Nerve Damage Related to Implant Dentistry Issues Associated with Avoiding, Diagnosing, and Managing Damage to the Trigeminal Nerve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Alveolar Ridge Preservation at Different Anatomical Locations
ALVEOLAR RIDGE PRESERVATION AT DIFFERENT ANATOMICAL LOCATIONS- CLINICAL AND HISTOLOGICAL EVALUATION OF TREATMENT OUTCOME MASTERS THESIS Presented in Partial Fulfillment of Requirements for the Degree Master of Science in Dentistry in the Graduate School of The Ohio State University By Mabel Salas, DDS Graduate Program in Dentistry The Ohio State University 2009 Master’s Examination Committee: Binnaz Leblebicioglu, DDS, MS, PhD, Advisor Dimitris N. Tatakis, DDS, PhD Suda Agarwal, PhD Do-Gyoon Kim, PhD Copyright by Mabel Salas 2009 ABSTRACT Background: Alveolar ridge preservation (ARP) is a surgical technique designed to prevent naturally occurring post-extraction bone resorption. It is well documented that alveolar bone height and width are reduced following tooth extraction as a result of physiologic bone remodeling. Depending on the type of post-extraction intrabony defect, an immediate or early implant placement itself may preserve the bone height and width. However, if the defect is generally too wide for immediate and/or early implant placement, it is recommended to perform ARP surgery to preserve the bone volume for future implant placement. The purpose of this study was to investigate clinical and histological healing outcomes following ARP performed on molar and premolar sites by using freeze-dried bone allograft (FDBA) together with a collagen membrane. Maxillary and mandibular sextants were compared for clinical and histological parameters. Methods: Patients who were scheduled to have tooth extraction and implant placement for a molar or premolar tooth were included into this study. Inclusion criteria were single tooth extraction with intact mesial and distal adjacent teeth. Exclusion criteria were smokers, systemic health problems that may affect wound healing and acute infection ii that may prevent bone graft placement. -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Periodontal Ligament, Cementum, and Alveolar Bone in the Oldest Herbivorous Tetrapods, and Their Evolutionary Significance
Periodontal Ligament, Cementum, and Alveolar Bone in the Oldest Herbivorous Tetrapods, and Their Evolutionary Significance Aaron R. H. LeBlanc*, Robert R. Reisz Department of Biology, University of Toronto Mississauga, Mississauga, Ontario, Canada Abstract Tooth implantation provides important phylogenetic and functional information about the dentitions of amniotes. Traditionally, only mammals and crocodilians have been considered truly thecodont, because their tooth roots are coated in layers of cementum for anchorage of the periodontal ligament, which is in turn attached to the bone lining the alveolus, the alveolar bone. The histological properties and developmental origins of these three periodontal tissues have been studied extensively in mammals and crocodilians, but the identities of the periodontal tissues in other amniotes remain poorly studied. Early work on dental histology of basal amniotes concluded that most possess a simplified tooth attachment in which the tooth root is ankylosed to a pedestal composed of ‘‘bone of attachment’’, which is in turn fused to the jaw. More recent studies have concluded that stereotypically thecodont tissues are also present in non-mammalian, non-crocodilian amniotes, but these studies were limited to crown groups or secondarily aquatic reptiles. As the sister group to Amniota, and the first tetrapods to exhibit dental occlusion, diadectids are the ideal candidates for studies of dental evolution among terrestrial vertebrates because they can be used to test hypotheses of development and homology in deep time. Our study of Permo-Carboniferous diadectid tetrapod teeth and dental tissues reveal the presence of two types of cementum, periodontal ligament, and alveolar bone, and therefore the earliest record of true thecodonty in a tetrapod. -

The Preservation of Alveolar Bone Ridge During Tooth Extraction Marius Kubilius, Ricardas Kubilius, Alvydas Gleiznys
