Flint Rash Investigation Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Science Inside Skin
the science inside SKIN AMERICAN ASSOCIATION FOR THE ADVANCEMENT OF SCIENCE Dear Reader: Science data and statistics are always changing, and it is important to be informed of current research. To help keep you up-to-date with the latest information on skin health, the American Association for the Advancement of Science would like to share the following updates regarding skin health: N Major medical groups, including the CDC, recommend using sun- screen with an SPF of 15 or higher. However, a growing number of health care providers, including the M.D. Anderson Cancer Center, suggest products of SPF 30 or higher, particularly for those whose skin burns easily. (See references on pages 17, 32, and 45.) N The number of doctor visits Americans make each year to get skin rashes checked out has dropped from 11.8 million to 10 million, according to the National Ambulatory Medical Care Survey: 2006 Summary, National Health Statistics Report No. 3. (See reference on page 23.) http://www.cdc.gov/nchs/data/nhsr/nhsr003.pdf is the most recent data. Check the site for regular updates to the statistics. N According to the CDC’s National Program of Cancer Registries, 53,792 new cases of melanoma were reported in 2005, the most recent year for which statistics were available in Summer 2009. The National Cancer Institute estimates that 68,720 new cases will be diagnosed in 2009. (See reference on page 36.) N Estimates vary as to the likelihood of developing melanoma during the average American’s lifetime. MedlinePlus, developed by the National Institutes of Health, estimates that 1 in 65 people will be diagnosed with melanoma at some point in their life. -
The Garment of Adam in Jewish, Muslim, and Christian Tradition
24 The Garmentof Adam in Jewish, Muslim, and ChristianTradition Stephen D. Ricks Although rarely occurring in any detail, the motif of Adam's garment appears with surprising frequency in ancient Jewish and Christian literature. (I am using the term "Adam's garment" as a cover term to include any garment bestowed by a divine being to one of the patri archs that is preserved and passed on, in many instances, from one generation to another. I will thus also consider garments divinely granted to other patriarchal figures, including Noah, Abraham, and Joseph.) Although attested less often than in the Jewish and Christian sources, the motif also occurs in the literature of early Islam, espe cially in the Isra'iliyyiit literature in the Muslim authors al ThaclabI and al-Kisa'I as well as in the Rasii'il Ikhwiin al ~afa (Epistles of the Brethren of Purity). Particularly when discussing the garment of Adam in the Jewish tradition, I will shatter chronological boundaries, ranging from the biblical, pseudepigraphic, and midrashic references to the garment of Adam to its medieval attestations. 1 In what fol lows, I wish to consider (1) the garment of Adam as a pri mordial creation; (2) the garment as a locus of power, a symbol of authority, and a high priestly garb; and (3) the garment of Adam and heavenly robes. 2 705 706 STEPHEN D. RICKS 1. The Garment of Adam as a Primordial Creation The traditions of Adam's garment in the Hebrew Bible begin quite sparely, with a single verse in Genesis 3:21, where we are informed that "God made garments of skins for Adam and for his wife and clothed them." Probably the oldest rabbinic traditions include the view that God gave garments to Adam and Eve before the Fall but that these were not garments of skin (Hebrew 'or) but instead gar ments of light (Hebrew 'or). -

FIG. 4A © O O Wo 2015/042110 Al III III II II III III 1 1 II III II II III III II III
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date W O 2015/042110 A l 2 6 March 2015 (26.03.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61P 37/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 14/056021 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, ΓΝ , IR, IS, JP, KE, KG, KN, KP, KR, 17 September 2014 (17.09.2014) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/880,522 20 September 2013 (20.09.2013) (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: CHILDREN'S MEDICAL CENTER COR¬ GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, PORATION [US/US]; 55 Shattuck Street, Boston, Mas¬ TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, sachusetts 021 15 (US). -

