Ottawa Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

App for Serum Phosphate Control: a Randomized Controlled Trial
Original Investigation Multidisciplinary Team versus a “Phosphate-Counting” App for Serum Phosphate Control: A Randomized Controlled Trial Ana Cecilia Farfan-Ruiz,1 Daniel Czikk,2 Julie Leidecker,3 Tim Ramsay,4 Brendan McCormick,1,3 Kumanan Wilson,5 and Deborah Zimmerman 1,3 Abstract Background Hyperphosphatemia is almost universal in well-nourished patients with ESKD treated with dialysis due to an imbalance between dietary intake and phosphate removal via residual kidney function and dialysis. Although food phosphate content can vary dramatically between meals, the current standard is to prescribe a fixed dose of phosphate binder that may not match meal phosphate intake. The primary objective of our study was to determine if the use of an app that matches phosphate binder dose with food phosphate content would be associated with an improvement in serum phosphate and a reduction in calcium carbonate intake compared with the multidisciplinary renal team. Methods Eighty patients with ESKD treated with peritoneal dialysis at a tertiary care hospital in Canada were randomized to the standard of care for serum phosphate management (multidisciplinary renal team) versus the OkKidney app. Serum phosphate was measured at baseline and then monthly for 3 months with adjustments to phosphate management as deemed necessary by the multidisciplinary team (control) or the phosphate binder multiplier in the OkKidney app (intervention) on the basis of the laboratory values. The primary analysis was an unpaired t test of the serum phosphate at study completion. Results The participants were 56 (614) years old, and 54% were men; the most common cause of ESKD was diabetes mellitus. -
List of Contributors
List of Contributors ADAMS, P.C., London Health Sciences Centre-University Campus, 339 Windermere Rd., London, ON N6A 5A5. Tel: (519) 858-5125 Fax: (519) 858-5114 E-mail: [email protected] ALLARD, J.P., University Health Network-Toronto General Hospital, EW 217A-200 Elizabeth St., Toronto, ON M5G 2C4. Tel: (416) 340-5159 Fax: (416) 348-0065 E-mail: [email protected] ARCHAMBAULT, A.P., Hôpital Maisonneuve-Rosemont, 5415 boulevard de l’Assomption, Montréal, QC H1T 2M4. Tel: (514) 252-3822 Fax: (514) 252-3486 ARMSTRONG, D., Associate Professor, Division of Gastroenterology, Chief of Clinical Service, Division of Gastroenterology, Hamilton Health Sciences, McMaster University Medical Centre, HSC-4W8-1200 Main St. W, Hamilton, ON L8N 3Z5. Tel: (905) 521-2100 ext. 76404 Fax: (905) 521-4958 E-mail: [email protected] BAIK, S.K., Associate Professor, Division of Gastroenterology and Hepatology, Department of Internal Medicine, Yonsei University, Wonju College of Medicine, 162 Ilsan-dong, Wonju, South Korea 220-701. Tel: (82) 33-741-1223 Fax: (82) 33-745-6782 E-mail: [email protected] BAIN, V.G., Director, Liver Unit, University of Alberta, 205 College Plaza, 8215- 112th St., Calgary, AB T6G 2C8. Tel: (780) 492-8128 Fax: (780) 492-8130 E-mail: [email protected] BECK, I.T., Gastroenterology/Internal Medicine, Hotel Dieu Hospital, 166 Brock St., Kingston, ON K7L 5G2. Tel: (613) 544-0225 Fax: (613) 544-3114 E-mail: [email protected] 2 list of contributors BURKE, J., Queen Elizabeth II Health Sciences Centre, 1278 Tower Rd., Halifax, NS B3H 2Y9. -