REVIEWS SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 14: 3-11, 2012 The preservation of alveolar bone ridge during tooth extraction Marius Kubilius, Ricardas Kubilius, Alvydas Gleiznys SUMMARY Objectives. The aims were to overview healing of extraction socket, recommendations for atraumatic tooth extraction, possibilities of post extraction socket bone and soft tissues preservation, augmentation. Materials and Methods. A search was done in Pubmed on key words in English from 1962 to December 2011. Additionally, last decades different scientifi c publications, books from ref- erence list were assessed for appropriate review if relevant. Results and conclusions. There was made intraalveolar and extraalveolar postextractional socket healing overview. There was established the importance and effectiveness of atraumatic tooth extraction and subsequent postextractional socket augmentation in limited hard and soft tissue defects. There are many different methods, techniques, periods, materials in regard to the review. It is diffi cult to compare the data and to give the priority to one. Key words: tooth extraction, grafting, socket, healing, ridge preservation. INTRODUCTION Nowadays tooth extraction becomes more im- portunity to get acknowledge with summarized con- portant in complex odontological treatment. Three temporary scientifi c publication results, methodologies dimensional bones’ and soft tissue parameters infl u- and practical recommendations in preserving alveolar ence further treatment plan, results and long time crest in tooth extraction (validity for atraumatic tooth prognosis. Tooth extraction inevitably has infl uence extraction, operative methods, protection of alveolus in bone resorption and changes in gingival contours. after extractions, feasible post extraction fi llers and Further treatment may become more complex in using complications, alternative treatment). -
List of Recommended Speakers Updated by BOT April 2015
American Academy of Periodontology List of Recommended Speakers Updated by BOT April 2015 The American Academy of Periodontology is committed to advancing the health and well-being of the public through excellence in the practice of periodontics. It has initiated in an effort to promote better care and health for patients by providing expert information on periodontics to members of the dental team. Continuing education program planners are invited to refer to this list when programming speakers for state, regional or national meetings. AAP members with expertise in the topic areas, experience presenting to general practice and dental hygiene audiences, and familiarity with the Academy's vision for the specialty have been included. Speakers are encouraged to address the advantages of a collaborative approach to addressing patients' needs. In this way, dental colleagues will benefit from learning how patient care may be improved, be it in the area of periodontal disease treatment, implant placement, or regenerative and esthetic procedures. Individuals included on the list are under no obligation to accept offers to speak. In addition, it is not the Academy's intent to provide financial support for either travel expenses or honorarium. All scheduling and financial arrangements are made between the individual and the organization extending the invitation to speak. This list is updated annually. The speakers are listed by topic and in alphabetical order. DISCLAIMER: This AAP List of Recommended Speakers has been generated to facilitate contact between groups programming continuing education speakers and potential speakers who are members of the Academy; it is not intended to be all inclusive. -

Aesthetic Enhancement Around Immediate Implant by Soft Tissue Augmentation with Free Gingival Graft: a Case Report Swapnil P
Borkar SP et al.: Soft Tissue Augmentation with Free Gingival Graft CASE REPORT Aesthetic Enhancement around Immediate Implant by Soft Tissue Augmentation with Free Gingival Graft: A Case Report Swapnil P. Borkar1, Surbhi Pandagale2, Girish Bhutada3 Correspondence to: 1-PG student, Department of Periodontology, Swargiya dadasaheb dental college and hospital, Nagpur. 2-Dental surgeon, Swargiya dadasaheb dental college and hospital, Dr. Swapnil P. Borkar, PG student, Department of Periodontology, Nagpur. 3-Professor, Department of Periodontology, Swargiya dadasaheb dental Swargiya dadasaheb dental college and hospital, Nagpur. college and hospital, Nagpur. Contact Us: www.ijohmr.com ABSTRACT Increasing keratinized tissue around immediate implant by soft tissue augmentation with free gingival graft. Immediate implant placement has been advocated as it reduces treatment time, allowing socket healing simultaneously alongwith implant osseointegration. Peri-implant plaque index is increased due to inadequate keratinized tissues. Peri-implant plastic surgery aims at creating adequate peri-implant keratinized tissue for proper oral hygiene maintenance and improving implant aesthetics. A 26 year old male patient reported to the Department of Periodontology complaining of unaesthetic appearance due to fractured permanent maxillary left lateral incisor. Following a thorough periodontal examination, treatment modality chosen was immediate implant placement at the respective site. Six months following implant placement, soft tissue augmentation using -