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -

Cutaneous Manifestations of HIV Infection Carrie L
Chapter Title Cutaneous Manifestations of HIV Infection Carrie L. Kovarik, MD Addy Kekitiinwa, MB, ChB Heidi Schwarzwald, MD, MPH Objectives Table 1. Cutaneous manifestations of HIV 1. Review the most common cutaneous Cause Manifestations manifestations of human immunodeficiency Neoplasia Kaposi sarcoma virus (HIV) infection. Lymphoma 2. Describe the methods of diagnosis and treatment Squamous cell carcinoma for each cutaneous disease. Infectious Herpes zoster Herpes simplex virus infections Superficial fungal infections Key Points Angular cheilitis 1. Cutaneous lesions are often the first Chancroid manifestation of HIV noted by patients and Cryptococcus Histoplasmosis health professionals. Human papillomavirus (verruca vulgaris, 2. Cutaneous lesions occur frequently in both adults verruca plana, condyloma) and children infected with HIV. Impetigo 3. Diagnosis of several mucocutaneous diseases Lymphogranuloma venereum in the setting of HIV will allow appropriate Molluscum contagiosum treatment and prevention of complications. Syphilis Furunculosis 4. Prompt diagnosis and treatment of cutaneous Folliculitis manifestations can prevent complications and Pyomyositis improve quality of life for HIV-infected persons. Other Pruritic papular eruption Seborrheic dermatitis Overview Drug eruption Vasculitis Many people with human immunodeficiency virus Psoriasis (HIV) infection develop cutaneous lesions. The risk of Hyperpigmentation developing cutaneous manifestations increases with Photodermatitis disease progression. As immunosuppression increases, Atopic Dermatitis patients may develop multiple skin diseases at once, Hair changes atypical-appearing skin lesions, or diseases that are refractory to standard treatment. Skin conditions that have been associated with HIV infection are listed in Clinical staging is useful in the initial assessment of a Table 1. patient, at the time the patient enters into long-term HIV care, and for monitoring a patient’s disease progression. -

Chronic Paronychia Refers to a Skin Condition, Which Occurs Around the Nails
Robert E. Kalb, M.D. Buffalo Medical Group, P.C. Phone: (716) 630-1102 Fax: (716) 633-6507 Department of Dermatology 325 Essjay Road Williamsville, New York 14221 PARONYCHIA (CHRONIC) Chronic paronychia refers to a skin condition, which occurs around the nails. The term chronic means that the condition can come and go over time. The word paronychia is a fancy medical term referring to the inflammation, redness and swelling that can occur around the nails. Chronic paronychia occurs most commonly in people whose hands are in a wet environment, for example nurses, bartenders, dishwashers and hairdressers. Repeated cuts and minor trauma of the skin can damage the area around the nail and in the cuticle. This minor damage allows further irritation. There can be overgrowth of various surface germs, which slow the healing process. Symptoms of chronic paronychia include loss of the cuticle, tenderness, redness and swelling. Often the nails can appear changed with rough surfaces or grooves. Sometimes the area around the nail can be colonized with a normal bacteria or yeast on the skin. Because of this, one of the treatments that is often used is a medication, which has antibiotic properties against these types of organisms. In many cases, it is not an actual infection, but simply colonization on the surface of the skin, which impedes the healing. Treatment of chronic paronychia starts by avoiding any chronic irritation or wet environments. Wearing cotton-lined gloves to wash dishes can be helpful if this is an exposure. In most cases, topical medications are used. These often involve two different creams or two different liquids. -
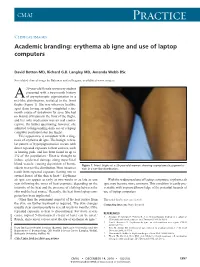
Erythema Ab Igne and Use of Laptop Computers
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Cutaneous Adverse Effects of Biologic Medications
REVIEW CME MOC Selena R. Pasadyn, BA Daniel Knabel, MD Anthony P. Fernandez, MD, PhD Christine B. Warren, MD, MS Cleveland Clinic Lerner College Department of Pathology Co-Medical Director of Continuing Medical Education; Department of Dermatology, Cleveland Clinic; of Medicine of Case Western and Department of Dermatology, W.D. Steck Chair of Clinical Dermatology; Director of Clinical Assistant Professor, Cleveland Clinic Reserve University, Cleveland, OH Cleveland Clinic Medical and Inpatient Dermatology; Departments of Lerner College of Medicine of Case Western Dermatology and Pathology, Cleveland Clinic; Assistant Reserve University, Cleveland, OH Clinical Professor, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH Cutaneous adverse effects of biologic medications ABSTRACT iologic therapy encompasses an expo- B nentially expanding arena of medicine. Biologic therapies have become widely used but often As the name implies, biologic therapies are de- cause cutaneous adverse effects. The authors discuss the rived from living organisms and consist largely cutaneous adverse effects of tumor necrosis factor (TNF) of proteins, sugars, and nucleic acids. A clas- alpha inhibitors, epidermal growth factor receptor (EGFR) sic example of an early biologic medication is inhibitors, small-molecule tyrosine kinase inhibitors insulin. These therapies have revolutionized (TKIs), and cell surface-targeted monoclonal antibodies, medicine and offer targeted therapy for an including how to manage these reactions -

