Cardiac Surgery Report (Adult)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines on the Diagnosis and Management of Pericardial
European Heart Journal (2004) Ã, 1–28 ESC Guidelines Guidelines on the Diagnosis and Management of Pericardial Diseases Full Text The Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology Task Force members, Bernhard Maisch, Chairperson* (Germany), Petar M. Seferovic (Serbia and Montenegro), Arsen D. Ristic (Serbia and Montenegro), Raimund Erbel (Germany), Reiner Rienmuller€ (Austria), Yehuda Adler (Israel), Witold Z. Tomkowski (Poland), Gaetano Thiene (Italy), Magdi H. Yacoub (UK) ESC Committee for Practice Guidelines (CPG), Silvia G. Priori (Chairperson) (Italy), Maria Angeles Alonso Garcia (Spain), Jean-Jacques Blanc (France), Andrzej Budaj (Poland), Martin Cowie (UK), Veronica Dean (France), Jaap Deckers (The Netherlands), Enrique Fernandez Burgos (Spain), John Lekakis (Greece), Bertil Lindahl (Sweden), Gianfranco Mazzotta (Italy), Joa~o Morais (Portugal), Ali Oto (Turkey), Otto A. Smiseth (Norway) Document Reviewers, Gianfranco Mazzotta, CPG Review Coordinator (Italy), Jean Acar (France), Eloisa Arbustini (Italy), Anton E. Becker (The Netherlands), Giacomo Chiaranda (Italy), Yonathan Hasin (Israel), Rolf Jenni (Switzerland), Werner Klein (Austria), Irene Lang (Austria), Thomas F. Luscher€ (Switzerland), Fausto J. Pinto (Portugal), Ralph Shabetai (USA), Maarten L. Simoons (The Netherlands), Jordi Soler Soler (Spain), David H. Spodick (USA) Table of contents Constrictive pericarditis . 9 Pericardial cysts . 13 Preamble . 2 Specific forms of pericarditis . 13 Introduction. 2 Viral pericarditis . 13 Aetiology and classification of pericardial disease. 2 Bacterial pericarditis . 14 Pericardial syndromes . ..................... 2 Tuberculous pericarditis . 14 Congenital defects of the pericardium . 2 Pericarditis in renal failure . 16 Acute pericarditis . 2 Autoreactive pericarditis and pericardial Chronic pericarditis . 6 involvement in systemic autoimmune Recurrent pericarditis . 6 diseases . 16 Pericardial effusion and cardiac tamponade . -

446 NQF #0773: Operative Mortality Stratified by the Five STS-EACTS Mortality Categories
Measure #446 (NQF 0733): Operative Mortality Stratified by the Five STS-EACTS Mortality Categories – National Quality Strategy Domain: Patient Safety 2017 OPTIONS FOR INDIVIDUAL MEASURES: REGISTRY ONLY MEASURE TYPE: Outcome DESCRIPTION: Percent of patients undergoing index pediatric and/or congenital heart surgery who die, including both 1) all deaths occurring during the hospitalization in which the procedure was performed, even if after 30 days (including patients transferred to other acute care facilities), and 2) those deaths occurring after discharge from the hospital, but within 30 days of the procedure, stratified by the five STAT Mortality Levels, a multi-institutional validated complexity stratification tool INSTRUCTIONS: This measure is to be reported for all pediatric and/or congenital heart patients each time a surgery is performed during the performance period. This measure is intended to reflect the quality of services provided for patients with congenital heart disease. This measure may be reported by eligible clinicians who perform the quality actions described in the measure based on the services provided and the measure-specific denominator coding. Measure Reporting: The listed denominator criteria is used to identify the intended patient population. The numerator quality-data codes included in this specification are used to submit the quality actions allowed by the measure. All measure-specific coding should be reported on the claim(s) representing the eligible encounter. THERE ARE TWO REPORTING CRITERIA FOR THIS MEASURE: -

