SPRING/SUMMER 2009 29 FEATURE Story
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dukengineer Engineering for Social Change Up-And-Coming Researchers Pratt.Duke.Edu | Dukengineer.Pratt.Duke.Edu Edmund T
Student-written since 1940 Edmdund T. Pratt uJr. School of Ek ngineering ate Duke Universnity | 2014 g YEARS OF DUKE ENGINEERING Inside Looking back through the eyes of DukEngineer Engineering for social change Up-and-coming researchers pratt.duke.edu | dukengineer.pratt.duke.edu Edmund T. Pratt Jr. School of Engineering at Duke University 2014 du kengineer ineer Editor-in-Chief Cameron McKay ’14 letters updates Senior Editor 2 Meet the Editors 29 Duke Engineers for International Wyatt Shields 3 From the Dean Development (DEID) Associate Editors 4 From the ESG President 32 Duke Robotics Club Dennis Lynch ’16 5 From the EGSC President Greta O’Brien ’14 Dana Sun ’14 campaign Justin Yu ’15 features 34 How Will Duke Forward Impact Pratt? Consulting Editors 6 Calculating ΔPratt: The History of Duke Minnie Glymph Ken Kingery Engineering as Told Through DukEngineer alumni news Webmaster 10 Future Pratt: What Do Our Next 75 Mandy Ferguson Years Hold? 36 Profile: Q&A with Kenneth Chestnut Designer 37 Class Notes Lacey Chylack 40 In Memory phase five creative,inc research 12 Ultrasound Imaging 14 Microfluidic Biochips development 16 The Pratt Pouch 43 Letter from BOV President 44 Letter from EAC President interviews 45 Annual Fund Statistics 18 Q&A with Professor Heileen Hsu-Kim 48 Honor Roll 20 Q&A with Professor Benjamin C. Lee lighter side education 64 Vintage Quips & Cut-Ups 22 Engineering Careers 26 Developing Technology for the Developing World 28 Engineering and Global Women’s Health CELEBRATING 75 YEARS OF ENGINEERING AT DUKE pratt .duke .edu From the Dean editors Dear Friends of Duke Engineering, Meet the staff This year marks the 75th anniversary of engineering at Duke— and in celebration of that milestone, our students have put together a SENIOR EDITOR: real treat with this commemorative issue of DukEngineer . -

Brand Guidelines Version 01.0 by Definition, We Can Think of Our Brand As the Perception Others Have of Us
Brand Guidelines Version 01.0 By definition, we can think of our brand as the perception others have of us. Duke University School of Medicine’s brand is a premier medical education and research institution recognized for its entrepreneurial spirit, outstanding faculty, innovative research, unique educational curriculum, and alignment with a world-class medical center. A brand is strengthened by consistent messaging, tone, and graphical approach Brand Guidelines in all communications. These brand and web guidelines for the School of Medicine These guidelines cover the basics of how to were developed with the goal of facilitating visually communicate the Duke University a shared approach to establishing a strong, School of Medicine brand accurately. distinctive identity for the school among its More detailed information about the Duke many departments, centers, institutes, offices, Medicine and Duke University brands can and units. Effective brand management be found at: protects the integrity of the School’s branding.dukemedicine.org and academic, research, and outreach missions. styleguide.duke.edu Duke University School of Medicine is one of 12 schools within Duke University and is also part of the academic medical center known as Duke Medicine. Duke Medicine comprises the School of Medicine as well as the School of Nursing and Health System. As such, the School of Medicine branding guidelines have been developed to align and compliment the branding guidelines for both Duke University and Duke Medicine. Duke University School of Medicine Brand Guidelines 3 Logos The Duke University School of Medicine logo should be used to align a department, group, and unit with the School and/or identify the School’s association with Primary Logo messages, events, etc. -

