Relationship Between Bilirubin and Auditory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Audiometry Techniques, Circuits, and Systems
M. Tech. Credit Seminar Report, Electronic Systems Group, EE Dept, IIT Bombay submitted Nov 03 Audiometry techniques, circuits, and systems Vineet P. Aras (Roll No. 03307411) Supervisor: Prof. P. C. Pandey Abstract Audiometry is the technique to identify and quantitatively determine the degree of hearing loss of a person by measuring his hearing sensitivity, so that suitable medical treatment or one of the appropriate hearing aids and assistive devices can be prescribed. In audiological investigations, the hearing sensitivity is tested for pure tones, speech or other sound stimuli. The result, when plotted graphically, is called an audiogram. The electronic instrument used for measuring the hearing threshold level is called an audiometer. Using it, the test tones of different frequencies and levels are generated and presented to the patient and hearing thresholds are determined on the basis of patient s response. The auditory system and its disorders are described. Different audiometric tests, techniques and various audiometers are discussed. 1. Introduction There could be various disorders in the various parts of the ear. Audiological investigations help us to diagnose the nature of deafness and localise the site of disorder. The method by which patient's hearing sensitivity can be determined is termed as audiometry [1]. It helps in assessing the nature, degree, and probable cause of the hearing impairment. In this technique, auditory stimuli with varying intensity levels are presented to the person who responds to these stimuli. The minimum intensity level of these stimuli to which consistent responses are obtained is taken as the threshold of hearing . Depending on this threshold, the patient s hearing sensitivity can be estimated by obtaining an audiogram. -

Investigation of the Perception of Tone Quality Changes During Conventional Tone Decay Test Procedures with Normally Hearing Human Subjects
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1986 Investigation of the perception of tone quality changes during conventional tone decay test procedures with normally hearing human subjects Anne M. Cook The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Cook, Anne M., "Investigation of the perception of tone quality changes during conventional tone decay test procedures with normally hearing human subjects" (1986). Graduate Student Theses, Dissertations, & Professional Papers. 2759. https://scholarworks.umt.edu/etd/2759 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. COPYRIGHT ACT OF 1976 THIS IS AN UNPUBLISHED MANUSCRIPT IN WHICH COPYRIGHT SUB SISTS. ANY FURTHER REPRINTING OF ITS CONTENTS MUST BE APPROVED BY THE AUTHOR, MANSFIELD LIBRARY UNIVERSITY OF [MONTANA DATE: 1986_ An Investigation of the Perception of Tone Quality Changes During Conventional Tone Decay Test Procedures with Normally Hearing Human Subjects By Anne M. Cook B.S., University of Washington, 1983 Presented in partial fulfillment of the requirements for the degree of Master of Arts University of Montana 1986 Approved by: Chair, Board of Maminers Dean", Gr a d ua te Sc hoo 1 / : H ftL Date ~]f UMI Number: EP34804 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. -

Audiology Staff At
3rd Edition contributions from and compilation by the VA Audiology staff at Mountain Home, Tennessee with contributions from the VA Audiology staffs at Long Beach, California and Nashville, Tennessee Department of Veterans Affairs Spring, 2009 TABLE OF CONTENTS Preface ...................................................................................................................... iii INTRODUCTION ..............................................................................................................1 TYPES OF HEARING LOSS ...........................................................................................1 DIAGNOSTIC AUDIOLOGY ............................................................................................3 