Splinting and Occlusal Correction Questions and Answers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alveolar Ridge Preservation at Different Anatomical Locations
ALVEOLAR RIDGE PRESERVATION AT DIFFERENT ANATOMICAL LOCATIONS- CLINICAL AND HISTOLOGICAL EVALUATION OF TREATMENT OUTCOME MASTERS THESIS Presented in Partial Fulfillment of Requirements for the Degree Master of Science in Dentistry in the Graduate School of The Ohio State University By Mabel Salas, DDS Graduate Program in Dentistry The Ohio State University 2009 Master’s Examination Committee: Binnaz Leblebicioglu, DDS, MS, PhD, Advisor Dimitris N. Tatakis, DDS, PhD Suda Agarwal, PhD Do-Gyoon Kim, PhD Copyright by Mabel Salas 2009 ABSTRACT Background: Alveolar ridge preservation (ARP) is a surgical technique designed to prevent naturally occurring post-extraction bone resorption. It is well documented that alveolar bone height and width are reduced following tooth extraction as a result of physiologic bone remodeling. Depending on the type of post-extraction intrabony defect, an immediate or early implant placement itself may preserve the bone height and width. However, if the defect is generally too wide for immediate and/or early implant placement, it is recommended to perform ARP surgery to preserve the bone volume for future implant placement. The purpose of this study was to investigate clinical and histological healing outcomes following ARP performed on molar and premolar sites by using freeze-dried bone allograft (FDBA) together with a collagen membrane. Maxillary and mandibular sextants were compared for clinical and histological parameters. Methods: Patients who were scheduled to have tooth extraction and implant placement for a molar or premolar tooth were included into this study. Inclusion criteria were single tooth extraction with intact mesial and distal adjacent teeth. Exclusion criteria were smokers, systemic health problems that may affect wound healing and acute infection ii that may prevent bone graft placement. -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Periodontal Ligament, Cementum, and Alveolar Bone in the Oldest Herbivorous Tetrapods, and Their Evolutionary Significance
Periodontal Ligament, Cementum, and Alveolar Bone in the Oldest Herbivorous Tetrapods, and Their Evolutionary Significance Aaron R. H. LeBlanc*, Robert R. Reisz Department of Biology, University of Toronto Mississauga, Mississauga, Ontario, Canada Abstract Tooth implantation provides important phylogenetic and functional information about the dentitions of amniotes. Traditionally, only mammals and crocodilians have been considered truly thecodont, because their tooth roots are coated in layers of cementum for anchorage of the periodontal ligament, which is in turn attached to the bone lining the alveolus, the alveolar bone. The histological properties and developmental origins of these three periodontal tissues have been studied extensively in mammals and crocodilians, but the identities of the periodontal tissues in other amniotes remain poorly studied. Early work on dental histology of basal amniotes concluded that most possess a simplified tooth attachment in which the tooth root is ankylosed to a pedestal composed of ‘‘bone of attachment’’, which is in turn fused to the jaw. More recent studies have concluded that stereotypically thecodont tissues are also present in non-mammalian, non-crocodilian amniotes, but these studies were limited to crown groups or secondarily aquatic reptiles. As the sister group to Amniota, and the first tetrapods to exhibit dental occlusion, diadectids are the ideal candidates for studies of dental evolution among terrestrial vertebrates because they can be used to test hypotheses of development and homology in deep time. Our study of Permo-Carboniferous diadectid tetrapod teeth and dental tissues reveal the presence of two types of cementum, periodontal ligament, and alveolar bone, and therefore the earliest record of true thecodonty in a tetrapod. -