Release of 2018 Research Reports
RELEASE OF 2018 RESEARCH REPORTS A special workshop for BIA members and partners AGENDA ¡ 8:30: Welcome & Introductions ¡ 8:40: 2018 BIA Member Census Report ¡ 9:00: 2018 Retail Trade Area Analysis ¡ 9:20: Takeaways for the BIA ¡ 9:30: Questions & Discussion WELCOME AND INTRODUCTIONS ¡ Name and business/ organizational affiliation 2018 BIA MEMBER CENSUS REPORT Michel Frojmovic, Creative Neighbourhoods Wellington West BIA 5 November 2018 Market Research Program Highlights from 2012-2018 Presented by Michel Frojmovic BIA market research program highlights Part 1 Census of businesses ◦ What types of businesses are here? ◦ How are they doing? ◦ Delivered every year since 2014 BIA market research program highlights Part 2 Visitor Survey ◦ Who visits the BIA neighbourhood? ◦ How do they get here? ◦ How much do they spend? ◦ Conducted annually from 2012-2017 How the BIA uses the Market Research 1. Member Engagement 2. Marketing & promotion 3. Understanding the Local Economy https://wellingtonwest.ca/a-business/ Wellington West BIA Business Census Door-to-door and floor- to-floor survey of all non-residential locations within the BIA Over 80 variables collected on a range of topics of relevance to the BIA, its members and potential members WWBIA boundary divided into 10 zones, each containing similar numbers of businesses. Used for analysis and comparison. Figure 1. Business census: Basic profile 2018 2014 Total # of unique non-residential locations 594 (businesses, non-profits, parks, parking lots; excludes home- 556 based businesses, street food vendors) 542 Members (property is levied) 505 52 Non-members 51 Figure 2. Businesses by category, 2018 Stores & Boutiques, Arts & Culture, 7% 13% Community Services, 12% Restaurants, 15% Food Services, 5% Health & Beauty, 18% Professional Services, 30% Figure 3. -

Portrait of an Academic Hospital the French Version of the Community Report Is Available at Rapportannuel.Hopitalmontfort.Com
MONTFORT 101: Portrait of an Academic Hospital The french version of the community report is available at rapportannuel.hopitalmontfort.com Hôpital Montfort June 2016 Message from the leadership team The year 2015-2016 was a turning point in Montfort’s evolution as an academic hospital. Intense reflection, nourished by the experiences and accomplishments of our 2011-2015 strategic plan led to the development of a new strategy. Therefore, it is with great pleasure that we present you with the Hôpital Montfort 2016-2021 Strategy: Mission Hôpital Montfort is Ontario’s Francophone Academic Hospital, offering exemplary person-centred care. Vision Your hospital of reference for outstanding services, designed with and for you. Values Our daily actions are guided by compassion, excellence, respect, accountability and mutual support. Our 2016–2021 strategy is based on four major objectives. Over the next five years, through the work of the entire Montfort Team, these objectives will translate into results with a positive impact on our community. Our objectives are: • To enhance targeted clinical services • To become a clinical centre of excellence in multimorbidity • To achieve the attributes of an academic hospital • To fulfill our provincial mandate Our new mission and its accompanying strategy will expand Montfort’s role as an academic hospital. This designation was conferred in June 2013, and the impact of this new status is felt each day with growing intensity. We are often asked: What does it change for Montfort to be an academic hospital? The answer is simple: an academic hospital stands out for the exemplary care it offers its patients, thepractical teaching it provides for the next generation of healthcare professionals, and the research it conducts to advance knowledge in health and medicine. -

Ottawa Quality and Patient Safety Conference
2019 Ottawa Patient Safety Conference Hosted by The Ottawa Hospital IQ@TOH Overview The Ottawa Hospital and IQ@TOH are proud to present the 2019 Ottawa Patient Safety Conference on November 1. The conference is an opportunity to share and learn about relevant practices to improve the quality and safety of care. This year’s theme is: “How Education Can Drive Innovation to Enhance Patient Safety” Our speakers will include prominent leaders in the field of patient safety, technology, education and innovation. Audience members will hear from keynote speakers are Dr. Brian Hodges and Dr. Marcia Clark, as well as a panel of experts. The conference is open to health care professionals, managers, administrators and academics. This forum will provide both presenters and registrants with a valuable opportunity to share innovative practices from diverse perspectives to: • Identify barriers and facilitators in the current health care environment for promoting patient safety • Integrate different perspectives to co-create educational solutions for patient safety • Propose educational solutions for improving patient safety within your context Planning Committee Dr. Alan Forster (Chair), Dr. Jerry Maniate, Samantha Hamilton (Conference Director), Leanne Bulsink (Conference Coordinator), Dr. Glen Posner, Dr. Lynn Ashdown, Dr. Eric Wooltorton, Thomas Hayes, Tracy Wrong, Melissa Brett, Lisa Freeman, David Molson, Venessa Goulet, Brooke Peloquin Catherine Foglietta. 1 Ottawa Quality & Patient Safety Conference Facilitated Interactive Session New to the conference this year is an interactive session where expert facilitators will assist attendees in sharing ideas and creating recommendations on how education can be enhanced to improve patient safety in Canada. After the conference, a consolidated summary of the recommendations will be created and shared with attendees. -