The Conversion to Rastelli's Type Operation from Patrick-Mcgoon's
General Thoracic and Cardiovascular Surgery (2019) 67:551–553 https://doi.org/10.1007/s11748-018-0942-x CASE REPORT The conversion to Rastelli’s type operation from Patrick-McGoon’s procedure of an adult with Taussig–Bing heart: a case report Keiichi Fujiwara1 · Kousuke Yoshizawa1 · Nobuhisa Ohno1 · Hisanori Sakazaki2 Received: 30 January 2018 / Accepted: 18 May 2018 / Published online: 11 June 2018 © The Japanese Association for Thoracic Surgery 2018 Abstract A 23-year-old female of Taussig–Bing heart with antero-posterior relation of the great arteries was underwent Patrick- McGoon’s intraventricular rerouting at 6 years old of age. The left ventricular outflow obstruction (peak pressure gradient of 100 mmHg) developed, and severe aortic valve regurgitation following bacterial endocarditis was noted. The conversion to Rastelli’s type operation and aortic valve replacement were performed successfully at 23 years old of age. She is doing well without any significant left or right ventricular outflow obstruction at 7 years postoperatively. Keywords Taussig–Bing heart · Intraventricular rerouting · Patrick-McGoon’s operation · Left ventricular outflow obstruction · Adult congenital heart disease Introduction Case Taussig–Bing heart is characterized by double-outlet right A 23-year-old female diagnosed of double outlet right ventricle with subpulmonary ventricular septal defect [1, 2]. ventricle with subpulmonary ventricular septal defect and Currently, the arterial switch procedure as anatomic repair, antero-posterior relation of the great arteries, was referred to connecting the left ventricle to aorta and the right ventricle our hospital for severe left ventricular outflow tract obstruc- to pulmonary artery, is a popular surgical management for tion following Patrick-McGoon’s intraventricular rerouting Taussig–Bing heart regardless of relation of the great arter- and moderate to severe aortic valve regurgitation following ies. -

Situs Inversus Totalis with Aortopulmonary Shunt: a Case Report in an Ethiopian
Ethiop. J. Health Biomed Sci., 2009. Vol.2, No.1 CASE REPORT SITUS INVERSUS TOTALIS WITH AORTOPULMONARY SHUNT: A CASE REPORT IN AN ETHIOPIAN Ermias Diro1 SUMMARY I report a patient who presented with long standing dyspnea without physical signs of congestive heart failure and finally diag- nosed to have situs inversus totalis with aortopulmonary window. Situs inversus totalis refers to a mirror image reversal of the normal position of the internal organs. The recognition of concomitant congenital anomalies such as in the heart or other or- gans is extremely important as it may disturb surgical procedures for concomitant diseases. This is a very rare condition and a coexisting aortopulmonary window was not described before to the best of my knowledge. their normal positions. Situs inversus with dextrocar- dia is termed situs inversus totalis because the car- INTRODUCTION diac position as well as the atrial chambers and ab- dominal viscera are mirror images of the normal anatomy (3). The purpose of this case report is to describe and discuss a rare situation with an important clinical Typically, patients with situs inversus have a normal significance. life expectancy except in the rare instances of cardiac anomalies, depending on the severity of the defect. Situs describes the position of the cardiac atria and Patients with Kartagners syndrome, a triad of situs viscera. Situs solitus is the normal position, and situs inversus, sinusitis and bronchiectasis, have a normal inversus is the mirror image of situs solitus. Cardiac life expectancy if the bronchiectasis is treated ade- situs is determined by the atrial location. In situs in- quately. -
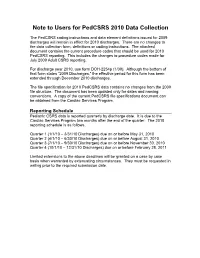
Note to Users for Pedcsrs 2010 Data Collection
Note to Users for PedCSRS 2010 Data Collection The PedCSRS coding instructions and data element definitions issued for 2009 discharges will remain in effect for 2010 discharges. There are no changes to the data collection form, definitions or coding instructions. The attached document contains the current procedure codes that should be used for 2010 PedCSRS reporting. This includes the changes to procedure codes made for July 2009 Adult CSRS reporting. For discharge year 2010, use form DOH-2254p (1/09). Although the bottom of that form states “2009 Discharges,” the effective period for this form has been extended through December 2010 discharges. The file specification for 2010 PedCSRS data contains no changes from the 2009 file structure. The document has been updated only for dates and naming conventions. A copy of the current PedCSRS file specifications document can be obtained from the Cardiac Services Program. Reporting Schedule Pediatric CSRS data is reported quarterly by discharge date. It is due to the Cardiac Services Program two months after the end of the quarter. The 2010 reporting schedule is as follows. Quarter 1 (1/1/10 – 3/31/10 Discharges) due on or before May 31, 2010 Quarter 2 (4/1/10 – 6/30/10 Discharges) due on or before August 31, 2010 Quarter 3 (7/1/10 – 9/30/10 Discharges) due on or before November 30, 2010 Quarter 4 (10/1/10 – 12/31/10 Discharges) due on or before February 28, 2011 Limited extensions to the above deadlines will be granted on a case by case basis when warranted by extenuating circumstances. -