The Preservation of Alveolar Bone Ridge During Tooth Extraction Marius Kubilius, Ricardas Kubilius, Alvydas Gleiznys
REVIEWS SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 14: 3-11, 2012 The preservation of alveolar bone ridge during tooth extraction Marius Kubilius, Ricardas Kubilius, Alvydas Gleiznys SUMMARY Objectives. The aims were to overview healing of extraction socket, recommendations for atraumatic tooth extraction, possibilities of post extraction socket bone and soft tissues preservation, augmentation. Materials and Methods. A search was done in Pubmed on key words in English from 1962 to December 2011. Additionally, last decades different scientifi c publications, books from ref- erence list were assessed for appropriate review if relevant. Results and conclusions. There was made intraalveolar and extraalveolar postextractional socket healing overview. There was established the importance and effectiveness of atraumatic tooth extraction and subsequent postextractional socket augmentation in limited hard and soft tissue defects. There are many different methods, techniques, periods, materials in regard to the review. It is diffi cult to compare the data and to give the priority to one. Key words: tooth extraction, grafting, socket, healing, ridge preservation. INTRODUCTION Nowadays tooth extraction becomes more im- portunity to get acknowledge with summarized con- portant in complex odontological treatment. Three temporary scientifi c publication results, methodologies dimensional bones’ and soft tissue parameters infl u- and practical recommendations in preserving alveolar ence further treatment plan, results and long time crest in tooth extraction (validity for atraumatic tooth prognosis. Tooth extraction inevitably has infl uence extraction, operative methods, protection of alveolus in bone resorption and changes in gingival contours. after extractions, feasible post extraction fi llers and Further treatment may become more complex in using complications, alternative treatment). -

Restoration of the Periodontally Compromised Dentition
Restoration of the 27 Periodontally Compromised Dentition Arnold S. Weisgold and Neil L. Starr NATURAL DENTITION DENTAL THERAPEUTICS: WITHOUT IMPLANTS IMPACT OF ESTHETICS DENTAL THERAPEUTICS: WITH IMPLANTS Outcome-Based Planning PERIODONTAL BIOTYPES Considerations at the Surgical Phase Transitional Implant-Assisted Restoration ROLE OF OCCLUSION Final Prosthetic Phase of Treatment Long-Term Maintenance/Professional Care TREATMENT PLANNING AND TREATMENT SEQUENCING WITH AND WITHOUT ENDOSSEOUS CONCLUSION IMPLANTS: A COMPREHENSIVE THERAPEUTIC APPROACH TO THE PARTIALLY EDENTULOUS PATIENT Diagnostic Evaluation Esthetic Treatment Approach Portions of this chapter are from Starr NL: Treatment planning and treatment sequencing with and without endosseous implants: a comprehensive therapeutic approach to the partially edentulous patient, Seattle Study Club Journal 1:1, 21-34, 1995. Chapter 27 Restoration of the Periodontally Compromised Dentition 677 !""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""""#$ The term periodontal prosthesis1,2 was coined by Amsterdam when it is achieved in concert with all the functional about 50 years ago. He defined periodontal prostheses needs of the dentition. as “those restorative and prosthetic endeavors that are absolutely essential in the treatment of advanced perio- PERIODONTAL BIOTYPES dontal disease.” New, more sophisticated techniques are currently available, and with the advent of endosseous Ochsenbein and Ross,15 Weisgold,16 and Olsson and implants3 -

Gingival Stillman's Cleft- Revisited Review Article
