Nutrition Survey Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aden History
10/14/2016 Aden History ﺃﺳﺭﺓ ﺍﻟﺗﺣﺭﻳﺭ Editors: ﺍﻟﺩﻛﺗﻭﺭ ﻋﺑﺩﷲ ﺍﻟﺳﻳﺎﺭﻱ Dr. A. Al Sayyari (Saudi Arabia) Dr. Shihab Ghanem ﺍﻟﺩﻛﺗﻭﺭ ﺷﻬﺎﺏ ﻏﺎﻧﻡ (UAE) ﺃﻻﻣﺎﺭﺍﺕ ﺍﻟﻣﺗﺣﺩﺓ) Dhow symbol which Ashraf Girgrah was incorporated (Canada) ﺃﺷﺭﻑ ﺟﺭﺟﺭﻩ into the Union Jack to form Aden Colony flag. Design : Ashraf Girgrah ﺃﺷﺭﻑ ﺟﺭﺟﺭﻩ ﺍﻟﺗﺣﺩﻳﺙ ﺍﻻﺧﻳﺭ ﻓﻲ Last update Oct. 2016 Search Query ﻋﻧﻭﺍﻥ ﺍﻻﺗﺻﺎﻝ Contact address: [email protected] Search European Time A short history of Aden Colony 18391967 The first European to give a first hand description on Aden at the beginning of the 16th century, was the Italian Ludovico di Varthema. He writes: "Aden is such mighty and powerful that I have hardly seen another city of its might during my life . all big ships anchor at the port coming from India Ethiopia or Sira Isalnd harbour in 1512. Persia".(1) www.philipsharpegallery.com Copper line engraving showing the earliest view of Aden first published by Braun and Hogenberg in Cologne 1572. An ancient trade center, the city of Aden was under Egyptian control British Navy squadron from the 3rd century BC until it became a Roman colony in 24 BC. It invading Aden in 1839. fell successively under Ethiopian and Persian control and became associated with Yemen about the 7th century AD. It fell to the Turks in Captain Haines, first 1538 and was incorporated into the Sultanate of Lahej in 1728. Under British Agent the rule of the Sultan of Lahej, Aden had declined to a small fishing appointee after invading village with only 600 inhabitants.(2) Aden on January In 1838, Sultan Muhsin bin Fadl ceded 75 square miles 194 (sq. -
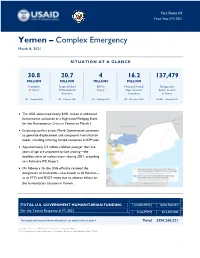
2021 03 08 USG Yemen Complex Emergency Fact Sheet #2
Fact Sheet #2 Fiscal Year (FY) 2021 Yemen – Complex Emergency March 8, 2021 SITUATION AT A GLANCE 30.8 20.7 4 16.2 137,479 MILLION MILLION MILLION MILLION Population People in Need IDPs in Projected Acutely Refugees and of Yemen of Humanitarian Yemen Food- Insecure Asylum Seekers Assistance Population in Yemen UN – February 2021 UN – February 2021 UN – February 2021 IPC – December 2020 UNHCR – February 2021 The USG announced nearly $191 million in additional humanitarian assistance at a High-Level Pledging Event for the Humanitarian Crisis in Yemen on March 1. Escalating conflict across Marib Governorate continues to generate displacement and compound humanitarian needs, including straining limited resources at IDP sites. Approximately 2.3 million children younger than five years of age are projected to face wasting—the deadliest form of malnutrition—during 2021, according to a February IPC Report. On February 16, the USG officially revoked the designation of Ansarallah—also known as Al Houthis— as an FTO and SDGT entity due to adverse effects on the humanitarian situation in Yemen. TOTAL U.S. GOVERNMENT HUMANITARIAN FUNDING USAID/BHA1 $336,760,221 For the Yemen Response in FY 2021 2 State/PRM $13,500,000 For complete funding breakdown with partners, see detailed chart on page 6 Total $350,260,221 1 USAID’s Bureau for Humanitarian Assistance (USAID/BHA). 2 U.S. Department of State’s Bureau of Population, Refugees, and Migration (State/PRM). 1 KEY DEVELOPMENTS USG Announces $191 Million at Humanitarian Pledging Conference The UN Office for the Coordination of Humanitarian Affairs (OCHA) and the governments of Sweden and Switzerland virtually hosted a High-Level Pledging Event for the Humanitarian Crisis in Yemen on March 1. -