Balloon Aortic Valvuloplasty
Original Research Article Journal of Structural Heart Disease, May 2015, Received: December 8, 2014 Volume 1, Issue 1: 20-32 Accepted: December 15, 2014 Published online: May 2015 DOI: http://dx.doi.org/10.12945/j.jshd.2015.00009-14 Balloon Aortic Valvuloplasty Patient Selection and Technical Considerations Ted Feldman, MD, FESC, FACC, MSCAI*, Mohammad Sarraf, MD, Wes Pedersen, MD, FACC, FSCAI Evanston Hospital, NorthShore University Health System, Evanston, Illinois NOTE: This manuscript includes videos. Not all PDF readers support video. For desktop computers we recommend using Adobe Acrobat Reader. To view videos within a PDF on an iPad we recommend viewing in ezPDF Reader or PDF Expert. On desktop computers you may view videos full screen by clicking on a video, right click on the video, then choose Full Screen Multimedia. Abstract BAV occurs in the vast majority of patients. While in BAV has had resurgence in association with the dissem- many this clinical improvement is short-lived, a ma- ination of TAVR. The lack of clear mortality benefit from jority of patients feel improved symptoms for as long BAV does not translate to lack of efficacy as a palliative as 1 year [1]. The utility of this therapy as a palliative therapy. BAV remains a useful bridge to surgical AVR or TAVR, and for symptom relief in patients who are not treatment is seen best among patients, who truly candidates for either AVR approach. It is also useful as a have no other option [2]. For example, the extreme diagnostic test for patients with low gradient-low out- risk patient, who is a candidate for neither surgical put AS, and for those with mixed pulmonary and aortic nor transcatheter AVR may undergo BAV periodically valvular disease. -

Surgery for Acquired Heart Disease
View metadata, citation and similar papers at core.ac.uk brought to you byCORE provided by Elsevier - Publisher Connector SURGERY FOR ACQUIRED HEART DISEASE EARLY RESULTS WITH PARTIAL LEFT VENTRICULECTOMY Patrick M. McCarthy, MD a Objective: We sought to determine the role of partial left ventriculectomy in Randall C. Starling, MD b patients with dilated cardiomyopathy. Methods: Since May 1996 we have James Wong, MBBS, PhD b performed partial left ventriculectomy in 53 patients, primarily (94%) in Gregory M. Scalia, MBBS b heart transplant candidates. The mean age of the patients was 53 years Tiffany Buda, RN a Rita L. Vargo, MSN, RN a (range 17 to 72 years); 60% were in class IV and 40% in class III. Marlene Goormastic, MPH c Preoperatively, 51 patients were thought to have idiopathic dilated cardio- James D. Thomas, MD b myopathy, one familial cardiomyopathy, and one valvular cardiomyopathy. Nicholas G. Smedira, MD a As our experience accrued we increased the extent of left ventriculectomy James B. Young, MD b and more complex mitral valve repairs. For two patients mitral valve replacement was performed. For 51 patients the anterior and posterior mitral valve leaflets were approximated (Alfieri repair); 47 patients also had ring posterior annuloplasty. In 27 patients (5!%) one or both papillary muscles were divided, additional left ventricular wall was resected, and the papillary muscle heads were reimplanted. Results: Echocardiography showed a significant decrease in left ventricular dimensions after resection (8.3 cm to 5.8 cm), reduction in mitral regurgitation (2.8+ to 0), and increase in forward ejection fraction (15.7% to 32.7%). -