Free Gingival Autograft for Augmen- Tation of Keratinized Tissue and Stabili- Zation of Gingival Recessions
Journal of IMAB - Annual Proceeding (Scientific Papers) 2008, book 2 FREE GINGIVAL AUTOGRAFT FOR AUGMEN- TATION OF KERATINIZED TISSUE AND STABILI- ZATION OF GINGIVAL RECESSIONS Chr. Popova, Tsv. Boyarova Department of Periodontology Faculty of Dental Medicine, Medical University - Sofia, Bulgaria SUMMARY: formation and periodontal disease can cause progressive Background: The presence of gingival recession loss of attachment and displacement of gingival margin associated with an insufficient amount of keratinized tissue apically reducing vestibular depth. Proper oral hygiene is may indicate gingival augmentation procedure. The most impossible in such cases with minimal vestibular depth and common technique for gingival augmentation procedure is lack of attached gingiva (2, 15). the free gingival autograft. There are several evidences that persons who The aim of this study was to evaluate the changes practice optimal oral hygiene may maintain periodontal in the amount of keratinized tissue and in the position of health with minimal amount of keratinized gingiva (18). gingival margin in sites treated with free gingival autograft However, a number of authors suggest that sufficient apical to the area of Miller’s class I, class II and class III amount of keratinized tissue is considered essential to gingival recessions. preserve the healthy periodontal status and to support the Methods: Twenty three subjects with 56 gingival dentogingival unit more resistant during the masticatory recessions associated with an insufficient amount of function and oral hygiene procedure (9). Therefore the keratinized gingiva were treated with gingival augmentation presence of gingival recession associated with a minimal procedure (free gingival graft). The grafts were positioned amount or lack of keratinized gingiva may indicate need of apical to the area of recession at the level of mucogingival gingival augmentation procedure to prevent additional junction. -

The Art and Science of Shade Matching in Esthetic Implant Dentistry, 275 Chapter 12 Treatment Complications in the Esthetic Zone, 301
FUNDAMENTALS OF ESTHETIC IMPLANT DENTISTRY Abd El Salam El Askary FUNDAMENTALS OF ESTHETIC IMPLANT DENTISTRY FUNDAMENTALS OF ESTHETIC IMPLANT DENTISTRY Abd El Salam El Askary Dr. Abd El Salam El Askary maintains a private practice special- Set in 9.5/12.5 pt Palatino izing in esthetic dentistry in his native Egypt. An experienced cli- by SNP Best-set Typesetter Ltd., Hong Kong nician and researcher, he is also very active on the international Printed and bound by C.O.S. Printers Pte. Ltd. conference circuit and as a lecturer on continuing professional development courses. He also holds the position of Associate For further information on Clinical Professor at the University of Florida, Jacksonville. Blackwell Publishing, visit our website: www.blackwellpublishing.com © 2007 by Blackwell Munksgaard, a Blackwell Publishing Company Disclaimer The contents of this work are intended to further general scientific Editorial Offices: research, understanding, and discussion only and are not intended Blackwell Publishing Professional, and should not be relied upon as recommending or promoting a 2121 State Avenue, Ames, Iowa 50014-8300, USA specific method, diagnosis, or treatment by practitioners for any Tel: +1 515 292 0140 particular patient. The publisher and the editor make no represen- 9600 Garsington Road, Oxford OX4 2DQ tations or warranties with respect to the accuracy or completeness Tel: 01865 776868 of the contents of this work and specifically disclaim all warranties, Blackwell Publishing Asia Pty Ltd, including without limitation any implied -

Case Report Morphological and Molecular Characterization of Human Gingival Tissue Overlying Multiple Oral Exostoses
Hindawi Case Reports in Dentistry Volume 2019, Article ID 3231759, 10 pages https://doi.org/10.1155/2019/3231759 Case Report Morphological and Molecular Characterization of Human Gingival Tissue Overlying Multiple Oral Exostoses Luca Francetti ,1,2 Claudia Dellavia ,1 Stefano Corbella ,1,2 Nicolò Cavalli ,1,2 Claudia Moscheni ,3 Elena Canciani ,1 and Nicoletta Gagliano 4 1Department of Biomedical, Surgical and Dental Sciences, Università degli Studi di Milano, via L. Mangiagalli 31, 20133 Milan, Italy 2IRCCS Istituto Ortopedico Galeazzi, Via R. Galeazzi, 4, 20161 Milan, Italy 3Department of Biomedical and Clinical Sciences “L. Sacco”, Università degli Studi di Milano, via G.B. Grassi 74, 20157 Milan, Italy 4Department of Biomedical Sciences for Health, Università degli Studi di Milano, via L. Mangiagalli 31, 20133 Milan, Italy Correspondence