory for a church building that is to be taken out of liturgical use. The actual deconsecration of a church building is, according to canon law, established by a decree that is issued by the responsible diocesan bishop. In the case of a church being taken out of liturgical use, however, there seems to be a shift from having a ritual void with regard to deconsecration rites, and also a focus on the “legitimate” way (in the sense of canon law) to deconsecrate a church building (object orientation), towards, in recent decades, paying more attention to a growing pastoral need (subject orientation) for deconsecration rites. -
Ten Strategies of a World-Class Cybersecurity Operations Center Conveys MITRE’S Expertise on Accumulated Expertise on Enterprise-Grade Computer Network Defense
Bleed rule--remove from file Bleed rule--remove from file MITRE’s accumulated Ten Strategies of a World-Class Cybersecurity Operations Center conveys MITRE’s expertise on accumulated expertise on enterprise-grade computer network defense. It covers ten key qualities enterprise- grade of leading Cybersecurity Operations Centers (CSOCs), ranging from their structure and organization, computer MITRE network to processes that best enable effective and efficient operations, to approaches that extract maximum defense Ten Strategies of a World-Class value from CSOC technology investments. This book offers perspective and context for key decision Cybersecurity Operations Center points in structuring a CSOC and shows how to: • Find the right size and structure for the CSOC team Cybersecurity Operations Center a World-Class of Strategies Ten The MITRE Corporation is • Achieve effective placement within a larger organization that a not-for-profit organization enables CSOC operations that operates federally funded • Attract, retain, and grow the right staff and skills research and development • Prepare the CSOC team, technologies, and processes for agile, centers (FFRDCs). FFRDCs threat-based response are unique organizations that • Architect for large-scale data collection and analysis with a assist the U.S. government with limited budget scientific research and analysis, • Prioritize sensor placement and data feed choices across development and acquisition, enteprise systems, enclaves, networks, and perimeters and systems engineering and integration. We’re proud to have If you manage, work in, or are standing up a CSOC, this book is for you. served the public interest for It is also available on MITRE’s website, www.mitre.org. more than 50 years. -

Durham Research Online
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Durham Research Online Durham Research Online Deposited in DRO: 23 June 2020 Version of attached le: Accepted Version Peer-review status of attached le: Peer-reviewed Citation for published item: Brooks, Mary M. and O'Connor, Sonia and Caple, Christopher and Graves, C. Pamela and Quye, Anita (2020) 'Fragments of Faith : unpicking Archbishop John Morton's vestments.', Antiquaries journal. Further information on publisher's website: https://doi.org/10.1017/S000358152000027X Publisher's copyright statement: This article has been published in a revised form in the Antiquaries journal. https://doi.org/10.1017/S000358152000027X. This version is published under a Creative Commons CC-BY-NC-ND. No commercial re-distribution or re-use allowed. Derivative works cannot be distributed. c The Society of Antiquaries of London 2020. Additional information: Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in DRO • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. Please consult the full DRO policy for further details. Durham University Library, Stockton Road, Durham DH1 3LY, United Kingdom Tel : +44 (0)191 334 3042 | Fax : +44 (0)191 334 2971 http://dro.dur.ac.uk FRAGMENTS OF FAITH: UNPICKING ARCHBISHOP JOHN MORTON’S VESTMENTS Mary M Brooks FSA (London) and Sonia O’Connor FSA (London) with contributions from Christopher Caple FSA (London), C. -