Delineating and Calculating the Length of Yemen's Mainland
International Journal of Alternative Fuels and Energy Research Article 2021 │Volume 5│Issue 1│1-9 Open Access Delineating and Calculating the Length of Article Information Yemen's Mainland Shoreline Received: February 20, 2021 * Accepted: March 29, 2021 Hisham M. H. Nagi Published: April 30, 2021 Department Environmental Sciences, Faculty of Petroleum and Natural Resources, Sana'a Keywords University, Sana’a, Yemen. Shoreline, Coast of Yemen, Abstract: Red Sea, Gulf of Aden, The Republic of Yemen is one of the countries gifted with a long coastal line. The Arabian Sea, coastal zone is rich with biodiversity and a wide range of coastal ecosystems, which GIS. is vital to the livelihood of the coastal communities. Despite the fact that several Authors’ Contribution studies have described its coastal characteristics, there are still obvious variations in HMHN designed and performed the experiments. HMHN wrote and stating the actual length of its shoreline. In many reports and research studies, the revised the paper. coastline length of Yemen's mainland has been reported with different figures such How to cite as 1,906, 2,000, 2,100, 2,200 2,300, 2,350, and 2,520 km. This research paper aims Nagi, H.M.H., 2021. Delineating to substantiate the actual shoreline length of Yemen, in addition, to calculate the and Calculating the Length of length of each coastal governorate and district using GIS tools. This study showed Yemen's Mainland Shoreline. Int. J. Altern. Fuels. Energy., 5(1): 1-9. that the total length of Yemen's mainland shoreline is about 2,252 km, with approximately 770 km overlooks the Red Sea and 1,482 km of the southern *Correspondence Hisham M. -

Yemen Country Office
Yemen Country Office Humanitarian Situation Report ©UNICEF Yemen/2020 Reporting Period: 1 – 28 February 2021 Situation in Numbers (OCHA, 2021 Humanitarian Needs Overview) Highlights • February witnessed a spike in the intensity of conflict on the Marib front 11.3 million despite ongoing peace talks and cessation of hostilities amongst conflicted children in need of parties in the country. Thousands fled conflict-affected parts of north-western humanitarian assistance Al Jawf, and southwestern and north-eastern Marib. The deteriorating security situation in these areas is leading to mass displacement and exacerbating 20.7 million already widespread needs. people in need • A total of 190,858 children over one year old were vaccinated against cholera (94 per cent coverage); among them, 188,850 received the second dose and 1.58 million 2,008 were reached with the first dose of the Oral Cholera Vaccine (OCV). children internally displaced • The Risk Communication and Community Engagement (RCCE) assessment on (IDPs) COVID-19 was conducted in three districts in Aden to assess knowledge and risk perception of the project beneficiaries, as well as to identify information needs and effective communication channels for engaging them. These findings will guide the COVID RCCE for shielding messaging and interventions in the targeted districts. UNICEF Appeal 2021 UNICEF’s Response and Funding Status1 $576.9 M Measles vaccination 3% Health Funding status 6% Humanitarian funds Other resources SAM admissions 6% $11.5M $44.5M Funding status Nutrition 13% MHPSS access 6% Child Funding status 16% Protection Education access 2% Carry-forward Funding status 42% $94.5M Education Safe water access 24% WASH Funding status 22% Funding gap HH with cash transfer 0% $426.4M Cash Funding status Transfer 28% Behavior change 8% C4D Funding status 51% RRM Kits 8% RRM Funding status 51% 0% 20% 40% 60% 80% 100% 1 Please refer to the narrative for details. -

