Local Immune Response in Bladder Pain Syndrome/Interstitial Cystitis ESSIC Type 3C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![UPK1B Antibody / Uroplakin 1B [Clone UPK1B/3081] (V8152)](https://docslib.b-cdn.net/cover/9189/upk1b-antibody-uroplakin-1b-clone-upk1b-3081-v8152-519189.webp)
UPK1B Antibody / Uroplakin 1B [Clone UPK1B/3081] (V8152)
UPK1B Antibody / Uroplakin 1B [clone UPK1B/3081] (V8152) Catalog No. Formulation Size V8152-100UG 0.2 mg/ml in 1X PBS with 0.1 mg/ml BSA (US sourced) and 0.05% sodium azide 100 ug V8152-20UG 0.2 mg/ml in 1X PBS with 0.1 mg/ml BSA (US sourced) and 0.05% sodium azide 20 ug V8152SAF-100UG 1 mg/ml in 1X PBS; BSA free, sodium azide free 100 ug Bulk quote request Availability 1-3 business days Species Reactivity Human Format Purified Clonality Monoclonal (mouse origin) Isotype Mouse IgG2b, kappa Clone Name UPK1B/3081 Purity Protein G affinity chromatography UniProt O75841 Localization Cell surface Applications Immunohistochemistry (FFPE) : 1-2ug/ml Limitations This UPK1B antibody is available for research use only. IHC staining of FFPE human urothelial carcinoma with UPK1B antibody. HIER: boil tissue sections in pH 9 10mM Tris with 1mM EDTA for 20 min and allow to cool before testing. IHC staining of FFPE human urothelial carcinoma with UPK1B antibody. HIER: boil tissue sections in pH 9 10mM Tris with 1mM EDTA for 20 min and allow to cool before testing. IHC staining of FFPE human urothelial carcinoma with UPK1B antibody. HIER: boil tissue sections in pH 9 10mM Tris with 1mM EDTA for 20 min and allow to cool before testing. Analysis of HuProt(TM) microarray containing more than 19,000 full-length human proteins using UPK1B antibody (clone UPK1B/3081). These results demonstrate the foremost specificity of the UPK1B/3081 mAb. Z- and S- score: The Z-score represents the strength of a signal that an antibody (in combination with a fluorescently-tagged anti-IgG secondary Ab) produces when binding to a particular protein on the HuProt(TM) array. -

Supplementary Materials
Supplementary materials Supplementary Table S1: MGNC compound library Ingredien Molecule Caco- Mol ID MW AlogP OB (%) BBB DL FASA- HL t Name Name 2 shengdi MOL012254 campesterol 400.8 7.63 37.58 1.34 0.98 0.7 0.21 20.2 shengdi MOL000519 coniferin 314.4 3.16 31.11 0.42 -0.2 0.3 0.27 74.6 beta- shengdi MOL000359 414.8 8.08 36.91 1.32 0.99 0.8 0.23 20.2 sitosterol pachymic shengdi MOL000289 528.9 6.54 33.63 0.1 -0.6 0.8 0 9.27 acid Poricoic acid shengdi MOL000291 484.7 5.64 30.52 -0.08 -0.9 0.8 0 8.67 B Chrysanthem shengdi MOL004492 585 8.24 38.72 0.51 -1 0.6 0.3 17.5 axanthin 20- shengdi MOL011455 Hexadecano 418.6 1.91 32.7 -0.24 -0.4 0.7 0.29 104 ylingenol huanglian MOL001454 berberine 336.4 3.45 36.86 1.24 0.57 0.8 0.19 6.57 huanglian MOL013352 Obacunone 454.6 2.68 43.29 0.01 -0.4 0.8 0.31 -13 huanglian MOL002894 berberrubine 322.4 3.2 35.74 1.07 0.17 0.7 0.24 6.46 huanglian MOL002897 epiberberine 336.4 3.45 43.09 1.17 0.4 0.8 0.19 6.1 huanglian MOL002903 (R)-Canadine 339.4 3.4 55.37 1.04 0.57 0.8 0.2 6.41 huanglian MOL002904 Berlambine 351.4 2.49 36.68 0.97 0.17 0.8 0.28 7.33 Corchorosid huanglian MOL002907 404.6 1.34 105 -0.91 -1.3 0.8 0.29 6.68 e A_qt Magnogrand huanglian MOL000622 266.4 1.18 63.71 0.02 -0.2 0.2 0.3 3.17 iolide huanglian MOL000762 Palmidin A 510.5 4.52 35.36 -0.38 -1.5 0.7 0.39 33.2 huanglian MOL000785 palmatine 352.4 3.65 64.6 1.33 0.37 0.7 0.13 2.25 huanglian MOL000098 quercetin 302.3 1.5 46.43 0.05 -0.8 0.3 0.38 14.4 huanglian MOL001458 coptisine 320.3 3.25 30.67 1.21 0.32 0.9 0.26 9.33 huanglian MOL002668 Worenine -