Planning Your Scheduled Cesarean Birth
Planning Your Scheduled Cesarean Birth THE OTTAWA HOSPITAL CP18 D (12/2013) Disclaimer This is general information developed by The Ottawa Hospital. It is not intended to replace the advice of a qualified health-care provider. Please consult your health-care provider who will be able to determine the appropriateness of the information for your specific situation. All rights reserved. No part of the contents of this book may be produced or transmitted in any form or by any means, without the written permission of The Ottawa Hospital, Clinical Pathway Project Team. © The Ottawa Hospital, December, 2013. Table of Contents Checklist: Evening before surgeryy . 2 Eating and Drinking Instructions . 3 The Day of Surgery In the morning before coming to the hospital . 3 Coming to the hospital . 5 At the hospital . 5 In the Operating Room (OR). 6 Preparing you for the operation and your baby’s birth . 6 In the Recovery Room (PACU) Family Presence . 7 Your Nursing Care . 8 Exercises . 9 On the Mother Baby Unit . 9 Civic Campus Map – 4th Floorr . 10 General Campus Map – 8th Floorr. 11 Birthing Unit Cesarean Birth Patient Handout My surgery will be on __________________________ at ________________ hr at The Ottawa Hospital _______________________________________ Campus Time of arrival to hospital: ____________________________________________ D Civic Campus D General Campus Finding out the time of surgery: Finding out the time of surgery: We will call you the day/evening We will call you day/evening before before your surgery. your surgery. Coming for surgery: Coming for surgery: Come to the Birthing Unit, 4th fl oor Come to the Birthing Unit, 8th fl oor (See map on page 10) (See map on page 11). -

Staff Profiles
DEPARTMENT OF OPHTHALMOLOGY – The Ottawa Hospital, Eye Institute and Riverside Eye Care Centre NAME SPECIALTY PROFILE Dr. Maryam Abtahi Cataract Surgeon and 205-2148 Carling Ave. Glaucoma Ottawa ON K2A 1H1 Tel: 613 596-0300 Fax: 613 596-0848 Dr. Peter Agapitos Comprehensive MD, 1982,uOttawa Ophthalmology Internship- McGill University, 1982-83 209 - 1919 Riverside Dr. Cataract Surgery Residency, Internal Medicine, uOttawa, 1983-84 and Ottawa ON K1H 1A2 Corneal Transplants Ophthalmology, uOttawa, 1984-87 Tel: 613 236-9929 Refractive Surgery RCPSC Certificate: 1987 Fax: 613 236-6801 ABO Diploma, 1988 Fellowship: Cornea, External Disease and Anterior Segment Surgery, U of Minnesota 1987-89. Head, Department of Ophthalmology, Riverside Campus Eye Care Centre, 2009 - 2019 Practice Focus: Cataract/IOL, Cornea/External Disease, ABO Diploma, 1988 Corneal Transplants Dr. Danah Albreiki Neuro- MMBS University of King Faisal, 2004 Eye Institute, TOH, General Ophthalmology Dammam Saudi Arabia Campus, 501 Smyth Rd. FRCSC (Ophthalmology), University of Ottawa, 2011 Ottawa ON K1H 8L6 Adult Strabismus Sub-specialty: Neuro-ophthalmology, University of Ottawa, 2012 Tel: 613 739-6805 Practice Focus: Neuro-ophthalmology and Adult Strabismus Fax: 613 739-6889 Dr. Kashif Baig Cornea MD, CM: 2002, McGill University Anterior Segment Residency: Ophthalmology, McGill University, 2003-2007 Eye Institute, TOH General Surgery Fellowship: Cornea, External Disease and Refractive Surgery, Campus, 501 Smyth Road Refractive Surgery Price Vision Group, Indianapolis, IN, 2007-2008 Ottawa, ON K1H 8L6 Cataract Surgery FRCSC Certificate: 2007 Tel: 613 737-8473 office MBA Diploma: 1999 Fax: 613 739-2733 Practice Focus: Cornea, Anterior Segment Surgery, Refractive Surgery, and Cataract Surgery Precision Cornea Centre Tel: 613 746-2244 Fax 613 739-2733 Dr. -