should be addressed to Nicoletta Gagliano; [email protected] Received 6 September 2018; Accepted 10 May 2019; Published 22 May 2019 Academic Editor: Jamil Awad Shibli Copyright © 2019 Luca Francetti et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Gingival and osseous augmentations are reported as hypertrophic or hyperplastic reactions to different factors including chronic traumatisms and surgeries such as free gingival graft (FGG) that induce an abnormal growth of both hard and soft tissues in genetically predisposed subjects. Since an imbalance in collagen turnover plays a key role in the development of gingival overgrowth leading to an accumulation of collagen in gingival connective tissue, in this study we described the histological and molecular features of three oral overgrowths obtained from a 34-year-old woman previously operated for FGG in order to evaluate a possible relationship between exostoses and overgrown tissue. -
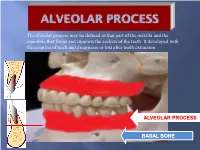
Alveolar Process May Be Defined As That Part of the Maxilla and the Mandible That Forms and Supports the Sockets of the Teeth
The alveolar process may be defined as that part of the maxilla and the mandible that forms and supports the sockets of the teeth. It developed with the eruption of teeth and disappears or lost after tooth extraction ALVEOLAR PROCESS BASAL BONE Alveolar (bone) process: is that part of the maxilla and the mandible that forms and supports the sockets of the teeth. Basal Bone. it is the bone of the facial skeleton which support the alveolar bone. There is no anatomical boundary between basal bones and alveolar bone. Both alveolar process and basal bone are covered by the same periosteum. In some areas alveolar processes may fuse or masked with jaw bones as in (1) Anterior part of maxilla (palatal). (2) Oblique line of the mandible. * Alveolar process is resorbed after extraction of teeth. Functions of alveolar bone – Houses and protects developing permanent teeth, while supporting primary teeth. – Organizes eruption of primary and permanent teeth. – Anchors the roots of teeth to the alveoli, which is achieved by the insertion of Sharpey’s fibers into the alveolar bone proper (attachment). – Helps to move the teeth for better occlusion (support). – Helps to absorb and distribute occlusal forces generated during tooth contact (shock absorber). – Supplies vessels to periodontal ligament. •DEVELOPMENT OF ALVEOLAR BONE •Near the end of the second month of fetal life, the maxilla as well as the mandible form a groove that is open towards the surface of the oral cavity. •Tooth germs develop within the bony structures at late bell stage. •Bony septa and bony bridge begin to form and separatethe individual tooth germs from one another, keeping individual tooth germs in clearly outlined bony compartments. -

The Internohonol Journal Ot Perjodonhcs £ Restorative Denlisi 289
288 The InternoHonol Journal ot PerJodonhcs £ Restorative DenlisI 289 Effect of Calculus and Abstract The role of supragingivol irrigotion in Irrigator Tip Design on the treatment of gingivitis is clear'"^; Depth of Subgingival This study oddressed three foctors however, the ability of subgingivol ir- Irrigation thot moy affect the penetratian af rigation ta improve the periadontal medicaments inta periadontol pock- stotus of patients with periodontitis re- ets: calculus, ejection site pressure, mains cantroversial.^"* Theoretically, ond irrigatar tip design. Ejection site delivery of antimicrobial solutions to pressure far the Mox-i-Probe, the suppress putotive periodontal path- Ytadent ond Water-Pik tips were de- ogens could represent a supplemen- termined with a variant of Bernoullis' tal procedure to enhance mechoni- equation. Depth of irrigont penetra- cal instrumentation. However, the fol- tion was determined by delivering lowing principles must be considered disclosing salutian supragingivotly before irTigction theropy is integrated ond subgingivolly. Following irriga- into treotment regimens: ¡1) drugs tion, assessed teeth were extracted must be delivered to the site of dis- and the percentage af packet pen- ease activity, ¡2} ontibocterial solu- Jeffrey R. Larner, DDS, MS' etratian by the dye was calculated. tions must be used ot bactericidal Gary Greenstein, DDS, M5' The Max-I-Probe and Viodent tips concentrotions, ond ¡31 medicaments had significantly greoter penetration than did the Water-File tip. Further- must be present long enough to more, calculus deposits reduced irri- work.' The latter two foctors can be gation penetration in deep pockets regulated by adjusting drug concen- (7 ta W mm¡. Ejection site pressures trations, selecting substantive medi- af the three tips ronged fram 0.10 to caments, ond odministering irrigotion 4.80 psi.