Case History ...............................................................................................................3 Otoscopic Examination ..............................................................................................3 Pure-Tone Audiometry ...............................................................................................3 Masking ......................................................................................................................6 Audiometric Tuning Fork Tests ..................................................................................6 Examples of Pure-Tone Audiograms ........................................................................7 Speech Audiometry ....................................................................................................8 -

Evaluation of Hearing Impairment Corporate Medical Policy
Evaluation of Hearing Impairment Corporate Medical Policy File Name: Evaluation of Hearing Impairment File Code: UM.DIAG.01 Origination: 07/1997 Last Review: 01/2019 Next Review: 01/2020 Effective Date: 10/01/2019 Description/Summary Hearing impairment or hearing loss is a reduction in the ability to perceive sound. The loss may range from slight to complete deafness. Audiometric studies are diagnostic tests that evaluate sensorineural and conductive hearing losses. Conductive hearing loss is the result of disorders of the external or middle ear; sensory hearing loss is secondary to disturbance of the cochlea; neural hearing loss results from disease of the auditory (eighth) nerve or central auditory channel connections. Sensory and neural hearing losses are frequently included under the term sensorineural hearing loss. Mixed or combined hearing loss involves disturbances of both conductive and sensorineural mechanisms. Policy Coding Information Click the links below for attachments, coding tables & instructions. Attachment I- CPT® coding table & instructions When a service may be considered medically necessary The Plan covers a screening test for hearing in conjunction with a preventive medicine evaluation and management service when done in accordance with current American Academy of Pediatrics, American Academy of Family Practice, and/or Bright Futures guidelines. Audiometric studies may be medically necessary for patients who have experienced or continue to experience illnesses or injuries which may predispose them to hearing loss -

Audiological Evaluation in Patients of Diabetes Mellitus
International Journal of Research and Review www.ijrrjournal.com E-ISSN: 2349-9788; P-ISSN: 2454-2237 Original Research Article Audiological Evaluation in Patients of Diabetes Mellitus Rajendra Kumar Gorwara1, Hemendra Bamaniya2, Padam Chand Ajmera3 1Assistant Professor, Department of ENT, Pacific Medical College & Hospital, Udaipur 2Associate Professor, Department of ENT, Ananta Institute of Medical Sciences, Rajsamand 3Professor, Department of ENT, Pacific Medical College & Hospital, Udaipur Corresponding Author: Hemendra Bamaniya ABSTRACT Aims & objective: the objective of present study was to assess the hearing loss in patients of diabetes mellitus type II by clinical and audiometric examinations. Material and methods: this prospective study was done in the department of ENT, Pacific Medical College and Hospital, Udaipur during the period from January 2016 to January 2018. 100 cases of diabetes mellitus type II were included in the study. 100 healthy were included in the study as controls. Complete routine and audiological investigations were done in all the subjects including audiogram, acoustic reflex, tone decay test, speech discrimination score and short increment sensitivity index score and the results were compared between cases and controls. Results: the study includes 100 diabetic cases with mean age 52.5 (age ranges from 40-60 years). Cases include 74 males and 26 females. 100 healthy controls were included with mean age 53.1. Age and sex were matched with cases. Prevalence of hearing loss was 46% in cases and 11% in controls. Hearing loss in all the subject was of sensorineural type (SNHL). Among cases, 3 patients had unilateral and 43 cases had bilateral hearing loss. All the 11 controls had bilateral hearing loss. -