Liquid Biopsy Biomarkers in Urine: a Route Towards Molecular Diagnosis and Personalized Medicine of Bladder Cancer
Journal of Personalized Medicine Review Liquid Biopsy Biomarkers in Urine: A Route towards Molecular Diagnosis and Personalized Medicine of Bladder Cancer Matteo Ferro 1,† , Evelina La Civita 2,†, Antonietta Liotti 2, Michele Cennamo 2, Fabiana Tortora 3 , Carlo Buonerba 4,5, Felice Crocetto 6 , Giuseppe Lucarelli 7 , Gian Maria Busetto 8 , Francesco Del Giudice 9 , Ottavio de Cobelli 1,10, Giuseppe Carrieri 9, Angelo Porreca 11, Amelia Cimmino 12,* and Daniela Terracciano 2,* 1 Department of Urology of European Institute of Oncology (IEO), IRCCS, Via Ripamonti 435, 20141 Milan, Italy; [email protected] (M.F.); [email protected] (O.d.C.) 2 Department of Translational Medical Sciences, University of Naples “Federico II”, 80131 Naples, Italy; [email protected] (E.L.C.); [email protected] (A.L.); [email protected] (M.C.) 3 Institute of Protein Biochemistry, National Research Council, 80131 Naples, Italy; [email protected] 4 CRTR Rare Tumors Reference Center, AOU Federico II, 80131 Naples, Italy; [email protected] 5 Environment & Health Operational Unit, Zoo-Prophylactic Institute of Southern Italy, 80055 Portici, Italy 6 Department of Neurosciences, Sciences of Reproduction and Odontostomatology, University of Naples Federico II, 80131 Naples, Italy; [email protected] 7 Department of Emergency and Organ Transplantation, Urology, Andrology and Kidney Transplantation Unit, University of Bari, 70124 Bari, Italy; [email protected] 8 Department of Urology and Organ Transplantation, -

A Transcriptomic Atlas of Aged Human Microglia
ARTICLE DOI: 10.1038/s41467-018-02926-5 OPEN A transcriptomic atlas of aged human microglia Marta Olah1,2, Ellis Patrick 3, Alexandra-Chloe Villani2,4, Jishu Xu 2, Charles C. White2, Katie J. Ryan5, Paul Piehowski 6, Alifiya Kapasi6, Parham Nejad2, Maria Cimpean 5, Sarah Connor1,2, Christina J. Yung1, Michael Frangieh5, Allison McHenry5, Wassim Elyaman1,2, Vlad Petyuk 6, Julie A. Schneider7, David A. Bennett7, Philip L. De Jager 1,2 & Elizabeth M. Bradshaw1,2 With a rapidly aging global human population, finding a cure for late onset neurodegenerative diseases has become an urgent enterprise. However, these efforts are hindered by the lack of 1234567890():,; understanding of what constitutes the phenotype of aged human microglia—the cell type that has been strongly implicated by genetic studies in the pathogenesis of age-related neuro- degenerative disease. Here, we establish the set of genes that is preferentially expressed by microglia in the aged human brain. This HuMi_Aged gene set captures a unique phenotype, which we confirm at the protein level. Furthermore, we find this gene set to be enriched in susceptibility genes for Alzheimer’s disease and multiple sclerosis, to be increased with advancing age, and to be reduced by the protective APOEε2 haplotype. APOEε4 has no effect. These findings confirm the existence of an aging-related microglial phenotype in the aged human brain and its involvement in the pathological processes associated with brain aging. 1 Center for Translational & Computational Neuroimmunology, Department of Neurology, Columbia University Medical Center, New York City, NY 10032, USA. 2 Program in Medical and Population Genetics, Broad Institute, Cambridge, MA 02142, USA. -

Single-Cell Transcriptomes Reveal a Complex Cellular Landscape in the Middle Ear and Differential Capacities for Acute Response to Infection