Ottawa Hospital Case Study
Nuance Healthcare Solutions Case Study Dragon® Medical Network Edition The Ottawa Hospital improves patient care and lowers transcription costs Challenge Solution Results – Improve continuity of care – Dragon Medical Network – Templates improve – Enhance patient safety and Edition complements the documentation accuracy, quality of care Oasis EHR thoroughness and consistency – Reduce transcription costs – Documentation is available two weeks faster – Documentation is accessible throughout the circle of care – Transcription savings of $7 million – $11 million projected savings over 5 years – 37,000 documents created per month vs 3,000 previously Summary The Ottawa Hospital is a 1,149-bed non-profit, academic health sciences center in Ottawa, Canada. It serves 1.3 million people across Eastern Ontario. The Ottawa Hospital was looking to improve patient safety and quality of care by giving all providers within the hospital and throughout the community immediate access to patient records. At the same time, it wanted to be a responsible steward of its financial resources. Nuance Healthcare Solutions Case Study Dragon® Medical Network Edition “ We expect to save $11 million over 5 years because of Dragon Medical. The accessibility of patient records—possible because our clinicians are documenting care electronically—is truly exciting.” Dr. Glen Geiger, CMIO The Ottawa Hospital Ottawa, Canada The first hospital in Canada to implement Dragon® Improved continuity of care Medical Network Edition alongside its Oasis EHR When physicians used phone dictation, the average solution, The Ottawa Hospital has succeeded in ensuring turnaround time for notes was 14 days. Now physicians timely access to accurate and comprehensive patient enter them immediately into the EHR. -

Arrangement and Description of Peterborough's Historical Hospital Records Includes
Arrangement and Description of Peterborough’s Historical Hospital Records Includes: Final Report By Rebecca Lindsay Completed for: Peterborough Museum and Archive Supervising Professor: Sharon Beaucage-Johnson, Trent University Trent Centre for Community-Based Education Department: Forensics Course Code: 4890Y Course Name: Forensic Community-Based Education Research Project Term: Fall/Winter 2011-12 Date of Project Submission: April 2012 Project ID: 4219 Call Number: Table of Contents Abstract ........................................................................................................................................... 3 Acknowledgements ......................................................................................................................... 4 Ket Research Terms ........................................................................................................................ 5 Introduction .................................................................................................................................... 6 Methods ........................................................................................................................................ 10 Results ........................................................................................................................................... 15 Conclusion ..................................................................................................................................... 19 Literature Cited ............................................................................................................................ -