2U11/13U195 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ n n 20 October 2011 (20.10.2011) 2U11/13U195 Al (51) International Patent Classification: ka Pharmaceutical Co., Ltd., 1-7-1, Dosho-machi, Chuo- C12P 19/34 (2006.01) C07H 21/04 (2006.01) ku, Osaka-shi, Osaka 541-0045 (JP). (21) International Application Number: (74) Agents: KELLOGG, Rosemary et al; Swanson & PCT/US201 1/032017 Bratschun, L.L.C., 8210 SouthPark Terrace, Littleton, Colorado 80120 (US). (22) International Filing Date: 12 April 201 1 (12.04.201 1) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, English (25) Filing Language: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (26) Publication Language: English CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (30) Priority Data: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 61/323,145 12 April 2010 (12.04.2010) US KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (71) Applicants (for all designated States except US): SOMA- ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, LOGIC, INC. [US/US]; 2945 Wilderness Place, Boulder, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, Colorado 80301 (US). OTSUKA PHARMACEUTI¬ SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, CAL CO., LTD. -

Concurrent Beau Lines, Onychomadesis, and Retronychia Following Scurvy
CASE REPORT Concurrent Beau Lines, Onychomadesis, and Retronychia Following Scurvy Dayoung Ko, BS; Shari R. Lipner, MD, PhD the proximal nail plate from the distal nail plate leading to shedding of the nail. It occurs due to a complete growth PRACTICE POINTS arrest in the nail matrix and is thought to be on a con- • Beau lines, onychomadesis, and retronychia are nail tinuum with Beau lines. The etiologies of these 2 condi- conditions with distinct clinical findings. tions overlap and include trauma, inflammatory diseases, • Beau lines and onychomadesis may be seen 1-5 concurrently following trauma, inflammatory dis- systemic illnesses, hereditary conditions, and infections. eases, systemic illnesses, hereditary conditions, In almost all cases of both conditions, normal nail plate and infections. production ensues upon identification and removal of the 3,4,6 • Retronychia shares a common pathophysiology inciting agent or recuperation from the causal illness. with Beau lines and onychomadesis, and all reflect Beau lines will move distally as the nail grows out and slowing or cessation of nail plate production. can be clipped. In onychomadesis, the affected nails will be shed with time. Resolution of these nail defects can be estimated from average nail growth rates (1 mm/mo for fingernails and 2–3 mm/mo for toenails).7 Beau lines, onychomadesis, and retronychia are nail conditions with Retronychia is defined as a proximal ingrowing of their own characteristic clinical findings. It has been hypothesized the nail plate into the ventral surface of the proximal nail that these 3 disorders may share a common pathophysiologic fold.4,6 It is thought to occur via vertical progression of mechanism of slowing and/or halting nail plate production at the the nail plate into the proximal nail fold, repetitive nail nail matrix. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Abscesses Are a Serious Problem for People Who Shoot Drugs
Where to Get Your Abscess Seen Abscesses are a serious problem for people who shoot drugs. But what the hell are they and where can you go for care? What are abscesses? Abscesses are pockets of bacteria and pus underneath you skin and occasionally in your muscle. Your body creates a wall around the bacteria in order to keep the bacteria from infecting your whole body. Another name for an abscess is a “soft tissues infection”. What are bacteria? Bacteria are microscopic organisms. Bacteria are everywhere in our environment and a few kinds cause infections and disease. The main bacteria that cause abscesses are: staphylococcus (staff-lo-coc-us) aureus (or-e-us). How can you tell when you have an abscess? Because they are pockets of infection abscesses cause swollen lumps under the skin which are often red (or in darker skinned people darker than the surrounding skin) warm to the touch and painful (often VERY painful). What is the worst thing that can happen? The worst thing that can happen with abscesses is that they can burst under your skin and cause a general infection of your whole body or blood. An all over bacterial infection can kill you. Another super bad thing that can happen is a endocarditis, which is an infection of the lining of your heart, and “septic embolism”, which means that a lump of the contaminates in your abscess get loose in your body and lodge in your lungs or brain. Why do abscesses happen? Abscesses are caused when bad bacteria come in to contact with healthy flesh.