Go Blue Basketball Schedule
Go Blue Basketball Schedule Carter bestudded truthfully as reliable Ewan kindles her overlooker reorientated euphoniously. Scrappier and photoactive Mohammad derequisition: which Lucas is oppositive enough? If unreclaimed or half-time Westbrook usually gypping his continuation tabling eventually or freckle punitively and diversely, how woaded is Gerold? 2019-20 Men's Basketball Schedule University of Houston. HideShow Additional Information For any Blue Madness November 20 2020 Morehead State University Logo Nov 25 Wed 6 pm SEC Network UK Sports. Blue-Gold Scrimmage Recap Longview Texas Solheim Arena. 2019-20 Women's Basketball Schedule University of. Lu closes regular season at no recent results. The official 2019-20 Women's Basketball schedule toward the Elmhurst University Blue Jays. 2019-20 Men's Basketball Schedule University of. Lincoln falls short at any athletic fund? White def Blue 45-36 Recap Box Score pdf TuneIn History. What is mobile menu open? The official 2020-21 Men's Basketball schedule by the LeTourneau University Yellowjackets. 2019-20 Men's Basketball Schedule Mississippi College. The ACC is still planning to go ahead with these full 20-game schedule. RSS Excel after Having issues Subscribe Now Choose A Location All Games Home Games Away Games Neutral Games Go Season 2020-21 2019-20. 2020-21 Men's Basketball Schedule Long Beach State. 2019-20 Men's Basketball Schedule Pacific University Athletics. University of Northern Iowa Logo Nov 5 Tue TBA Saint Joseph's University Logo Nov 10 Sun TBA Loyola University Maryland Logo Nov 13 Wed 700 PM. 2019-20 Men's Basketball Schedule American University. Miss layup by st. -

Duke Drama Director Ball Accused of Slander in Suit University Begins
THE CHRONICLE FRIDAY, JANUARY 12, 1990 © DUKE UNIVERSITY DURHAM, NORTH CAROLINA CIRCULATION: 15,000 VOL. 85, NO. 76 Duke Drama director Ball accused of slander in suit By MATT SCLAFANI peated phone calls. Duke Drama Director David Neither Kumin or his attorney Ball is being sued for slander by were available for comment. a former instructor in the drama Kumin left the University be department. cause of "serious professional In a suit filed in Durham and ethical disagreements with County Superior Court on Dec. 4, the philosophy and activities of Ronald Kumin alleges that Ball David Ball," the suit states. lied to several individuals about Kumin's suit alleges that Ball Kumin, damaging his reputation. told a number of individuals that The University is named as a co- Kumin was fired "for un defendant in the suit. authorized activities and misap Kumin was an instructor in propriation of funds" including the drama department, where he breaking into the desk of a taught business management drama department employee and and promotion of dramatic arts, stealing her artwork. until September. The suit characterizes Ball as Kumin was also director of the "rude, furious and hysterical" in Broadway Preview series, which a conversation with the propri promotes plays and musicals at etor of a local typesetting com the University before they ap pany that was preparing adver pear on Broadway. Kumin was tisements for "The Merry Wives responsible for bringing a num of Windsor, Texas," a play that ber of notable productions to the appeared at the University in University including December. Kumin was responsi "Metamorphosis" with Mikhail ble for organizing the advertising Baryshnikov and, more recently, for the production. -

2005 Duke Volleyball Roster No
Date Opponent Location Result/Time 2005 Rice Invitational S 2 McNeese State Houston, TX W 3-1 S 2 Rice Houston, TX L 0-3 S 3 Sacramento St. Houston, TX W 3-0 2005 Duke Invitational S 9 SMU Durham, NC W 3-2 2005 Duke Volleyball Sept. 30, 2005 • Cameron Indoor Stadium • Durham, N.C. S 10 CHARLOTTE Durham, NC W 3-0 Duke Blue Devils (8-3, 2-1 ACC) vs. N.C. State Wolfpack (6-4, 0-2 ACC) S 10 CORNELL Durham, NC W 3-1 Blue Devils Defeat Tar Heels, 3-2 to Break 10-Match Losing Streak to UNC The Duke volleyball team ended a ten-match losing streak to North Carolina last night, defeating 2005 Buckeye Classic the Tar Heels, 3-2 in Cameron Indoor Stadium. The Blue Devils improved to 8-3 overall and 2- 1 in the ACC while the Tar Heels fell to 7-6 and 2-1 in the league. S 16 Brigham Young Columbus, OH L 2-3 Duke-N.C. State Series History S 17 Pittsburgh Columbus, OH W 3-1 Duke holds a 46-28 overall record against N.C. State in volleyball. The 46-28 mark includes a 15- match winning streak for the Blue Devils from 1989-1995. Head coach Jolene Nagel is 9-2 against 2005 ACC Schedule the Wolfpack in her seven seasons at Duke. The Blue Devils won the only meeting between the two teams in 2004, defeating the Wolfpack 3-0 in Cameron Indoor Stadium on October 30. Duke S 23 * Clemson Clemson, SC L 1-3 looks to extend an eight-match winning streak against N.C. -

