Medicare Benefit Policy Manual Chapter 10 - Ambulance Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ambulance Transportation Billing Guide
Washington Apple Health (Medicaid) Ambulance Transportation Billing Guide January 1, 2021 Disclaimer Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between this document and a Health Care Authority (HCA) rule arises, HCA rules apply. Billing guides are updated on a regular basis. Due to the nature of content change on the internet, we do not fix broken links in past guides. If you find a broken link, please check the most recent version of the guide. If this is the most recent guide, please notify us at [email protected]. About this guide* This publication takes effect January 1, 2021, and supersedes earlier billing guides to this program. HCA is committed to providing equal access to our services. If you need an accommodation or require documents in another format, please call 1-800-562- 3022. People who have hearing or speech disabilities, please call 711 for relay services. Washington Apple Health means the public health insurance programs for eligible Washington residents. Washington Apple Health is the name used in Washington State for Medicaid, the children’s health insurance program (CHIP), and state-only funded health care programs. Washington Apple Health is administered by the Washington State Health Care Authority. Refer also to HCA’s ProviderOne Billing and Resource Guide for valuable information to help you conduct business with HCA. How can I get HCA Apple Health provider documents? To access provider alerts, go to HCA’s provider alerts webpage. To access provider documents, go to HCA’s provider billing guides and fee schedules webpage. -

Ambulance Helicopter Contribution to Search and Rescue in North Norway Ragnar Glomseth1, Fritz I
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Glomseth et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:109 DOI 10.1186/s13049-016-0302-8 ORIGINAL RESEARCH Open Access Ambulance helicopter contribution to search and rescue in North Norway Ragnar Glomseth1, Fritz I. Gulbrandsen2,3 and Knut Fredriksen1,4* Abstract Background: Search and rescue (SAR) operations constitute a significant proportion of Norwegian ambulance helicopter missions, and they may limit the service’s capacity for medical operations. We compared the relative contribution of the different helicopter resources using a common definition of SAR-operation in order to investigate how the SAR workload had changed over the last years. Methods: We searched the mission databases at the relevant SAR and helicopter emergency medical service (HEMS) bases and the Joint Rescue Coordination Centre (North) for helicopter-supported SAR operations within the potential operation area of the Tromsø HEMS base in 2000–2010. We defined SAR operations as missions over land or sea within 10 nautical miles from the coast with an initial search phase, missions with use of rescue hoist or static rope, and avalanche operations. Results: There were 769 requests in 639 different SAR operations, and 600 missions were completed. The number increased during the study period, from 46 in 2000 to 77 in 2010. The Tromsø HEMS contributed with the highest number of missions and experienced the largest increase, from 10 % of the operations in 2000 to 50 % in 2010. Simple terrain and sea operations dominated, and avalanches accounted for as many as 12 % of all missions. -
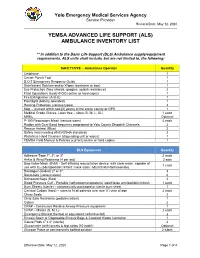
(Als) Ambulance Inventory List
Yolo Emergency Medical Services Agency Service Provider Revised Date: May 12, 2020 YEMSA ADVANCED LIFE SUPPORT (ALS) AMBULANCE INVENTORY LIST ** In addition to the Basic Life Support (BLS) Ambulance supply/equipment requirements, ALS units shall include, but are not limited to, the following: SAFETY/PPE – Ambulance Operator Quantity Cellphone 1 Center Punch Tool 1 D.O.T Emergency Response Guide 1 Disinfectant Solution and/or Wipes (container or box) 1 Eye Protection (face shields, goggles, splash resistance) 2 Field Operations Guide (FOG) online or hard copies 1 Fire Extinguisher (A-B-C) 1 Flashlight (battery operated) 1 Hearing Protection (various types) 2 Map – (current within two [2] years) of the entire county or GPS 1 Medical Grade Gloves, Latex free – sizes (S, M, L, XL) 1 each MREs Optional P-100 Respiratory Mask (various sizes) 4 each Radios with Dual Band frequency programed to Yolo County Dispatch Channels 2 Rescue Helmet (Blue) 2 Safety Vest meeting ANSI/OSHA standards 2 Waterless Hand Cleanser (dispensing unit or wipes) 1 YEMSA Field Manual & Policies (current) online or hard copies 1 BLS Equipment Quantity Adhesive Tape 1", 2", or 3" 2 each Ankle & Wrist Restraints (4 per set) 2 sets Bag-Valve-Mask (BVM) - Self-inflating resuscitation device, with clear mask, capable of 1 each use with O2 (adult/pediatric/infant; mask sizes: adult/child/infant/neonate) Bandages (Rolled) 2" or 3" 3 Band-Aids (various sizes) 6 Biohazard Bags (Red) 2 Blood Pressure Cuff - Portable (sphygmomanometers) (adult/large arm/pediatric/infant) 1 each -