Chapter 3 Implementation Plan Chapter 3 Implementation Plan
CHAPTER 3 IMPLEMENTATION PLAN CHAPTER 3 IMPLEMENTATION PLAN 3-1 Implementation Plan 3-1-1 Concept for Implementation The Project will be implemented in accordance with the framework of the grant aid scheme of the Government of Japan after the conclusion of the Exchange of Notes (E/N) by both Governments of Japan and Yemen following a cabinet decision on the implementation of the Project by the Government of Japan. The Government of Yemen will then select a Japanese consultant firm as the Consultant for the Project to proceed with the detailed design work on the facilities and equipment. Following finalization of the detailed design documents, a Japanese construction company and a Japanese equipment supplier, selected on a tender basis respectively, will conduct the construction work and the equipment supply and installation. All of the consultancy, construction and equipment supply / installation contracts will become valid once they have been verified by the Government of Japan. The work management system will be established by the Project Implementation Body, the Consultant, the Contractor and the Equipment Supplier under the control of the related organizations of the two governments involved. The basic issues and points to note for the implementation of the Project are described below. (1) Project Implementation Body The responsible agency for the Project on the Yemeni side is the Ministry of Public Health (MOPH) which is expected to sign the contract on behalf of the Government of Yemen. Meanwhile, the Health Office of the Aden Governorate will act as the implementation agency and will be responsible for the general coordination of the work during the project implementation period. -

Yemen Humanitarian Situation Report May 2019
UNICEF YEMEN HUMANITARIAN SITUATION REPORT MAY 2019 - Yemen Humanitarian Situation Report marginalized community during a cholera prevention session conducted femaleby religious leaders in in Al Hasabah district, Sana’a.in ©UNICEF Yemen/2019/Mona Adel. childA from a Highlights May 2019 • On 16 May, multiple air strikes hit various locations in Amanat Al Asimah and Sana’a 12.3 million governorates, killing children and wounding more than 70 civilians. Seven children # of children in need of humanitarian between the ages of 4 and 14 were also killed on 24 May in an attack on the Mawiyah assistance (estimated) district, in the southern Yemeni city of Taiz. This attack increased the verified number 24.1 million # of people in need of children killed and injured the escalation of violence near Sanaa and in Taiz to 27 in (OCHA, 2019 Yemen Humanitarian Needs only 10 days, but the actual numbers are likely to be much higher. Overview) • The number of Acute Watery Diarrhoea/suspected cholera cases has continued to rise 1.71 million since the start of 2019, with 312 out of 333 districts reporting suspected cases this year # of children internally displaced (IDPs) so far. Since 1 January 2019 to 31 May 2019, there have been 365,223 suspected cases 4.7 million and 638 associated deaths recorded (CFR 0.20 per cent). Children under five represent # of children in need of educational assistance 360,000 a quarter of the total suspected cases. # of children under 5 suffering Severe Acute • UNICEF continues to assess and monitor the nutrition situation in Yemen. -

Yemen Country Office
Yemen Country Office Humanitarian Situation Report ©UNICEF Yemen/2020 Reporting Period: 1 – 31 March 2021 © UNICEF/2021/Yemen Situation in Numbers (OCHA, 2021 Humanitarian Needs Overview) Highlights 11.3 million • The humanitarian situation in Ma’rib continued to be of concern, and with various children in need of waves of violence during the reporting period, the situation showed no signs of humanitarian assistance improvement. People’s lives remained to be impacted every day by fighting, and thousands were being displaced from their homes and displacement sites. Conflict continued as well as in Al Hodeidah, Taizz, and Al Jawf. 20.7 million • In March, 30,317 IDPs were displaced, with the majority of displacement waves people in need coming from Ma’rib, Al Hodeidah, Taizz and Al-Jawf, as internal displacement within governorates towards safer districts increased. • The Rapid Response Mechanism (RRM) reached an additional 3,500 newly displaced 1.58 million families, 2,200 families of which were in Ma’rib (24,500 individuals). Beneficiaries children internally displaced received RRM kits that included food, family basic hygiene kits, and female dignity kits. (IDPs) • As of 5 April 2021, there were 4,798 COVID-19 officially confirmed cases in Yemen, with 946 associated deaths and 1,738 recovered cases (resulting in a 19.7 per cent confirmed fatality rate). 382 suspected cases were health workers, or 4.78 per cent of the total cases. Funding Status UNICEF’s Response and Funding Status 2021 Appeal: $576.9M SAM Admission 15% n Funding status -