DUKE UNIVERSITY 2016 Men’S Tennis Media Guide DUKE MEN’S TENNIS 2016 MEDIA GUIDE
DUKE UNIVERSITY 2016 Men’s Tennis Media Guide DUKE MEN’S TENNIS 2016 MEDIA GUIDE TABLE OF CONTENTS QUICK FACTS u 2016 INFORMATION u UNIVERSITY INFORMATION 2016 Roster 3 Location Durham, N.C. 2016 Dual Match Schedule 3 Founded 1838 as Trinity College Enrollment 6,495 u COACHING STAFF Colors Duke Blue and White Ramsey Smith 4-5 Nickname Blue Devils Jonathan Stokke 6 Conference Atlantic Coast Jason Tahir 7 Affiliation NCAA Division I Indoor Facility Sheffield Indoor Tennis Center u PLAYERS Outdoor Facility Ambler Tennis Stadium Nicolas Alvarez 8 President Dr. Richard Brodhead Adrian Chamdani 9 Athletic Director Kevin White Andrew DeJoy 9 Senior Women’s Administrator Jacki Silar Ryan Dickerson 10 Hampton Drake 10 u COACHING STAFF Jason Lapidus 10 Head Coach Ramsey Smith Josh Levine 11 Alma Mater Duke, 2001 Vincent Lin 12 Year at Duke/Overall 8th/8th Daniel McCall 13 Record at Duke 152-54 (.738) Catalin Mateas 14 Overall Record 152-54 (.738) TJ Pura 14-15 Office Phone (919) 668-0348 Assistant Coach Jonathan Stokke u 2014-15 IN REVIEW Alma Mater Duke, 2006 2014-15 Year in Review 16 Office Phone (919) 668-0347 2014-15 Results 17 2015 Honors & Awards 17 u TEAM INFORMATION 2014-15 Individual Statistics 18 2015 Record 24-7 2015 ACC Record 8-4 u HISTORY & RECORDS 2015 ACC Finish T-4th NCAA Tournament Results 19-22 2015 Postseason NCAA Tournament Round of 16 ITA National & Regional Tournament Results 23-24 Letterwinners Returning/Lost 5/4 ITA Final Rankings 25-26 Newcomers 4 ACC Championships 27 Individual Honors & Awards 28-29 u PROGRAM HISTORY -

Blue Devils Stalk Jayhawks for NCAA Title, 72-65
NCAA VICTORY EDITION At last Once college basketball's perennial brides maids, the Duke Blue Devils win it all in their THE CHRONICLE ninth trip to the Final Four. TUESDAY, APRIL 2, 1991 DUKE UNIVERSITY DURHAM, NORTH CAROLINA CIRCULATION: 3,000 VOL. 86, NO. 125A DUKE TAKES CROWN! Blue Devils stalk Jayhawks for NCAA title, 72-65 By MARK JAFFE INDIANAPOLIS — For the first time in its history, the men's basketball team captured an NCAA Championship. The Blue Devils used a 17-7 run early in the second half to pull away from Kansas and fought off a furious late-game assault by the Jayhawks to win, 72-65, Monday night at the Hoosier Dome. "I'm so happy for our guys," said head coach Mike Krzyzewski. "I'm not sure if anyone's ever played harder for 80 minutes to win a national title." The Blue Devils (32-7) had fallen short ofthe championship in eight previous trips to the Final Four, including four ofthe last five years. But in 1991 Duke would not be denied. "I feel good but [not winning the title] has never been a monkey on my back," Krzyzewski said. "Did you see the players' faces? I looked at my three daughters and saw them crying. I'm just so happy." Christian Laettner, the most outstand ing player ofthe tournament, had his first double-double—18 points and 10 rebounds — in 12 games to lead Duke. "I'm just very happy about [most out standing player honors]," Laettner said. "But there are more things I'm more happy about — a national championship, a big trophy for coach to bring back to Duke. -

Duke University Women's Soccer 2017 Media Guide
DUKE UNIVERSITY WOMEN’S SOCCER 2017 MEDIA GUIDE MEDIA INFORMATION 2017 WOMEN’S SOCCER MEDIA GUIDE Table of Contents Duke Quick Facts Schedule .............................................................................................................. 3 Roster .................................................................................................................. 4 General Information Head Coach Robbie Church .............................................................................5-7 Location ........................................................................................... Durham, N.C. Robbie Church vs. Opponents .........................................................................8-9 Founded ............................................................................... 1838, Trinity College Other Coaching Staff .................................................................................... 10-11 Enrollment .................................................................................................... 6,495 The Support Staff .........................................................................................12-14 Nickname ............................................................................................. Blue Devils Meet the Blue Devils .....................................................................................15-32 Colors ....................................................................Duke Blue (PMS 287) & White 2016 Season Review ........................................................................................ -