fgene-11-00358 April 9, 2020 Time: 15:55 # 1 ORIGINAL RESEARCH published: 15 April 2020 doi: 10.3389/fgene.2020.00358 Single-Cell Transcriptomes Reveal a Complex Cellular Landscape in the Middle Ear and Differential Capacities for Acute Response to Infection Allen F. Ryan1*, Chanond A. Nasamran2, Kwang Pak1, Clara Draf1, Kathleen M. Fisch2, Nicholas Webster3 and Arwa Kurabi1 1 Departments of Surgery/Otolaryngology, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States, 2 Medicine/Center for Computational Biology & Bioinformatics, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States, 3 Medicine/Endocrinology, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States Single-cell transcriptomics was used to profile cells of the normal murine middle ear. Clustering analysis of 6770 transcriptomes identified 17 cell clusters corresponding to distinct cell types: five epithelial, three stromal, three lymphocyte, two monocyte, Edited by: two endothelial, one pericyte and one melanocyte cluster. Within some clusters, Amélie Bonnefond, Institut National de la Santé et de la cell subtypes were identified. While many corresponded to those cell types known Recherche Médicale (INSERM), from prior studies, several novel types or subtypes were noted. The results indicate France unexpected cellular diversity within the resting middle ear mucosa. The resolution of Reviewed by: Fabien Delahaye, uncomplicated, acute, otitis media is too rapid for cognate immunity to play a major Institut Pasteur de Lille, France role. Thus innate immunity is likely responsible for normal recovery from middle ear Nelson L. S. Tang, infection. The need for rapid response to pathogens suggests that innate immune The Chinese University of Hong Kong, China genes may be constitutively expressed by middle ear cells. -

Comprehensive Analysis Reveals Novel Gene Signature in Head and Neck Squamous Cell Carcinoma: Predicting Is Associated with Poor Prognosis in Patients
5892 Original Article Comprehensive analysis reveals novel gene signature in head and neck squamous cell carcinoma: predicting is associated with poor prognosis in patients Yixin Sun1,2#, Quan Zhang1,2#, Lanlin Yao2#, Shuai Wang3, Zhiming Zhang1,2 1Department of Breast Surgery, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China; 2School of Medicine, Xiamen University, Xiamen, China; 3State Key Laboratory of Cellular Stress Biology, School of Life Sciences, Xiamen University, Xiamen, China Contributions: (I) Conception and design: Y Sun, Q Zhang; (II) Administrative support: Z Zhang; (III) Provision of study materials or patients: Y Sun, Q Zhang; (IV) Collection and assembly of data: Y Sun, L Yao; (V) Data analysis and interpretation: Y Sun, S Wang; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Zhiming Zhang. Department of Surgery, The First Affiliated Hospital of Xiamen University, Xiamen, China. Email: [email protected]. Background: Head and neck squamous cell carcinoma (HNSC) remains an important public health problem, with classic risk factors being smoking and excessive alcohol consumption and usually has a poor prognosis. Therefore, it is important to explore the underlying mechanisms of tumorigenesis and screen the genes and pathways identified from such studies and their role in pathogenesis. The purpose of this study was to identify genes or signal pathways associated with the development of HNSC. Methods: In this study, we downloaded gene expression profiles of GSE53819 from the Gene Expression Omnibus (GEO) database, including 18 HNSC tissues and 18 normal tissues. -
A Validation and Extended Description of the Lund Taxonomy for Urothelial