Paper 1 Suppl Data File 2.Xlsx
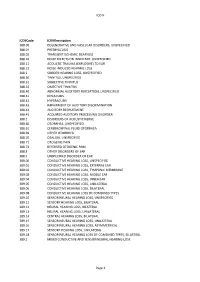
ICD-9 ICD9Code ICD9Description 388.00 DEGENERATIVE AND VASCULAR DISORDERS, UNSPECIFIED 388.01 PRESBYACUSIS 388.02 TRANSIENT ISCHEMIC DEAFNESS 388.10 NOISE EFFECTS ON INNER EAR, UNSPECIFIED 388.11 ACOUSTIC TRAUMA (EXPLOSIVE) TO EAR 388.12 NOISE-INDUCED HEARING LOSS 388.2 SUDDEN HEARING LOSS, UNSPECIFIED 388.30 TINNITUS, UNSPECIFIED 388.31 SUBJECTIVE TINNITUS 388.32 OBJECTIVE TINNITUS 388.40 ABNORMAL AUDITORY PERCEPTION, UNSPECIFIED 388.41 DIPLACUSIS 388.42 HYPERACUSIS 388.43 IMPAIRMENT OF AUDITORY DISCRIMINATION 388.44 AUDITORY RECRUITMENT 388.45 ACQUIRED AUDITORY PROCESSING DISORDER 388.5 DISORDERS OF ACOUSTIC NERVE 388.60 OTORRHEA, UNSPECIFIED 388.61 CEREBROSPINAL FLUID OTORRHEA 388.69 OTHER OTORRHEA 388.70 OTALGIA, UNSPECIFIED 388.71 OTOGENIC PAIN 388.72 REFERRED OTOGENIC PAIN 388.8 OTHER DISORDERS OF EAR 388.9 UNSPECIFIED DISORDER OF EAR 389.00 CONDUCTIVE HEARING LOSS, UNSPECIFIED 389.01 CONDUCTIVE HEARING LOSS, EXTERNAL EAR 389.02 CONDUCTIVE HEARING LOSS, TYMPANIC MEMBRANE 389.03 CONDUCTIVE HEARING LOSS, MIDDLE EAR 389.04 CONDUCTIVE HEARING LOSS, INNER EAR 389.05 CONDUCTIVE HEARING LOSS, UNILATERAL 389.06 CONDUCTIVE HEARING LOSS, BILATERAL 389.08 CONDUCTIVE HEARING LOSS OF COMBINED TYPES 389.10 SENSORINEURAL HEARING LOSS, UNSPECIFIED 389.11 SENSORY HEARING LOSS, BILATERAL 389.12 NEURAL HEARING LOSS, BILATERAL 389.13 NEURAL HEARING LOSS, UNILATERAL 389.14 CENTRAL HEARING LOSS, BILATERAL 389.15 SENSORINEURAL HEARING LOSS, UNILATERAL 389.16 SENSORINEURAL HEARING LOSS, ASYMMETRICAL 389.17 SENSORY HEARING LOSS, UNILATERAL 389.18 SENSORINEURAL -
Vertigo and Dizziness: a Study of Relationships to Audiological Testing and Patient History Data
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1972 Vertigo and dizziness: a study of relationships to audiological testing and patient history data Nancy Lee Crosby The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Crosby, Nancy Lee, "Vertigo and dizziness: a study of relationships to audiological testing and patient history data" (1972). Graduate Student Theses, Dissertations, & Professional Papers. 6190. https://scholarworks.umt.edu/etd/6190 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. VERTIGO Aim DIZZINESS: A STUDY OF RELATIONSHIPS TO AUDIOLOGICAL TESTING AND PATIENT HISTORY DATA By Nancy L. Crosby B.A., University of Montana, 1962 Presented in partial fulfillment of the requirements for the degree of Master of Arts UNIVERSITY OF MONTANA 1972 Approved by: Chairman, Board of Examiners ^ j ili Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. UMI Number: EP36991 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. -

Acoustic Reflex Measurements and the Loudness Function in Sensorineural Hearing Loss
ACOUSTIC REFLEX MEASUREMENTS AND THE LOUDNESS FUNCTION IN SENSORINEURAL HEARING LOSS SHEILA ULIEL, M.A. (AUDIOLOGY) (WITWATERSRAND) Unit for Hearing-impaired Children, University of the Witwatersrand, Johannesburg. SUMMARY The suprathreshold acoustic reflex responses of forty two ears affected by sensorineural hearing loss of cochlear origin and fifty-eight ears demonstrating normal hearing, were recorded by means of an electro-acoustic impedance meter and attached X-Y recorder. The recordings were done in ascending and descending fashion, at successively increasing and decreasing 5 dB intensity levels from 90-120-90 dB HL respectively, for the individual pure-tone frequencies of 500, 1 000, 2 000 and 4 000 Hz. The contralateral mode of measurement was employed. Analysis of these recordings indicated that the acoustic reflex responses could be differentiated into five characteristic patterns of growth, which could be depicted upon a continuum of peaked, peaked-rounded, rounded, rounded-flat, and flat shapes. The peaked and peaked-rounded