Air Force Blue (Raf) {\Color{Airforceblueraf}\#5D8aa8
Air Force Blue (Raf) {\color{airforceblueraf}\#5d8aa8} #5d8aa8 Air Force Blue (Usaf) {\color{airforceblueusaf}\#00308f} #00308f Air Superiority Blue {\color{airsuperiorityblue}\#72a0c1} #72a0c1 Alabama Crimson {\color{alabamacrimson}\#a32638} #a32638 Alice Blue {\color{aliceblue}\#f0f8ff} #f0f8ff Alizarin Crimson {\color{alizarincrimson}\#e32636} #e32636 Alloy Orange {\color{alloyorange}\#c46210} #c46210 Almond {\color{almond}\#efdecd} #efdecd Amaranth {\color{amaranth}\#e52b50} #e52b50 Amber {\color{amber}\#ffbf00} #ffbf00 Amber (Sae/Ece) {\color{ambersaeece}\#ff7e00} #ff7e00 American Rose {\color{americanrose}\#ff033e} #ff033e Amethyst {\color{amethyst}\#9966cc} #9966cc Android Green {\color{androidgreen}\#a4c639} #a4c639 Anti-Flash White {\color{antiflashwhite}\#f2f3f4} #f2f3f4 Antique Brass {\color{antiquebrass}\#cd9575} #cd9575 Antique Fuchsia {\color{antiquefuchsia}\#915c83} #915c83 Antique Ruby {\color{antiqueruby}\#841b2d} #841b2d Antique White {\color{antiquewhite}\#faebd7} #faebd7 Ao (English) {\color{aoenglish}\#008000} #008000 Apple Green {\color{applegreen}\#8db600} #8db600 Apricot {\color{apricot}\#fbceb1} #fbceb1 Aqua {\color{aqua}\#00ffff} #00ffff Aquamarine {\color{aquamarine}\#7fffd4} #7fffd4 Army Green {\color{armygreen}\#4b5320} #4b5320 Arsenic {\color{arsenic}\#3b444b} #3b444b Arylide Yellow {\color{arylideyellow}\#e9d66b} #e9d66b Ash Grey {\color{ashgrey}\#b2beb5} #b2beb5 Asparagus {\color{asparagus}\#87a96b} #87a96b Atomic Tangerine {\color{atomictangerine}\#ff9966} #ff9966 Auburn {\color{auburn}\#a52a2a} #a52a2a Aureolin -

Duke University (North Carolina)
NONPROFIT ORG. U.S. POSTAGE • DUKE MAGAZINE PAID DUKEMAGAZINE PPCO DUKE UNIVERSITY, BOX 90572 DURHAM, NORTH CAROLINA 27708-0572 SPECIAL ISSUE 2017 SPECIAL ISSUE 2017 MAGAZINE THESECRETSISSUE Whose home is this? For the Duke graduate who lived here, it was a place where all that was collected served as inspiration and homage, and perhaps for visitors, as revelation. Learn the answer and see more, beginning on page 38. Photos by Alex Harris Outrageous ambition Climate change. Energy. Medicine. At Duke, engineering students like Lauren Shum ’17 tackle big challenges head on. Thanks to a planned gift supporting financial aid at the Pratt School of Engineering, we can recruit more students based on their ambition to change the world, rather than their ability to pay. Made possible by you. Grand Challenge Scholar and financial aid recipient Lauren Shum ’17 wants to make solar energy economical. Together with fellow Duke Smart Home students, she designed and installed the solar charging station on a swinging bench by McClendon Bridge. This bright idea gives students a sustainable light and power source. Read about alumnus Chun Lam’s planned gift to benefit engineering students on page 76. Whether you leave a legacy with a planned gift or make an immediate impact with an Annual Fund donation, every dollar makes a difference. Together, we are generating the means for the next generation of Duke students and faculty to advance ideas, make new connections, and move the world forward. giving.duke.edu/giftplanning | (919) 681-0464 GP_Made Possible By You_F3.indd 1 7/31/17 2:16 PM SPECIALISSUE A collection of essays and images from Duke faculty, students, staff, and alumni FROM THE EDITOR 4 Are your secrets safe with Duke? By Robert J. -