Escalating Conflict Flash Update 14 | 20 April 2015 (10.00)
Yemen: Escalating Conflict Flash Update 14 | 20 April 2015 (10.00) Daily Key messages Parties to the conflict have an obligation to protect civilians and civilian infrastructure. Reports of civilian casualties due to ongoing conflict are unacceptable. Overview Yemeni authorities report that at least 30 people have been killed and up to 300 injured in Sana’a City after an airstrike set off a huge explosion in Faj Attan suburb earlier today. The airstrike may have targeted a munitions depot in the area. Nearby homes were damaged, trapping people in rubble. Ambulances took the wounded to hospital. Parties to the conflict have an obligation, under international humanitarian law, to protect civilians and civilian infrastructure. In the last 24 hours, airstrikes have hit targets in Aden, Lahj, Sana’a, Sa’ada and Marib governorates. In Sirwak district, Marib governorate, an airstrike hit a health facility in Al Juhlan area. This was the only medical facility in the area. In Sahar district, Sa'ada governorate, one civilian was reportedly killed and seven others injured in an airstrike on a petrol station.. In Amran governorate, the districts of Huth and Khamir were hit, with casualties reported. In Aden, armed clashes and mortar shelling continues amid clashes between militants in Khormakser, Crater, Al Mualla, Al Qalowa, Dar Sad and Ash Sheikh Othman districts. The security situation remains very tense. Today, clashes intensified for hours in the vicinity of President Hadi's residence and the Russian consulate. In Lahj governorate, militants continued their advance towards Aden governorate. Armed clashes were also reported in Al Dhale’e governorate. -

Growth and Malnutrition Among Preschool Children in Democratic Yemen G
Bulletin of the World Health Organization, 66 (4): 491-498 (1988) © World Health Organization 1988 Growth and malnutrition among preschool children in Democratic Yemen G. BAGENHOLM,1 B. KRISTIANSSON,1 & A. A. A. NASHER2 A cross-sectional anthropometric study ofchildren aged 0-84 months was performed in 1982-83 in Democratic Yemen. The total sample included 3407 children, representing populations from urban, rural, and slum areas ofthe country. NCHS/WHO growth data were usedfor reference purposes. A high overall prevalence ofwasting (8. 7%) and stunting (35.2%) was found among the children. However, rural children exhibited a satisfactory weight-for-height during the first 6 months of life compared with both the reference and the urban and slum children. Slum children had a high prevalence of wasting during the first 18 months of life. For the younger age groups, rural children were shorter than urban children, but at 7years ofage all the children were similar, with a mean height-for-age corresponding to -1. 7 standard deviations ofthatfor the reference population. Mothers in the urban area weighed significantly more than those from the slum or rural areas (P <0.001), but all mothers had similar heights. Only a few studies have assessed growth and mal- years were eligible for inclusion in the study, and nutrition among children in Democratic Yemen. Table 1 contains demographic data on those sampled. Among these, a hospital-based study performed in Urban, rural, and slum populations were studied and 1976 showed an incidence of severe malnutrition the selection procedures outlined below were used. (cut-off level not defined) corresponding to 7 % of all children admitted (1). -

IOM Yemen Crisis Situation Report #33, 19 November 2015
INTERNATIONAL ORGANIZATION FOR MIGRATION SITUATION REPORT 19 November 2015 Migrants provided with psychosocial support by IOM’s Health Unit psychologist, Al Hudaydah. Highlights © IOM 2015 (Photo: IOM Yemen) As part of the Task Force for Population Since the beginning of the crisis, IOM As of 18 November, over 70,000 Movement, IOM was able to identify over has provided over 12,200 individuals with people have arrived in Djibouti, Somalia, 5,900 IDP households displaced by onward transportation assistance from Ethiopia and Sudan from Yemen. Close to Cyclones Chapala and Megh across 13 Djibouti and Somalia to their areas of 23,000 individuals have received post- districts in six governorates through the origin. arrival assistance from IOM. Displacement Tracking Matrix. Situation Overview Fighting continues with recent reports from Human Rights Watch identifying the use of banned landmines by Houthi forces in the of Abyan, Aden, Marib, Lahj, and Taizz governorates in recent months. In addition, heavy fighting continues particularly in AlDhale’e and Taizz governorates. The humanitarian community continues to provide assistance to those who were directly affected by the Tropical Cyclones Chapala and Megh earlier this month which brought an unprecedented amount of rainfall into the region. A preliminary assessment by the Task Force for Population Movement, estimates around 47,000 people have been displaced in Abyan, Hadramaut, Shabwah, and Socotra governorates. Essential infrastructure, including roads and telecommunication networks, were severely damaged. Priority needs include food, fuel, NFIs, tents and medical supplies (source: OCHA, 16 November). Ten trucks sent by IOM, UNHCR and UNICEF, transporting over 33 metric tons (MT) of Non-Food Items from Aden, have arrived in Al Mukalla. -