Closed Mitral Commissurotomy—A Cheap, Reproducible and Successful Way to Treat Mitral Stenosis
149 Editorial Closed mitral commissurotomy—a cheap, reproducible and successful way to treat mitral stenosis Manuel J. Antunes Clinic of Cardiothoracic Surgery, Faculty of Medicine, University of Coimbra, Coimbra, Portugal Correspondence to: Prof. Manuel J. Antunes. Faculty of Medicine, University of Coimbra, 3000-075 Coimbra, Portugal. Email: [email protected]. Provenance and Peer Review: This article was commissioned by the Editorial Office, Journal of Thoracic Disease. The article did not undergo external peer review. Comment on: Xu A, Jin J, Li X, et al. Mitral valve restenosis after closed mitral commissurotomy: case discussion. J Thorac Dis 2019;11:3659-71. Submitted Oct 23, 2019. Accepted for publication Nov 29, 2019. doi: 10.21037/jtd.2019.12.118 View this article at: http://dx.doi.org/10.21037/jtd.2019.12.118 In the August issue of the Journal, Xu et al. (1), from Bayley (4,5) and then became widely accepted. Subsequently, China, discuss the case of a patient who had a successful the technique of CMC suffered several modifications, both reoperation for restenosis of the mitral valve performed in the way the mitral valve was accessed and split. Several 30 years after closed mitral commissurotomy (CMC). instruments were created to facilitate the opening of the The specific aspects of this case were most appropriately commissures, culminating with the development of the commented by several experienced surgeons from different Tubbs dilator, which became the standard instrument for parts of the world. I was now invited by the Editor of this the procedure (Figure 1). Journal to write a Comment on this paper and its subject. -

Mustard Procedure Br Heart J: First Published As 10.1136/Hrt.72.1.85 on 1 July 1994
Br Heart J 1994;72:85-88 85 Transcatheter stent implantation for recurrent pulmonary venous pathway obstruction after the Mustard procedure Br Heart J: first published as 10.1136/hrt.72.1.85 on 1 July 1994. Downloaded from Martin C K Hosking, Kenneth A Murdison, Walter J Duncan Abstract pathway obstruction reaching a maximum A 5 year old boy presented with obstruc- flow velocity of 2'0 m/s associated with a tion of the pulmonary venous pathway stenosis measuring 2-3 mm in diameter. four years after the Mustard procedure. Right ventricular dysfunction was a persistent A successful balloon dilatation ofthe pul- echocardiographic finding associated with an monary venous pathway was performed increase in left ventricle dimension in but the benefit was transient. Placement response to the rise of pulmonary arterial of a 10 mm balloon expandable intravas- pressure secondary to the pulmonary venous cular stent across the recurrent stenosis inflow obstruction. A significant systemic to resulted in complete relief ofthe obstruc- pulmonary venous chamber baffle leak mea- tion with prompt resolution ofthe clinical suring 5 mm x 4 mm with right to left shunting signs. The delivery system was modified was seen by Doppler colour flow mapping and to facilitate stent delivery. contributed to central cyanosis. Serial chest x ray films showed persistence of cardiomegaly (Br Heart 1994;72:85-88) with increasing evidence of pulmonary venous congestion. To avoid the risks of surgical repair in a Paediatric experience with transcatheter patient with impaired -