Review Article Gingival Stillman’s Cleft- Revisited Deepa D1 , Gouri Bhatia2, Priyanka Srivastava3 Professor1, Senior Lecturer2 , Private Practitioner 3 1-2 Department of Periodontology, Subharti Dental College and Hospital, Haridwar By-pass road, Meerut-250005, U.P, India, Delhi Abstract: Stillman’s clefts are apostrophe shaped indentations extending from and into the gingival margin for varying distances. The etiology of this cleft is still not clear. They may repair spontaneously or persist as surface lesions of deep periodontal pockets that penetrate into the supporting tissues. Here we report a case of stillman’s cleft in the mandibular left lateral incisor region treated with de-epithelialisation. Keywords: Stillman’s cleft, inflammatory, occlusal trauma, developmental, gingival clefts, simple clefts. Introduction Stillman’s cleft is a term used to describe a specific type trauma. Stillman’s cleft was seen in relation to of gingival recession consisting of a narrow mandibular left lateral incisor on the labial aspect triangular-shaped gingival recession. As the recession extending from marginal gingiva towards the progresses apically, the cleft becomes broader, exposing muco-gingival junction. Radiographic examination the cementum of the root surface. When the lesion revealed no evidence of bone loss #32. Scaling and root reaches the mucogingival junction, the apical border of planing was performed and during re-evaluation of Phase oral mucosa is usually inflamed because of the difficulty I, Stillman’s cleft still persisted. Gingival -

The Influence of Controlled Occlusal Overload on Peri-Implant Tissue. Part 3: a Histologic Study in Monkeys
The Influence of Controlled Occlusal Overload on Peri-implant Tissue. Part 3: A Histologic Study in Monkeys Takashi Miyata, DDS, DDSc1/Yukinao Kobayashi, DDS2/Hisao Araki, DDS, DDSc3/ Takaichi Ohto, DDS4/Kitetsu Shin, DDS, DDSc5 The influence of experimental occlusal overload on peri-implantitis in monkeys (Macaca fascicu- laris) has been examined to explain the pathology of the disease that develops in the tissue around osseointegrated implants. In the first article of this series, it was reported that bone resorption was not observed around implants when occlusal trauma was produced by a super- structure that was in supraocclusal contact with an excess occlusal height of approximately 100 µm, provided there was no inflammation in the peri-implant tissue. In the second part of the study, experimental inflammation was created in the peri-implant tissue, and occlusal overload was produced by a superstructure with an excess occlusal height of 100 µm. Notable bone resorption was observed around the implant with the passage of time. These results suggested that, in addition to the control of inflammation in peri-implant tissue, traumatic occlusion may play a role in bone breakdown around the implant. In the present study, while the peri-implant tis- sue was kept in an inflammation-free state, bone level changes around the implants were investi- gated when various levels of traumatic force were exerted. The supraoccluding prostheses were defined as excessively high by 100 µm, 180 µm, and 250 µm, respectively. The heights were determined with an image analysis device, and the bone responses around the implants induced by the traumatic forces were investigated. -

October 2000
cda journal, vol 28, nº 10 CDA Journal Volume 28, Number 10 Journal october 2000 departments 727 The Editor/Achieving Consensus 733 Impressions/Building the Multi-Generation Dental Team 812 Dr. Bob/A Breath of Fresh Air features 745 CURRENT ISSUES IN OCCLUSION An introduction to the issue. By Donald A. Curtis, DMD, and Richard T. Kao, DDS, PhD 748 OCCLUSION: WHAT IT IS AND WHAT IT IS NOT Management of the occlusion is directly correlated to the successful treatment and maintenance of the teeth, but it has not been scientifically proven that it is directly correlated to the musculoskeletal disorders that affect the jaw. By Charles McNeill, DDS 760 OCCLUSAL CONSIDERATIONS IN DETERMINING TREATMENT PROGNOSIS Occlusion influences the prognosis of individual teeth and the overall treatment prognosis. By Richard T. Kao, DDS, PhD; Raymond Chu, DDS; and Donald A. Curtis, DMD 771 OCCLUSAL CONSIDERATIONS FOR IMPLANT RESTORATIONS IN THE PARTIALLY EDENTULOUS PATIENT Appropriate occlusal considerations can decrease