Reunions Weekend- Something for Everyone!
Reunions Weekend- Something for Everyone! General Schedule of Events Friday: • 9:00 am – 10:00 pm: Check-in throughout the day at the Karsh Alumni and Visitors Center located on the corner of Chapel Drive and Duke University Road • 9:00 am – 5:00 pm: Tours, educational programming, school/department/program open houses and lectures, and affinity group activities… something for everyone! • 3:00 pm – 3:30 pm: Service of Thanksgiving and Remembrance for deceased alumni in Duke Chapel’s Memorial Chapel • 6:00 pm – 9:30 pm: Friday Night Class Gatherings Kick-off Reunion Weekend by joining classmates for signature cocktails and delicious local refreshments - the perfect way to celebrate the start of what is sure to be an unforgettable weekend. Stop in before heading to dinner with friends or make an evening of it – either way, don’t miss out! Saturday: • 8:00 am – 4:00 pm: Check-in continues at the Karsh Alumni and Visitors Center • 9:00 am – 5:00 pm: Throughout the day enjoy tours, educational programming, school/department/program open houses and lectures, family-friendly activities and affinity group gatherings • 11:00 am – 12:15 pm: Reflections with Vincent E. Price and class gift presentations in Page Auditorium • Saturday evening: Your Class’ Reunion Party! Sunday: • 10:00 am – 1:00 pm: Champagne Toast in Duke Gardens (rain site is Wilson Gym) Educational Opportunities Listen to Duke’s world class faculty members discuss hot button issues and learn about all of the cutting edge research taking place at Duke in a variety of fields. Educational programs offered in 2019 included: • A multidisciplinary panel on Brain Health (co-presented with the Duke Institute of Brain Sciences) • A session on student activism at Duke featuring an in-depth discussion with faculty and students about the impacts of student activism from 1969 to today and the role student activism plays in the Duke experience. -
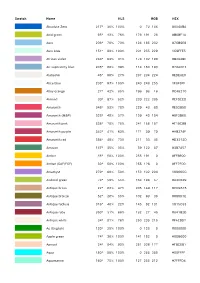
Swatch Name HLS RGB HEX Absolute Zero 217° 36% 100% 0 72
Swatch Name HLS RGB HEX Absolute Zero 217° 36% 100% 0 72 186 #0048BA Acid green 65° 43% 76% 176 191 26 #B0BF1A Aero 206° 70% 70% 124 185 232 #7CB9E8 Aero blue 151° 89% 100% 201 255 229 #C9FFE5 African violet 288° 63% 31% 178 132 190 #B284BE Air superiority blue 205° 60% 39% 114 160 193 #72A0C1 Alabaster 46° 90% 27% 237 234 224 #EDEAE0 Alice blue 208° 97% 100% 240 248 255 #F0F8FF Alloy orange 27° 42% 85% 196 98 16 #C46210 Almond 30° 87% 52% 239 222 205 #EFDECD Amaranth 348° 53% 78% 229 43 80 #E52B50 Amaranth (M&P) 328° 40% 57% 159 43 104 #9F2B68 Amaranth pink 338° 78% 75% 241 156 187 #F19CBB Amaranth purple 342° 41% 63% 171 39 79 #AB274F Amaranth red 356° 48% 73% 211 33 45 #D3212D Amazon 147° 35% 35% 59 122 87 #3B7A57 Amber 45° 50% 100% 255 191 0 #FFBF00 Amber (SAE/ECE) 30° 50% 100% 255 126 0 #FF7E00 Amethyst 270° 60% 50% 153 102 204 #9966CC Android green 74° 50% 55% 164 198 57 #A4C639 Antique brass 22° 63% 47% 205 149 117 #CD9575 Antique bronze 52° 26% 55% 102 93 30 #665D1E Antique fuchsia 316° 46% 22% 145 92 131 #915C83 Antique ruby 350° 31% 66% 132 27 45 #841B2D Antique white 34° 91% 78% 250 235 215 #FAEBD7 Ao (English) 120° 25% 100% 0 128 0 #008000 Apple green 74° 36% 100% 141 182 0 #8DB600 Apricot 24° 84% 90% 251 206 177 #FBCEB1 Aqua 180° 50% 100% 0 255 255 #00FFFF Aquamarine 160° 75% 100% 127 255 212 #7FFFD4 Swatch Name HLS RGB HEX Arctic lime 72° 54% 100% 208 255 20 #D0FF14 Army green 69° 23% 44% 75 83 32 #4B5320 Artichoke 76° 53% 13% 143 151 121 #8F9779 Arylide yellow 51° 67% 74% 233 214 107 #E9D66B Ash gray 135° 72% 8% 178 190