patterns were found to predominate at all four pure-tone frequencies in the normal ears, while the rounded-fiat and flat patterns were found to predominate only at the higher pure-tone frequencies of 2 000 and 4 000 Hz in the ears affected by sensorineural hearing loss. This latter relationship was also able to be applied to two disorders of the loudness function — loudness recruitment and hyperacusis. It was concluded that the flattened acoustic reflex patterns at the higher pure-tone frequencies constituted a potential diagnostic cue related to the differential diagnosis of sensori-neural hearing loss, and to disorders of the loudness function. -

Assessing Auditory Nerve Condition by Tone Decay in Deaf Subjects with a Cochlear Implant
International Journal of Audiology ISSN: 1499-2027 (Print) 1708-8186 (Online) Journal homepage: https://www.tandfonline.com/loi/iija20 Assessing auditory nerve condition by tone decay in deaf subjects with a cochlear implant Jan-Willem A. Wasmann, Ruben H. M. van Eijl, Huib Versnel & Gijsbert A. van Zanten To cite this article: Jan-Willem A. Wasmann, Ruben H. M. van Eijl, Huib Versnel & Gijsbert A. van Zanten (2018) Assessing auditory nerve condition by tone decay in deaf subjects with a cochlear implant, International Journal of Audiology, 57:11, 864-871, DOI: 10.1080/14992027.2018.1498598 To link to this article: https://doi.org/10.1080/14992027.2018.1498598 © 2018 British Society of Audiology, International Society of Audiology, and Nordic Audiological Society. Published by Informa UK Limited, trading as Taylor & Francis Group. Published online: 27 Sep 2018. Submit your article to this journal Article views: 182 View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=iija20 INTERNATIONAL JOURNAL OF AUDIOLOGY 2018, VOL. 57, NO. 11, 864–871 https://doi.org/10.1080/14992027.2018.1498598 ORIGINAL ARTICLE Assessing auditory nerve condition by tone decay in deaf subjects with a cochlear implant Jan-Willem A. Wasmanna,b, Ruben H. M. van Eijla,c, Huib Versnela,c and Gijsbert A. van Zantena,c aDepartment of Otorhinolaryngology and Head & Neck Surgery, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands; bDepartment of Otorhinolaryngology, Radboud University Medical Center, Nijmegen, The Netherlands; cBrain Center Rudolf Magnus, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands ABSTRACT ARTICLE HISTORY The condition of the auditory nerve is a factor determining hearing performance of cochlear implant (CI) Received 8 June 2016 recipients. -
![Overview of Hearing Loss in the Elderly Molinier CE*, Gallois Y, Marx M and Fraysse B Polygenicity [7]](https://docslib.b-cdn.net/cover/5545/overview-of-hearing-loss-in-the-elderly-molinier-ce-gallois-y-marx-m-and-fraysse-b-polygenicity-7-4165545.webp)
Overview of Hearing Loss in the Elderly Molinier CE*, Gallois Y, Marx M and Fraysse B Polygenicity [7]
Open Access Gerontology & Geriatrics: Research Special Article - Hearing Loss Overview of Hearing Loss in the Elderly Molinier CE*, Gallois Y, Marx M and Fraysse B polygenicity [7]. At present, a genetic examination is not systematically Department of Otoneurology-Head and Neck Surgery, conducted in the context of classical presbycusis. Pierre-Paul Riquet University Hospital Center of Toulouse, France Screening for hearing loss *Corresponding author: Charles-Edouard Molinier, There is no universal screening system for adults as hearing loss is Department of Otoneurology-Head and Neck Surgery, currently defined by general practitioners, ENT specialists or hearing Pierre-Paul Riquet University Hospital Center, France aid acousticians on request by the patient or family. Received: December 11, 2019; Accepted: January 03, WHO-sponsored awareness days such as World Hearing Day, 2020; Published: January 10, 2020 held on March 3rd each year, provide free screening for patients at Introduction participating centers in many countries. The gold standard in the diagnosis of presbycusis is still tonal Deafness is a major public health issue worldwide. According to and vocal audiometry. Therefore, presbycusis appears to be bilateral the World Health Organization (WHO), of all diseases it is the 4th symmetrical sensorineural hearing loss that is predominant in high leading cause of morbidity. The WHO defines hearing loss as a loss of frequencies on tonal audiometry. Speech audiometry identifies more than 25dB in the ear with best hearing. Deafness is considered difficulties in speech discrimination with an increase in the disabling when hearing loss exceeds 40dB in adults and 30dB in intelligibility threshold, which corresponds with the dB threshold children in the best ear. -