restorative complications. By Donald A. Curtis, DMD, Arun Sharma, BDS, MS; Fredrick C. Finzen, DDS; and Richard T. Kao, DDS, PhD 780 OCCLUSION: AN ORTHODONTIC PERSPECTIVE Excellent static occlusal and functional goals are critical elements in the long-term stability of orthodontic treatment. By Paul M. Kasrovi, DDS, MS; Michael Meyer, DDS; Gerald D. Nelson, DDS 792 A PRACTICAL GUIDE TO OCCLUSAL MANAGEMENT FOR THE GENERAL PRACTITIONER An classification system outlined in this article can assist the general dentist in the diagnosis, treatment planning, and management of problems associated with the stomatognathic system. By Gordon D. Douglass, DDS, MS; Larry Jenson, DDS; and Daniel Mendoza, DDS head Editor cda journal, vol 28, n 10 º Achieving Consensus Jack F. -

The Influence of Primary Occlusal Trauma on the Development of Gingival Recession Revista Clínica De Periodoncia, Implantología Y Rehabilitación Oral, Vol
Revista Clínica de Periodoncia, Implantología y Rehabilitación Oral ISSN: 0718-5391 [email protected] Sociedad de Periodoncia de Chile Chile Lindoso Gomes Campos, Mirella; Tomazi, Patrícia; Távora de Albuquerque Lopes, Ana Cristina; Quartaroli Téo, Mirela Anne; Machado da Silva, Joyce Karla; Colombini Ishikiriama, Bella Luna; dos Santos, Pâmela Letícia The influence of primary occlusal trauma on the development of gingival recession Revista Clínica de Periodoncia, Implantología y Rehabilitación Oral, vol. 9, núm. 3, diciembre, 2016, pp. 271-276 Sociedad de Periodoncia de Chile Santiago, Chile Available in: http://www.redalyc.org/articulo.oa?id=331049327010 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Documento descargado de http://www.elsevier.es el 13-01-2017 Rev Clin Periodoncia Implantol Rehabil Oral. 2016;9(3):271---276 Revista Clínica de Periodoncia, Implantología y Rehabilitación Oral www.elsevier.es/piro ORIGINAL ARTICLE The influence of primary occlusal trauma on the development of gingival recession a,∗ b Mirella Lindoso Gomes Campos , Patrícia Tomazi , c c Ana Cristina Távora de Albuquerque Lopes , Mirela Anne Quartaroli Téo , d e Joyce Karla Machado da Silva , Bella Luna Colombini Ishikiriama , f Pâmela Letícia dos Santos a Ph.D. in Periodontics, Docent and Researcher of the Post-Graduation Course in Oral Biology, Area of Oral Biology, Universidade Sagrado Corac¸ão, USC, Brazil b Graduate Student in Dentistry in Univeridade do Sagrado Corac¸ão, Bauru, SP, Brazil c M.Sc. -
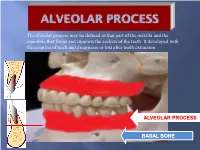
Alveolar Process May Be Defined As That Part of the Maxilla and the Mandible That Forms and Supports the Sockets of the Teeth
The alveolar process may be defined as that part of the maxilla and the mandible that forms and supports the sockets of the teeth. It developed with the eruption of teeth and disappears or lost after tooth extraction ALVEOLAR PROCESS BASAL BONE Alveolar (bone) process: is that part of the maxilla and the mandible that forms and supports the sockets of the teeth. Basal Bone. it is the bone of the facial skeleton which support the alveolar bone. There is no anatomical boundary between basal bones and alveolar bone. Both alveolar process and basal bone are covered by the same periosteum. In some areas alveolar processes may fuse or masked with jaw bones as in (1) Anterior part of maxilla (palatal). (2) Oblique line of the mandible. * Alveolar process is resorbed after extraction of teeth. Functions of alveolar bone – Houses and protects developing permanent teeth, while supporting primary teeth. – Organizes eruption of primary and permanent teeth. – Anchors the roots of teeth to the alveoli, which is achieved by the insertion of Sharpey’s fibers into the alveolar bone proper (attachment). – Helps to move the teeth for better occlusion (support). – Helps to absorb and distribute occlusal forces generated during tooth contact (shock absorber). – Supplies vessels to periodontal ligament. •DEVELOPMENT OF ALVEOLAR BONE •Near the end of the second month of fetal life, the maxilla as well as the mandible form a groove that is open towards the surface of the oral cavity. •Tooth germs develop within the bony structures at late bell stage. •Bony septa and bony bridge begin to form and separatethe individual tooth germs from one another, keeping individual tooth germs in clearly outlined bony compartments. -