The Cardinal's Wardrobe
Chapter 32 The Cardinal’s Wardrobe Carol M. Richardson By the end of the 17th century, the papal master of ceremonies, Francesco Sestini da Bibbiena, could report that cardinals’ dress consisted of the sou- tane (a long, sleeved cassock, buttoned down the front), rochet (a linen over- garment or surplice), manteletta (short shoulder cape worn only in Rome), mozzetta (short cape usually buttoned in front) and cappa magna (voluminous cloak with a hood). The hat was always red, whereas the cassock and cloak could be in one of three qualities of the colour: pavonazzo (peacock-coloured), rosso (red) or rose secche (old rose), depending on the occasion.1 Although red is the colour worn by cardinals, it is not the cardinals’ colour but the popes’. The colour is significant precisely because it binds the pope and his cardinals, as head and members of the papal body: “in capite et in mem- bris” (see also Barbara Bombi’s chapter in this volume).2 William Durandus explained in his Rationale of 1286: the Sovereign Pontiff always appears dressed with a red cape on the out- side while underneath it he is dressed with white vestments; for within, he ought to shine through innocence and charity; and on the outside, he ought to be red through compassion, so that he might show himself to be always ready to lay down his life for his sheep; for he stands in the place of Him who made red His garments for all the sheep in the world.3 Papal garb seems to have been established relatively early on, though its first formal record is in the late 13th-century ordo, or ceremonial book, of Gregory x.4 How the cardinals’ costume evolved was a long, often contentious process, that 1 Francesco Sestini, Il moderno maestro di camera (Rome: 1697), 9–10. -

Selected Works of Joseph Cardinal Bernardin
Selected Works of Joseph Cardinal Bernardin VOLUME 2 Church and Society Alphonse P. Spilly, C.PP.S. Editor A Liturgical Press Book THE LITURGICAL PRESS i)_~ Collegeville, Minnesota Cover design by Ann Blattner Excerpts are taken From the New American Bible, © 1970 by the Confraternity of Christian Doctrine, 3211 Fourth Street N,E,, Washington, DC. 20017—1194, reserved. and are used by permission of the copyright holder. All rights and Post Conciliar Excerpts are also quoted from Vatican Council II: The Conciliar Documents, © 1975 and 1986 by Harry J. Costello and Reverend Austin Flannery, O.P., Costello Publishing Co., PO. Box 9, Northport, NY 11768, USA. © 2000 by the Archdiocese of Chicago, Chicago, Illinois. All rights reserved. No electronic or part of this work may be reproduced in any form or by any means, mechanical, including photocopying, recording, taping, or any retrieval system, without the written permission of The Liturgical Press, Collegeville, MN 56321. Printed in the United States of America. Volume 2: ISBN 0-8146—2584-3 1 2 3 4 S 6 7 8 Library of Congress Cataloging-in-Publication Data Bernardin, Joseph Louis, 1928~ [Selections 2000] Selected works of Joseph Cardinal Bernardin / Alphonse P. Spilly, editor ; foreword by Roger Cardinal Mahony. p cm, Includes bibliographical references and index, Contents: v 1‘ Homilies and teaching documents, ISBN 0-8146-2583-5 (alk. paper) 1. Catholic Church—Doctrines. I. Spilly, Alphonse P, 19397 . 11, Title. BX47OS.838125 A25 2000 282K77311~dc21 99-039499 CIP Address “Catholic Identity: Resolving Conflicting Expectations”* Fordham University, New York, New York _ April 20, 1991 It is good to be back at Fordham University which provided a forum in 1983 for my first in a series of addresses on the need for a consistent ethic of life. -

Guidelines for Eucharistic Processions
Guidelines for Eucharistic Processions Pope Paul VI writes of special forms of worship of the Eucharist, “The Catholic Church has always displayed and still displays this latria that ought to be paid to the Sacrament of the Eucharist, both during Mass and outside of it, by taking the greatest possible care of consecrated hosts, by exposing them to the solemn veneration of the faithful, and by carrying them about in processions to the joy of great numbers of the people.”1 May our processions also bring joy to all who participate! This is not an unfounded joy, but one founded on the knowledge that Christ comes to us, to be among us, to make is dwelling in our midst, to teach us, and lead us to the Father. The following are helpful guidelines for preparing a Eucharistic Procession according to the norms of the Church. 1. The source texts for Eucharistic Processions is Holy Communion and Worship of the Eucharist Outside Mass (HCWEOM), #’s 101-108 and Ceremonial of Bishops #’s 385-394. 2. The following are the things that should be prepared for the procession in addition to what is needed for the Mass: a. A host to be used in the monstrance b. Monstrance c. Humeral Veil d. [Second Thurible] e. Candles for the procession f. [Canopy] 3. A day of especial importance for Eucharistic devotion, and thus also for processions, is the Feast of Corpus Christi. While processions may be done on other days, it is for the local ordinary to determine these other times (cf. HCWEOM 101-102) 4. -