Study of Retro Cochlear Pathology for Finding Hearing Ability Using Tone Decay Test by Dr
Global Journal of Medical Research: D Radiology, Diagnostic Imaging and Instrumentation Volume 16 Issue 2 Version 1.0 Year 2016 Type: Double Blind Peer Reviewed International Research Journal Publisher: Global Journals Inc. (USA) Online ISSN: 2249-4618 & Print ISSN: 0975-5888 Study of Retro Cochlear Pathology for finding Hearing Ability using Tone Decay Test By Dr. Sharmila. R. Chaudhari P D E A’s Baburaoji Gholap College Abstract- Pure tone Audiometry (PTA)-Tone Decay Test is the key hearing test used to identify hearing threshold levels of an individual, enabling determination of the degree, type and configuration of a hearing loss. The test is used to indentify quickly screening for Retro Cochlear pathology. In audio logical investigations, the hearing sensitivity is tested for pure tones. The test tones of different frequencies and levels are generated and presented to the patient and hearing thresholds are determined on the basis of patient’s response. Thus in this work we described the auditory system and its disorders. Keywords: audiometer, pure tone decay. GJMR-D Classification: NLMC Code: WV 201 StudyofRetroCochlearPathologyforfindingHearingAbilityusingToneDecayTest Strictly as per the compliance and regulations of: © 2016. Dr. Sharmila. R. Chaudhari. This is a research/review paper, distributed under the terms of the Creative Commons Attribution-Noncommercial 3.0 Unported License http://creativecommons.org/licenses/by-nc/3.0/), permitting all non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Study of Retro Cochlear Pathology for finding Hearing Ability using Tone Decay Test Dr. Sharmila. R. Chaudhari Abstract- Pure tone Audiometry (PTA)-Tone Decay Test is the METER is used to perform Tone Decay Test & results key hearing test used to identify hearing threshold levels of an are concluded. -
Hearing Loss
Assessment of Hearing and Management of hearing loss DR. H. P. SINGH Additional Professor Department of ENT & Head Neck Surgery Disclaimer This presentation is for educational purposes only not for commercial activity. Principles of hearing Air-conduction Bone-conduction Why do we test hearing To detect one of major hearing impairment Quality: Sensorineural (perception) or Conductive Quantity: how much dB loss Types of Hearing Loss Conductive: External or Middle ear pathology Sensorineural: Damage at the inner ear (cochlea) Mixed: Both cochlear damage & outer/middle ear pathology Tests for detection of hearing loss Finger friction Watch test Speech test Loud conversation at 12 meter Whisper at 6 meter Tuning fork test Weber test Rinne test Bing test Schwabach’s test Gelle’s test Audiometry Objective Subjective Speech test App. 6 meter distance Each ear must be test separately Patient should repeat 5 words whispered by the doctor, 5 words told loudly High-frequency words (silence, similarly, sitting) Low-frequency words (drum, button) Results: loss of high frequencies – perception disease (i.e. presbyacusis) low frequencies – conductive disease (i.e. otitis media) Tuning fork tests these allow one to distinguish (much more clearly) between conductive and sensorineural deafness Frequencies: 128, 256, 512, 1024, 2048 & 4096 Hz Rinne´s test ➢ comparison is made between bone and air conduction ➢ base of a tuning fork is placed to the mastoid area (bone), and then after the sound is no longer appreciated, the vibrating