www.nature.com/scientificreports OPEN A validation and extended description of the Lund taxonomy for urothelial carcinoma using the Received: 11 July 2017 Accepted: 19 February 2018 TCGA cohort Published: xx xx xxxx Nour-al-dain Marzouka1, Pontus Eriksson1, Carlos Rovira1, Fredrik Liedberg2, Gottfrid Sjödahl2 & Mattias Höglund1 Global gene expression analysis has been a major tool for urothelial carcinoma subtype discovery. This approach has revealed extensive complexity both in intrinsic features of the tumor cells and in the microenvironment. However, global gene expression cannot distinguish between gene expression signals originating from the tumor cells proper and from normal cells in the biopsy. Here, we use a large cohort of advanced urothelial carcinomas for which both gene expression data and extensive immunohistochemistry are available to create a supervised mRNA expression centroid classifer. This classifer identifes the major Lund taxonomy tumor cell phenotypes as defned by IHC. We apply this classifer to the independent TCGA dataset and show excellent associations between identifed subtypes and genomic features. We validate a progressed version of Urothelial-like A (UroA-Prog) that shows FGFR3 mutations and CDKN2A deletions, and we show that the variant Urothelial-like C is almost devoid of FGFR3 mutations. We show that Genomically Unstable tumors are very distinct from Urothelial-like tumors at the genomic level, and that tumors classifed as Basal/SCC-like all complied with the established defnition for Basal/SCC-like tumors. We identify the Mesenchymal-like and Small- cell/Neuroendocrine-like subtypes, and demonstrate that patients with UroB and Sc/NE-like tumors show the worst overall survival. -
Downloaded from the Mouse Lysosome Gene Database, Mlgdb
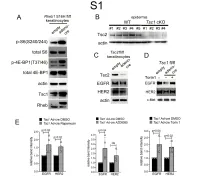
1 Supplemental Figure Legends 2 3 Supplemental Figure S1: Epidermal-specific mTORC1 gain-of-function models show 4 increased mTORC1 activation and down-regulate EGFR and HER2 protein expression in a 5 mTORC1-sensitive manner. (A) Immunoblotting of Rheb1 S16H flox/flox keratinocyte cultures 6 infected with empty or adenoviral cre recombinase for markers of mTORC1 (p-S6, p-4E-BP1) 7 activity. (B) Tsc1 cKO epidermal lysates also show decreased expression of TSC2 by 8 immunoblotting of the same experiment as in Figure 2A. (C) Immunoblotting of Tsc2 flox/flox 9 keratinocyte cultures infected with empty or adenoviral cre recombinase showing decreased EGFR 10 and HER2 protein expression. (D) Expression of EGFR and HER2 was decreased in Tsc1 cre 11 keratinocytes compared to empty controls, and up-regulated in response to Torin1 (1µM, 24 hrs), 12 by immunoblot analyses. Immunoblots are contemporaneous and parallel from the same biological 13 replicate and represent the same experiment as depicted in Figure 7B. (E) Densitometry 14 quantification of representative immunoblot experiments shown in Figures 2E and S1D (r≥3; error 15 bars represent STDEV; p-values by Student’s T-test). 16 17 18 19 20 21 22 23 Supplemental Figure S2: EGFR and HER2 transcription are unchanged with epidermal/ 24 keratinocyte Tsc1 or Rptor loss. Egfr and Her2 mRNA levels in (A) Tsc1 cKO epidermal lysates, 25 (B) Tsc1 cKO keratinocyte lysates and(C) Tsc1 cre keratinocyte lysates are minimally altered 26 compared to their respective controls. (r≥3; error bars represent STDEV; p-values by Student’s T- 27 test). -

Monoclonal Antibody(Clone: UPK1B/3102)