Healthy Choices Get a Head Start on Great Health
Healthy Choices Get a Head Start on Great Health 2015 Benefits Guide MedStar Georgetown University Hospital, Non-union MedStar Health Research Institute MedStar National Rehabilitation Network Non-hospital Based Businesses, South Table of Contents 1 Enrollment Checklist 2 Enrollment Guidelines 3 Online Enrollment Instructions 4 Wellness Resources 4 Your Medical Plan Options 5 COBRA Continued Benefit Coverage 6 2015 Medical Plan Options Chart 8 Prescription Drug Plans 9 Your Dental Plan Options 11 Your Vision Plan Option 12 Flexible Spending Accounts (FSAs) 14 Life Insurance 14 Accidental Death and Dismemberment Insurance 15 Disability Plans 15 Universal Life, Critical Illness and Accident Insurances 16 Legal Resources 16 MedStar Associate Advantages 18 Contact Information i 2015 Annual Enrollment Choices For Healthy Living MedStar Health provides a comprehensive benefits If you are a benefit-eligible associate, take advantage of package for you and your family—MedStar Total MedStar Total Rewards. You must enroll online to receive Rewards. You are responsible for selecting the best mix medical, dental, vision, flexible spending accounts, of benefits to meet your needs and actively managing supplemental life, supplemental accidental death and these benefits and your health throughout the year. Use dismemberment, dependent life, or legal coverage in 2015. this guide to select your MedStar Total Rewards health and welfare package for 2015. Enrollment Checklist Read through this guide to design your MedStar Total Rewards package for 2015. Medical Accidental Death and Dismemberment Elect a healthcare coverage option. Insurance • MedStar Select Plan Consider if additional coverage would give your • CareFirst BlueCross BlueShield Preferred family more peace of mind. Provider Organization (PPO) Plan • Kaiser Permanente Health Maintenance Disability Organization (HMO) Plan MedStar provides full-time associates with short- and long-term disability coverage equal to 60 Dental percent of your base pay, at no cost to you. -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b. -

MEDICAL COVERAGE POLICY SERVICE: Air Ambulance
MEDICAL COVERAGE POLICY SERVICE: Air Ambulance Policy Number: 282 Effective Date: 05/01/2021 Last Review: 03/25/2021 Next Review Date: 03/25/2022 Important note: Unless otherwise indicated, this policy will apply to all lines of business. Even though this policy may indicate that a particular service or supply may be considered medically necessary and thus covered, this conclusion is not based upon the terms of your particular benefit plan. Each benefit plan contains its own specific provisions for coverage and exclusions. Not all benefits that are determined to be medically necessary will be covered benefits under the terms of your benefit plan. You need to consult the Evidence of Coverage (EOC) or Summary Plan Description (SPD) to determine if there are any exclusions or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and your plan of benefits, the provisions of your benefits plan will govern. However, applicable state mandates will take precedence with respect to fully insured plans and self-funded non-ERISA (e.g., government, school boards, church) plans. Unless otherwise specifically excluded, Federal mandates will apply to all plans. With respect to Medicare-linked plan members, this policy will apply unless there are Medicare policies that provide differing coverage rules, in which case Medicare coverage rules supersede guidelines in this policy. Medicare-linked plan policies will only apply to benefits paid for under Medicare rules, and not to any other health benefit plan benefits. CMS's Coverage Issues Manual can be found on the CMS website. -