Carling Avenue, the Property Is in Close Proximity to the Ottawa Civic Hospital and the PARKING Royal Ottawa Mental Health Centre
CARLING 1081AVENUE [ PARKDALE MEDICAL BUILDING ] Jessica Whiting Sarah Al-Hakkak Senior Sales Representative Sales Representative +1 613 683 2208 +1 613 683 2212 [email protected] [email protected] CARLING 1081AVENUE PARKDALE MEDICAL BUILDING INCENTIVE: Sign a new 5+ year lease by September 30, 2019 to receive 6 months of net rent free! [ HIGHLIGHTS ] AVAILABLE AREA 662 SF - 6,917 SF NET RENT $16.00 PSF Turnkey options On-site parking Available available & rapid transit at immediately doorstep ADDITIONAL RENT Join existing medical tenants in a professionally managed building. $16.95 PSF Located at the corner of Parkdale Avenue and Carling Avenue, the property is in close proximity to the Ottawa Civic Hospital and the PARKING Royal Ottawa Mental Health Centre. On-site amenities include a café 1:1,000 SF | $100/MONTH and a pharmacy. CARLING 1081AVENUE PARKDALE MEDICAL BUILDING [ AVAILABLE SPACE ] SUITE SIZE (SF) B2 812 202 662 207 4,274 308 4,372 403 678 409 673 502 1,345 600 6,917 [ UPCOMING SPACE ] SUITE SIZE (SF) DATE 704 944 NOV 2019 705 2,000 JUNE 2019 706 2,000 JUNE 2019 ON-SITE CAFÉ CARLING 1081AVENUE [ FLOOR PLAN ] PARKDALE MEDICAL BUILDING SUITE 207 - 4,274 SF CARLING 1081AVENUE [ FLOOR PLAN ] PARKDALE MEDICAL BUILDING SUITE 409 - 673 SF CARLING 1081AVENUE [ FLOOR PLAN ] PARKDALE MEDICAL BUILDING SUITE 502 - 1,345 SF CARLING 1081AVENUE [ FLOOR PLAN ] PARKDALE MEDICAL BUILDING SUITE 600 - 6,917 SF PORTAGE BRIDGE ELGIN STREET EDDY STREET WELLINGTON STREET ALBERT STREET SLATER STREET CARLINGLAURIER AVENUE AVENUE -
Printer-Friendly Version
Compassionate People. World-Class Care. The Ottawa Hospital 2011-2012 Annual Report www.worldclasscare.ca Table of Content Welcome……………………………………………………………………………………….. 2 Success Stories……………………………………………………………………………..… 3 Changing practice, saving lives………………………………………………….…. 4 The virtual road to recovery…………………………………………………………. 7 Stem cell therapies: the future of regenerative medicine………………………... 9 Highlights………………………………………………………………………………………. 11 Patient Care…………………………………………………………………………... 12 Collaboration………………………………………………………………………….. 16 Research………………………………………………………………...................... 19 Fundraising…………………………………………………………………………… 23 At a Glance……………………………………………………………………………………. 24 Quality Indicators……………………………………………………………………………… 31 Financials……………………………………………………………………………………… 32 Contact Us…………………………………………………………………………………….. 33 1 In this 2011-2012 Annual Report, we want to share with you successes we‘ve experienced and the progress we‘ve made at The Ottawa Hospital (TOH) and across the region. Combining technology and research with expertise and compassion, our team is at the forefront of a medical revolution - creating a world-class facility with internationally renowned physicians, scientists and researchers dedicated to providing outstanding care to the citizens of Ottawa and beyond. The best care possible is what the community expects, and most importantly, it is what it deserves. TOH, with the support of its Board of Governors, has set a new and ambitious goal: to become a top 10 per cent performer in quality and safety of patient care in North America. We‘ve taken big strides towards reaching this goal – tracking measurable progress to each and every one of our targets. We‘re just so proud of our many innovations, some of which you‘ll see and read about right here in the 2011- 2012 report. This year you will meet Canadian diplomat Bushra Saeed. After being seriously injured in Afghanistan, it was TOH‘s leading-edge Rehabilitation Virtual Reality Laboratory and compassionate multidisciplinary care team that made all the difference in her rehabilitation. -
Revised 2021-08
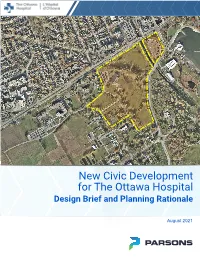
New Civic Development for The Ottawa Hospital Design Brief and Planning Rationale – Master Site Plan August 5th 2021 New Civic Development for The Ottawa Hospital Design Brief and Planning Rationale - Master Site Plan Applications for: Site Plan Control, Master Site Plan and Lifting of Holding Zone August 5th 2021 Prepared by: Parsons with HDR and GBA Page 1 New Civic Development for The Ottawa Hospital Design Brief and Planning Rationale - Master Site Plan August 5th 2021 TABLE OF CONTENTS 1.0 INTRODUCTION ................................................................................................................................................................ 1 1.1 Local Context .............................................................................................................................................................. 1 1.2 Site Significance ......................................................................................................................................................... 4 1.3 Existing Potential for Transportation Network .......................................................................................................... 4 1.4 Site Topography and Open Space ............................................................................................................................. 5 2.0 DESIGN BRIEF .................................................................................................................................................................. 6 2.1 Design Vision and Design