Saint John the Apostle Catholic Parish and School Altar Server Handbook
Saint John the Apostle Catholic Parish and School Altar Server Handbook February 2017 Table of Contents Chapter 1 – What is an Altar Server Page 3 Chapter 2 – Server Duties Page 5 Chapter 3 – The Mass Page 7 Chapter 4 – Baptism within the Mass Page 13 Chapter 5 – Nuptial Mass (Weddings) Page 14 Chapter 6 – Funeral Mass Page 15 Chapter 7 – Benediction Page 19 Chapter 8 – Stations of the Cross Page 20 Chapter 9 – Incense feasts Page 21 Chapter 10 – Miter and Crozier Page 22 Chapter 11 – Church Articles Page 24 2 Chapter 1 What is an Altar Server? An altar server is a lay assistant to a member of the clergy during a religious service. An altar server attends to supporting tasks at the altar such as fetching and carrying, ringing bells, setting up, cleaning up, and so on. Until 1983, only young men whom the Church sometimes hoped to recruit for the priesthood and seminarians could serve at the altar, and thus altar boy was the usual term until Canon 230 was changed in the 1983 update to the Code of Canon which provided the option for local ordinaries (bishops) to permit females to serve at the altar. The term altar server is now widely used and accepted. When altar servers were only young men and seminarians the term acolyte was used. An acolyte is one of the instituted orders which is installed by a bishop. The title of acolyte is still only given to men as it is historically a minor order of ordained ministry. This term is now usually reserved for the ministry that all who are to be promoted to the diaconate receives at least six months before being ordained a deacon (c. -

Pope Creates 22 New Cardinals, Including Three from US, Canada
50¢ February 26, 2012 Volume 86, No. 8 GO DIGITAL todayscatholicnews.org todayscatholicnews.org Serving the Diocese of Fort Wayne-South Bend CLICK ON CIRCULATION ’’ No time TTODAYODAYSS CCATHOLICATHOLIC for retirement Retirement ‘far and away’ from boring Pope creates 22 new cardinals, Pages 9-13 including three from US, Canada ‘Ad limina’ visit highlights BY CINDY WOODEN In Truth and Charity VATICAN CITY (CNS) — Pope Benedict XVI cre- ated 22 new cardinals from 13 countries — including Page 2 three from the United States and Canada — placing red hats on their heads and calling them to lives of even greater love and service to the Church. The churchmen who joined the College of Cardinals Feb. 18 included Cardinals Timothy M. More HHS Dolan of New York; Edwin F. O’Brien, grand master mandate reaction of the Equestrian Order of the Holy Sepulcher of Jerusalem and former archbishop of Baltimore; and In defense of religious liberties Thomas C. Collins of Toronto. In their first official act in their new role, the Pages 3-4 new cardinals were asked to join their peers in giv- ing the pope their opinion, in writing, on the can- onization of seven new saints, including Blessed Kateri Tekakwitha, an American Indian, and Blessed Scouts honor Marianne Cope of Molokai, Hawaii. The pope announced at the consistory that the chaplain canonization ceremony would be celebrated Oct. 21 at the Vatican. Father Steinacker receives Cardinal Collins said, “I am delighted that my first action as a cardinal was to join with the College of St. George Award Cardinals in affirming the canonization of Blessed Page 7 Kateri Tekakwitha, who has been such an inspiration for the people of our First Nations and so many others in Canada and the United States.” Cardinal Dolan also mentioned the consultation on CNS PHOTO/PAUL HARING the canonization of Blessed Kateri, who was born in Pope Benedict embraces Cardinal Timothy M.