Chronic Periodontitis Exacerbated by Occlusal Trauma: Report of a Case and Revision of Literature Ma
tist Den ry Dentistry Rodriguez et al., Dentistry 2017, 7:5 ISSN: 2161-1122 DOI: 10.4172/2161-1122.1000426 Review Article Open Access Chronic Periodontitis Exacerbated by Occlusal Trauma: Report of A Case and Revision of Literature Ma. Lourdes Rodriguez1,2*, Iturralde M3, Vega J3 and Pinos X3 1Chair of Semiology and Clinical Diagnosis, University of Cuenca, Ecuador 2Institute of Microbiology, Parasitology and Immunology, Faculty of Medicine, University of Buenos Aires, Argentina 3Faculty of Dentistry, University of Cuenca, Ecuador *Corresponding author: Ma. Lourdes Rodriguez, Professor, Chair of Semiology and Clinical Diagnosis, Faculty of Dentistry, University of Cuenca, Ecuador, Tel: 5932933554; E-mail: [email protected] Received date: March 16, 2017; Accepted date: April 4, 2017; Published date: April 11, 2017 Copyright: © 2017 Rodriguez L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Occlusal trauma has been associated with periodontal disease 100 years ago, but only observationally. Since the 1930s, the effect of excessive occlusal forces on the periodontium has been evaluated at the pre-clinical level. At first, studies on animal and human autopsy material showed no association between occlusal discrepancies and periodontal destruction. However, in the last 10 years new evidence has emerged that today allows us to establish a relationship between both clinical entities. The latest review on the subject published in 2015, states that at the moment there is a lack of strong evidence to assume a relation of cause/effect between periodontitis and excessive occlusal forces. -

Evaluation of Clinical Effects of Occlusal
Romanian Journal of Oral Rehabilitation Vol. 7, No. 3, July - September 2015 EVALUATION OF CLINICAL EFFECTS OF OCCLUSAL TRAUMA ON GINGIVAL RECESSION Mihaela Moisei1, Cosmin Popa2, Ioana Rudnic*2, Dana Popa2, Amelia Surdu2, Nicoleta Ioanid2,Lucian Burlea2, Silvia Martu2 1“Dunarea de Jos” University - Galați, Romania, Faculty of Dentistry 2“Gr. T. Popa" U.M.Ph. - Iași, Romania, Faculty of Dentistry *Corresponding author: Ioana Rudnic, MD, PhD “Gr. T. Popa" University of Medicine and Pharmacy - Iași, Romania e-mail: ioana_rudnic@ yahoo.com ABSTRACT Aim of the study The aim of this study was to investigate the occlusal contacts during maximum intercuspation to protrusive, lateroprotrusive and lateral excursive movements and their effects on gingival recession. Material and methods Fourteen subjects having gingival recession aged by 18–53 years old were selected, examined about the location and extent of gingival recession and occlusal wear facets were recorded. The type of occlusion and the nature of occlusal contact in maximum intercuspation and eccentric mandibular movements were also recorded using articulating foil. Results Our results indicated that gingival recession was more frequent in patients with occlusal function group than at patients with occlusal canine protection. At patients with occlusal canine protection gingival recession was located on the labial surface while at patients with function group recession was equally distributed on vestibular surface of the teeth in the anterior and posterior areas. Almost all patients with interference in protrusive, lateroprotrusive movements had teeth with gingival recession. Also abrasion was observed in most teeth with gingival recession. Conclusions These results suggest that occlusal interferences in maximum intercuspation and eccentric movements in one form or the other and absence of mutually protected occlusion can contribute to gingival lesions such as gingival recessions.