State Ambulance Policies and Services (OEI-09-95-00410; 2/98)
- - -- -------- --of -- - OFFICE OF INSPECTOR GENERAL FEBRUARY 1998 OEI-09-95-00410 EXECUTIVE SUMMARY PURPOSE To provide baseline data about the ambulance industry and determine how State and local ordinances affect the delivery of ambulance services. BACKGROUND According to Section 1861(s)(7) of Social Security Act, Medicare pays for medically necessary ambulance services when other forms of transportation would endanger the beneficiary’s health. Ambulance suppliers provide two distinct levels of service--advanced life support and basic life support. The major distinctions between the levels are the types of vehicles and the skills of the personnel and the services they render. The Health Care Financing Administration (HCFA) is considering proposed Medicare regulations that would base reimbursement for ambulance services on the patient’s condition rather than the type of vehicle and personnel used. The final rule may include a special waiver for suppliers in non-Metropolitan Statistical Areas who would be hurt financially if they use only advanced life support ambulances. The HCFA may consider several options and may include a special waiver only if HCFA is convinced through overwhelming information of the need for the waiver. We decided to examine the effect and need for a special waiver based on Metropolitan Statistical Areas and non-Metropolitan Statistical Areas. In addition, we developed baseline information on the number of ambulance suppliers, vehicles, and personnel nationwide. We conducted in-person and telephone interviews with 53 State Emergency Medical Services Directors for the 50 States, the District of Columbia, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands. Using a structured discussion guide, we (1) identified State, county, and municipal mandates that require specific levels of ambulance services and (2) obtained baseline data on the number of suppliers, licensed vehicles, and certified personnel operating within the States in 1995 and 1996. -
Revitalizing Health for All: Case Studies Of
REVITALIZING HEALTH FOR ALL Case Studies of the Struggle for Comprehensive Primary Health Care While impressive medical and technological developments have im- proved health care around the world, improvements in health have been moderate and inconsistent across countries and communities. In response to this challenge, the World Health Organization outlined the concept of comprehensive primary health care, which involves not only providing a range of medical care from prevention to treatment, but also working to improve equity in health care access, community em- powerment, the participation of marginalized groups, and collabora- tion across sectors beyond health. Revitalizing Health for All examines 13 cases of efforts to implement comprehensive primary health care reforms in communities around the globe, including in Australia, Brazil, Democratic Republic of Congo, South Africa, and Iran. The case studies originated from an international research-to-action initiative that brought researchers and research-users from national public health systems together to design, implement, and assess local projects. This volume reveals the similarities among com- prehensive primary health care projects in diverse national contexts and offers a rich evidence base from which future reform initiatives can draw. ronald labonté is a professor in the Faculty of Medicine at the University of Ottawa and the Faculty of Health Sciences at Flinders University. david sanders is a professor emeritus and founding director of the School of Public Health at the University of the Western Cape. corinne packer is a senior researcher in the Faculty of Medicine at the University of Ottawa. nikki schaay is a senior researcher in the School of Public Health at the University of the Western Cape. -

Collective Advanced Life Support Ambulance an Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response
Collective Advanced Life Support Ambulance An Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response Thierry Lentz SAMU 92 Charles Groizard SAMU 92 Abel Colomes SAMU 92 Anna Ozguler ( [email protected] ) INSERM https://orcid.org/0000-0002-9277-610X Michel Baer SAMU 92 Thomas Loeb SAMU 92 Research article Keywords: Emergency medical service, Critical care transport, Interhospital transfer of critically ill patients, Collective Transport, Mass casualty incidents, Disaster DOI: https://doi.org/10.21203/rs.3.rs-48425/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/14 Abstract Background: During the COVID-19 pandemic, as the number of available Intensive Care beds in France did not meet the needs, it appeared necessary to transfer a large number of patients from the most affected areas to the less ones. Mass transportation resources were deemed necessary. To achieve that goal, the concept of a Collective Advanced Life Support Ambulance (CALSA) was proposed in the form of a long-distance bus re-designed and equipped so as to accommodate up to six intensive care patients and allow Advanced Life Support (ALS) techniques to be performed while en route. Methods: The expected beneƒt of the CALSA, when compared to ALS ambulances accommodating a single patient, was to reduce the resources requirements, in particular by a lower personnel headcount for several patients being transferred to the same destination. A foreseen prospect, comparing to other collective transportation vectors such as airplanes, was the door-to-door capability, minimalizing patients’ handovers for safety concerns and time e∆ciency. -
Wisconsin Emergency Medical Services System Overview; a Call to Action
WISCONSIN EMERGENCY MEDICAL SERVICES SYSTEM OVERVIEW; A CALL TO ACTION Developed by EMS Stakeholders September, 2008 Approved by EMS Board 08/2008 EMS System Overview; A Call to Action EXECUTIVE SUMMARY The current state of the Emergency Medical Services (EMS) System and Trauma Care System are at risk of catastrophic failure. This document discusses the issues through a strengths, weaknesses, opportunities, and threats (SWOT) analysis of the system. Primarily the following are the main findings: Strengths‐ These are generally categorized as the number of volunteers that provide care, the dedicated stakeholders/providers, various committees providing network opportunities, a developing hospital and trauma system, EMS educational system, progressive scopes of practice for all level of providers, and the current funding assistance initiatives. Weaknesses‐ identified as workforce issues, lack of stable funding to support development and structure, no increase in funding assistance dollars since its inception, poor communication of information through the EMS industry adding to inadequate representation, lack of DHS/DPH support, lack of regional EMS support, and the geography of service areas. Opportunities ‐ a potential legislative council study, building consensus through stakeholder initiatives and consortia, potential restructuring of the systems, infrastructure to educate and promote EMS & Trauma, developing EMS & Trauma data systems. Threats‐ include inconsistent and inaccurate messages to the public and government leaders, Public perception, other special interest groups, strong ethics of the workforce, lack of stable funding, open administrative rules, DHS/DPH Management, all of which are representative of a failing EMS & Trauma infrastructure. The SWOT analysis is found to be directly associated with the 2001 National Highway Transportation Safety Administration (NHTSA). -