Humanitarian Update
HUMANITARIAN UPDATE Issue 07 / July 2020 Distribution of commodity vouchers in Ammar bin Yaser School in Amant Al Asimah, Sana’a, April 2020. ©WFP/Mohammed Awadh New food security analysis HIGHLIGHTS forecasts an alarming increase in Funding shortage closes the number of people facing high life-saving programmes as humanitarian needs rise levels of acute food insecurity by P 02 end of 2020 COVID-19 strategy refreshed A new Integrated Phase Classification Grande, Humanitarian Coordinator as COVID-19 continues to (IPC) analysis released by the World for Yemen. “Eighteen months ago, spread across Yemen Food Program (WFP), the UN when we faced a similar situation, P 04 Children’s Fund (UNICEF) and the we were generously funded. We Food and Agriculture Organization used the resources we were entrusted Fuel crisis is another shock (FAO) on 22 July, warns that with wisely and massively scaled- to the humanitarian situation economic shocks, conflict, floods, up assistance in the districts where in northern governorates locusts and COVID-19 could reverse people were the hungriest and most P 05 food security gains in Yemen. The at risk. The result was tremendous. report, which analyzes the situation We prevented famine. Unless we Hopes of a UN assessment of 7.9 million people in 133 districts receive the funding we need now, mission to avert a in southern governorates, forecasts we won’t be able to do the same this catastrophic oil spill from an alarming increase in the number time.” the Safer tanker falter of people facing high levels of acute Food insecurity is high in areas food insecurity (IPC Phase 3 and IPC P 07 characterized by fighting, which Phase 4), from 2 million (25 per cent leads to access restrictions for of the population) to 3.2 million (40 Air strikes causing civilian humanitarian food assistance and per cent of the population) in the next casualties double in the to markets, and causes constant six months, even if existing levels of second quarter of 2020 population displacements. -

UNHCR Operational Update in Yemen
UNHCR OPERATIONAL UPDATE YEMEN 20 February 2020 IDP Response During the reporting period, UNHCR and partners provided assistance to a total Key figures: of 756 families in Amanat Al-Asimah, Sana’a, Dhamar and Al Bayda governorates. Some 140 internally displaced persons (IDPs) with mental health and psychosocial 24.1 M needs received support at community centres managed by UNHCR partners, while people in need some 200 individuals attended awareness sessions on children’s rights and registration support conducted by a legal counsellor. Additionally, 164 families (1,027 individuals) affected by the conflict received household items such as blankets, mattresses and other 3.65 M displaced emergency shelter materials to address their immediate needs. 1 since March 2015 As part of UNHCR’s winter assistance response for families living in cold areas, UNHCR through partner YGUSSWP, targeted 923 households in Bani Hushaysh Over 80 per cent and Hamdan Districts, Sana’a governorate. Out of those targeted, 842 families were have been displaced for identified as meeting the criteria for cash assistance beginning on 18 February. more than a year Following recent clashes in Nihm district, Sana’a governorate and Majzar district, Marib governorate, some 570 households were displaced to neighboring districts 66,499 families newly in Al Jawf governorate. New displacements were reported in Al Gail and Al Maslub displaced since districts, where UNHCR sub-national clusters are coordinating a response. All new IDPs beginning of 20192 were provided with a Rapid Response Mechanism package, consisting of food rations, hygiene products and dignity kits, while 62 IDP households received tents from partner 1.28 million YRC.