9853 Pacific Heights Blvd. Suite D. San Diego, CA 92121, USA Tel: 858-263-4982 Email: [email protected] 36-3347: Anti-Uroplakin 1B (Urothelial Differentiation Marker) Monoclonal Antibody(Clone: UPK1B/3102) Clonality : Monoclonal Clone Name : UPK1B/3102 Application : ELISA, IHC Reactivity : Human Gene : UPK1B Gene ID : 7348 Uniprot ID : O75841 Alternative Name : Tetraspanin-20; Tspan-20; TSPAN20; UP1b; UPIb; UPK1B; Uroplakin-1b Isotype : Mouse IgG1, kappa Recombinant fragment (around aa 109-229) of human Uroplakin 1B (UPK1B) protein (exact Immunogen Information : sequence is proprietary) Description The protein encoded by this gene is a member of the transmembrane 4 superfamily, also known as the tetraspanin family. Most of these members are cell-surface proteins that are characterized by the presence of four hydrophobic domains. The proteins mediate signal transduction events that play a role in the regulation of cell development, activation, growth and motility. This encoded protein is found in the asymmetrical unit membrane (AUM) where it can form a complex with other transmembrane 4 superfamily proteins. It may play a role in normal bladder epithelial physiology, possibly in regulating membrane permeability of superficial umbrella cells or in stabilizing the apical membrane throµgh AUM/cytoskeletal interactions.UPK1B is expressed by terminally differentiated urothelial cells. Product Info Amount : 20 µg / 100 µg 200 µg/ml of Ab Purified from Bioreactor Concentrate by Protein A/G. Prepared in 10mM PBS with Content : 0.05% BSA & 0.05% azide. Also available WITHOUT BSA & azide at 1.0mg/ml. Antibody with azide - store at 2 to 8°C. Antibody without azide - store at -20 to -80°C. -

Oviduct Extracellular Vesicles Protein Content and Their Role During Oviduct–Embryo Cross-Talk
REPRODUCTIONRESEARCH Oviduct extracellular vesicles protein content and their role during oviduct–embryo cross-talk Carmen Almiñana1, Emilie Corbin1, Guillaume Tsikis1, Agostinho S Alcântara-Neto1, Valérie Labas1,2, Karine Reynaud1, Laurent Galio3, Rustem Uzbekov4,5, Anastasiia S Garanina4, Xavier Druart1 and Pascal Mermillod1 1UMR0085 Physiologie de la Reproduction et des Comportements (PRC), Institut National de la Recherche Agronomique (INRA)/CNRS/Univ. Tours, Nouzilly, France, 2UFR, CHU, Pôle d’Imagerie de la Plate-forme de Chirurgie et Imagerie pour la Recherche et l’Enseignement (CIRE), INRA Nouzilly, France, 3UMR1198, Biologie du Développement et Reproduction, INRA Jouy-en-Josas, France, 4Laboratoire Biologie Cellulaire et Microscopie Electronique, Faculté de Médecine, Université François Rabelais, Tours, France and 5Faculty of Bioengineering and Bioinformatics, Moscow State University, Moscow, Russia Correspondence should be addressed to C Almiñana; Email: [email protected] Abstract Successful pregnancy requires an appropriate communication between the mother and the embryo. Recently, exosomes and microvesicles, both membrane-bound extracellular vesicles (EVs) present in the oviduct fluid have been proposed as key modulators of this unique cross-talk. However, little is known about their content and their role during oviduct-embryo dialog. Given the known differences in secretions by in vivo and in vitro oviduct epithelial cells (OEC), we aimed at deciphering the oviduct EVs protein content from both sources. Moreover, we analyzed their functional effect on embryo development. Our study demonstrated for the first time the substantial differences between in vivo and in vitro oviduct EVs secretion/content. Mass spectrometry analysis identified 319 proteins in EVs, from which 186 were differentially expressed when in vivo and in vitro EVs were compared (P < 0.01). -

UPK1B Polyclonal Antibody Gene Symbol: UPK1B