Coronary Artery Disease and Transcatheter Aortic Valve Replacement JACC State-Of-The-Art Review
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL. 74, NO. 3, 2019 ª 2019 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION PUBLISHED BY ELSEVIER THE PRESENT AND FUTURE JACC STATE-OF-THE-ART REVIEW Coronary Artery Disease and Transcatheter Aortic Valve Replacement JACC State-of-the-Art Review Laurent Faroux, MD, MSC, Leonardo Guimaraes, MD, Jérôme Wintzer-Wehekind, MD, Lucia Junquera, MD, Alfredo Nunes Ferreira-Neto, MD, David del Val, MD, Guillem Muntané-Carol, MD, Siamak Mohammadi, MD, Jean-Michel Paradis, MD, Josep Rodés-Cabau, MD ABSTRACT About one-half of transcatheter aortic valve replacement (TAVR) candidates have coronary artery disease (CAD), and controversial results have been reported regarding the effect of the presence and severity of CAD on clinical outcomes post-TAVR. In addition to coronary angiography, promising data has been recently reported on both the use of computed tomography angiography and the functional invasive assessment of coronary lesions in the work-up pre-TAVR. While waiting for the results of ongoing randomized trials, percutaneous revascularization of significant coronary lesions has been the routine strategy in TAVR candidates with CAD. Also, scarce data exists on the incidence, characteristics, and management of coronary events post-TAVR, and increasing interest exist on potential coronary access challenges in patients requiring coronary angiography/intervention post-TAVR. This review provides an updated overview of the current landscape of CAD in TAVR recipients, focusing on its prevalence, clinical impact, pre- and post-procedural evaluation and management, unresolved issues and future perspectives. (J Am Coll Cardiol 2019;74:362–72) © 2019 by the American College of Cardiology Foundation. -

Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Pediatric Cardiovascular Arterial Switch Operation Surgery Surgical Solutions to Complex Problems Tom R. Karl, MS, MD The arterial switch operation is appropriate treatment for most forms of transposition of Andrew Cochrane, FRACS the great arteries. In this review we analyze indications, techniques, and outcome for Christian P.R. Brizard, MD various subsets of patients with transposition of the great arteries, including those with an intact septum beyond 21 days of age, intramural coronary arteries, aortic arch ob- struction, the Taussig-Bing anomaly, discordant (corrected) transposition, transposition of the great arteries with left ventricular outflow tract obstruction, and univentricular hearts with transposition of the great arteries and subaortic stenosis. (Tex Heart Inst J 1997;24:322-33) T ransposition of the great arteries (TGA) is a prototypical lesion for pediat- ric cardiac surgeons, a lethal malformation that can often be converted (with a single operation) to a nearly normal heart. The arterial switch operation (ASO) has evolved to become the treatment of choice for most forms of TGA, and success with this operation has become a standard by which pediatric cardiac surgical units are judged. This is appropriate, because without expertise in neonatal anesthetic management, perfusion, intensive care, cardiology, and surgery, consistently good results are impossible to achieve. Surgical Anatomy of TGA In the broad sense, the term "TGA" describes any heart with a discordant ven- triculoatrial (VA) connection (aorta from right ventricle, pulmonary artery from left ventricle). The anatomic diagnosis is further defined by the intracardiac fea- tures. Most frequently, TGA is used to describe the solitus/concordant/discordant heart. -

Reduction Ventriculoplasty for Dilated Cardiomyopathy : the Batista Procedure Shahram Salemy Yale University
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1999 Reduction ventriculoplasty for dilated cardiomyopathy : the Batista procedure Shahram Salemy Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Salemy, Shahram, "Reduction ventriculoplasty for dilated cardiomyopathy : the Batista procedure" (1999). Yale Medicine Thesis Digital Library. 3123. http://elischolar.library.yale.edu/ymtdl/3123 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. SlDDCITOM VENTRICULOPIASTy FOR DILATED CARDIOMYOPATHY THE BATISTA PROCEDURE W«M * (e,yx»> ShaLramSalemy YALE DNIVERSriY YALE UNIVERSITY CUSHING/WHITNEY MEDICAL LIBRARY Permission to photocopy or microfilm processing of this thesis for the purpose of individual scholarly consultation or reference is hereby granted by the author. This permission is not to be interpreted as affecting publication of this work or otherwise placing it in the public domain, and the author reserves all rights of ownership guaranteed under common law protection of unpublished manuscripts. Signature of Author Date REDUCTION VENTRICULOPLASTY FOR DILATED CARDIOMYOPATHY: THE BATISTA PROCEDURE Shahram Salemy B.S., George Tellides M.D., Ph.D., and John A. Elefteriades M.D. February 5, 1999 r 113 f'Uh (e(e.cl 0 REDUCTION VENTRICULOPLASTY FOR DILATED CARDIOMYOPATHY: THE BATISTA PROCEDURE.