Final Bulletin-Format
Bulletin Michigan Department of Health and Human Services Bulletin Number: MSA 15-48 Distribution: Ambulance Providers, Hospitals, Medicaid Health Plans Issued: December 1, 2015 Subject: Medicaid Ambulance Policy Revisions Effective: January 1, 2016 Programs Affected: Medicaid, Healthy Michigan Plan, Children's Special Health Care Services The purpose of this bulletin is to clarify and amend Michigan Medicaid, Children's Special Health Care Services and Healthy Michigan Plan ambulance policy pertaining to Advanced Life Support (ALS) and base rate services, non-emergent air ambulance transports and neonatal emergency transports. This policy is effective for dates of service on and after December 1, 2015, and applies to Medicaid Fee-for Service. For beneficiaries enrolled in a Medicaid Health Plan (MHP), providers should contact the MHP for policy and coverage information. I. Advanced Life Support & Base Rate Services The determination to respond emergently with either an ALS or Basic Life Support (BLS) ambulance vehicle is dependent upon local 911 or equivalent service dispatch protocol. When a dispatch was inconsistent with this standard of protocol, or when no protocol was used, the beneficiary’s condition at the time of ambulance arrival determines the appropriate level of reimbursement. Even if a local government or medical control authority requires an ALS-level response to all calls, the base rate billed must reflect the level of service rendered and not the vehicle in which the beneficiary was transported. The furnishing of an ALS assessment without a medically necessary ALS intervention is sufficient to bill the ALS base rate if the beneficiary’s condition at the time of dispatch indicated an ALS level of service was required. -

Colorado Search and Rescue Fund
Colorado Search and Rescue Fund Frequently Asked Questions 1. What is the Colorado Search and Rescue Fund? The fund was created in 1987 for the purpose of reimbursing political subdivisions and search and rescue organizations for expenses incurred in conducting search and rescue operations within the State of Colorado. 2. How do I contribute to the Colorado Search and Rescue Fund? If you purchase fishing or hunting licenses, a stand-alone Colorado Wildlife Habitat Stamp, or register an off-highway vehicle, boat or snowmobile, you automatically contribute to the fund. Another way to contribute to the fund is by purchasing a Colorado Outdoor Recreation Search and Rescue Card. 3. What types of expenses are reimbursable under the Colorado Search and Rescue Fund? The fund reimburses on actual operating expenses incurred by local governments and teams during search and rescue missions. Those expenses include reasonable costs incidental to SAR activities such as: fuel, repair and rental of motor vehicles, fixed-wing aircraft, helicopters (when used for search and/or rescue not medical evacuation), snowmobiles, boats, horses, generators and any other equipment necessary or appropriate for conducting SAR activities; reimbursement of mileage at the appropriate state rate; meals and room rental for personnel and any other similar expenses. 4. Is the Colorado Search and Rescue Fund insurance? No, the fund is not an insurance program. It does not reimburse individuals for expenses incurred such as medical transport and medical expenses. Medical transport includes helicopter flights or ground ambulance. 5. Who manages the Colorado Search and Rescue Fund? Responsibility for management of the Colorado Search and Rescue Fund lies with the Colorado Department of Local Affairs.