UPK1B polyclonal antibody Gene Symbol: UPK1B Catalog Number: PAB25730 Gene Alias: TSPAN20, UPIB, UPK1 Regulatory Status: For research use only (RUO) Gene Summary: The protein encoded by this gene is a member of the transmembrane 4 superfamily, also Product Description: Rabbit polyclonal antibody raised known as the tetraspanin family. Most of these members against synthetic peptide of UPK1B. are cell-surface proteins that are characterized by the presence of four hydrophobic domains. The proteins Immunogen: A synthetic peptide corresponding to 17 mediate signal transduction events that play a role in the amino acids at internal region of human UPK1B. regulation of cell development, activation, growth and motility. This encoded protein is found in the Host: Rabbit asymmetrical unit membrane (AUM) where it can form a complex with other transmembrane 4 superfamily Reactivity: Human,Mouse,Rat proteins. It may play a role in normal bladder epithelial Applications: ELISA, IHC, WB-Ti physiology, possibly in regulating membrane (See our web site product page for detailed applications permeability of superficial umbrella cells or in stabilizing information) the apical membrane through AUM/cytoskeletal interactions. The use of alternate polyadenylation sites Protocols: See our web site at has been found for this gene. [provided by RefSeq] http://www.abnova.com/support/protocols.asp or product page for detailed protocols Specificity: At least two isoforms of UPK1B are known to exist; this antibody will recognize both isoforms. UPK1B antibody is predicted to not cross-react with other tetraspanin protein family members. Form: Liquid Purification: Peptide affinity purification Concentration: 1 mg/mL Isotype: IgG Recommend Usage: Western Blot (0.5-1 ug/mL) Immunohistochemistry (5 ug/mL) The optimal working dilution should be determined by the end user. -
The GUDMAP Database – an Online Resource for Genitourinary Research Simon D
TECHNICAL PAPER RESEARCH ARTICLE 2845 Development 138, 2845-2853 (2011) doi:10.1242/dev.063594 © 2011. Published by The Company of Biologists Ltd The GUDMAP database – an online resource for genitourinary research Simon D. Harding1,*, Chris Armit2, Jane Armstrong2, Jane Brennan2, Ying Cheng1, Bernard Haggarty1, Derek Houghton1, Sue Lloyd-MacGilp2, Xingjun Pi1, Yogmatee Roochun1, Mehran Sharghi1, Christopher Tindal1, Andrew P. McMahon3, Brian Gottesman3, Melissa H. Little4, Kylie Georgas4, Bruce J. Aronow5, S. Steven Potter6, Eric W. Brunskill6, E. Michelle Southard-Smith7, Cathy Mendelsohn8, Richard A. Baldock1, Jamie A. Davies2 and Duncan Davidson1 SUMMARY The GenitoUrinary Development Molecular Anatomy Project (GUDMAP) is an international consortium working to generate gene expression data and transgenic mice. GUDMAP includes data from large-scale in situ hybridisation screens (wholemount and section) and microarray gene expression data of microdissected, laser-captured and FACS-sorted components of the developing mouse genitourinary (GU) system. These expression data are annotated using a high-resolution anatomy ontology specific to the developing murine GU system. GUDMAP data are freely accessible at www.gudmap.org via easy-to-use interfaces. This curated, high-resolution dataset serves as a powerful resource for biologists, clinicians and bioinformaticians interested in the developing urogenital system. This paper gives examples of how the data have been used to address problems in developmental biology and provides a primer for those wishing to use the database in their own research. KEY WORDS: Database, Gene expression, Genitourinary, In situ hybridisation, Microarray INTRODUCTION the expression of thousands of transcripts, annotated at high Mammalian development is complicated; each of the thousands of resolution and made easily accessible to manual and automated embryological events that operate in sequence to make a mature queries.