The American Society of Echocardiography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thermodynamics of Spacetime: the Einstein Equation of State
gr-qc/9504004 UMDGR-95-114 Thermodynamics of Spacetime: The Einstein Equation of State Ted Jacobson Department of Physics, University of Maryland College Park, MD 20742-4111, USA [email protected] Abstract The Einstein equation is derived from the proportionality of entropy and horizon area together with the fundamental relation δQ = T dS connecting heat, entropy, and temperature. The key idea is to demand that this relation hold for all the local Rindler causal horizons through each spacetime point, with δQ and T interpreted as the energy flux and Unruh temperature seen by an accelerated observer just inside the horizon. This requires that gravitational lensing by matter energy distorts the causal structure of spacetime in just such a way that the Einstein equation holds. Viewed in this way, the Einstein equation is an equation of state. This perspective suggests that it may be no more appropriate to canonically quantize the Einstein equation than it would be to quantize the wave equation for sound in air. arXiv:gr-qc/9504004v2 6 Jun 1995 The four laws of black hole mechanics, which are analogous to those of thermodynamics, were originally derived from the classical Einstein equation[1]. With the discovery of the quantum Hawking radiation[2], it became clear that the analogy is in fact an identity. How did classical General Relativity know that horizon area would turn out to be a form of entropy, and that surface gravity is a temperature? In this letter I will answer that question by turning the logic around and deriving the Einstein equation from the propor- tionality of entropy and horizon area together with the fundamental relation δQ = T dS connecting heat Q, entropy S, and temperature T . -

4B. the Heart (Cor) 1
Henry Gray (1821–1865). Anatomy of the Human Body. 1918. 4b. The Heart (Cor) 1 The heart is a hollow muscular organ of a somewhat conical form; it lies between the lungs in the middle mediastinum and is enclosed in the pericardium (Fig. 490). It is placed obliquely in the chest behind the body of the sternum and adjoining parts of the rib cartilages, and projects farther into the left than into the right half of the thoracic cavity, so that about one-third of it is situated on the right and two-thirds on the left of the median plane. Size.—The heart, in the adult, measures about 12 cm. in length, 8 to 9 cm. in breadth at the 2 broadest part, and 6 cm. in thickness. Its weight, in the male, varies from 280 to 340 grams; in the female, from 230 to 280 grams. The heart continues to increase in weight and size up to an advanced period of life; this increase is more marked in men than in women. Component Parts.—As has already been stated (page 497), the heart is subdivided by 3 septa into right and left halves, and a constriction subdivides each half of the organ into two cavities, the upper cavity being called the atrium, the lower the ventricle. The heart therefore consists of four chambers, viz., right and left atria, and right and left ventricles. The division of the heart into four cavities is indicated on its surface by grooves. The atria 4 are separated from the ventricles by the coronary sulcus (auriculoventricular groove); this contains the trunks of the nutrient vessels of the heart, and is deficient in front, where it is crossed by the root of the pulmonary artery. -
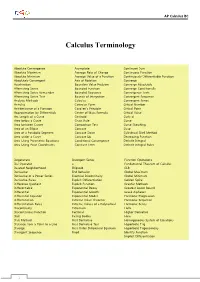
Calculus Terminology
AP Calculus BC Calculus Terminology Absolute Convergence Asymptote Continued Sum Absolute Maximum Average Rate of Change Continuous Function Absolute Minimum Average Value of a Function Continuously Differentiable Function Absolutely Convergent Axis of Rotation Converge Acceleration Boundary Value Problem Converge Absolutely Alternating Series Bounded Function Converge Conditionally Alternating Series Remainder Bounded Sequence Convergence Tests Alternating Series Test Bounds of Integration Convergent Sequence Analytic Methods Calculus Convergent Series Annulus Cartesian Form Critical Number Antiderivative of a Function Cavalieri’s Principle Critical Point Approximation by Differentials Center of Mass Formula Critical Value Arc Length of a Curve Centroid Curly d Area below a Curve Chain Rule Curve Area between Curves Comparison Test Curve Sketching Area of an Ellipse Concave Cusp Area of a Parabolic Segment Concave Down Cylindrical Shell Method Area under a Curve Concave Up Decreasing Function Area Using Parametric Equations Conditional Convergence Definite Integral Area Using Polar Coordinates Constant Term Definite Integral Rules Degenerate Divergent Series Function Operations Del Operator e Fundamental Theorem of Calculus Deleted Neighborhood Ellipsoid GLB Derivative End Behavior Global Maximum Derivative of a Power Series Essential Discontinuity Global Minimum Derivative Rules Explicit Differentiation Golden Spiral Difference Quotient Explicit Function Graphic Methods Differentiable Exponential Decay Greatest Lower Bound Differential -
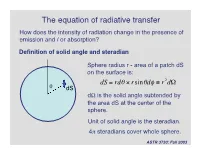
The Equation of Radiative Transfer How Does the Intensity of Radiation Change in the Presence of Emission and / Or Absorption?
The equation of radiative transfer How does the intensity of radiation change in the presence of emission and / or absorption? Definition of solid angle and steradian Sphere radius r - area of a patch dS on the surface is: dS = rdq ¥ rsinqdf ≡ r2dW q dS dW is the solid angle subtended by the area dS at the center of the † sphere. Unit of solid angle is the steradian. 4p steradians cover whole sphere. ASTR 3730: Fall 2003 Definition of the specific intensity Construct an area dA normal to a light ray, and consider all the rays that pass through dA whose directions lie within a small solid angle dW. Solid angle dW dA The amount of energy passing through dA and into dW in time dt in frequency range dn is: dE = In dAdtdndW Specific intensity of the radiation. † ASTR 3730: Fall 2003 Compare with definition of the flux: specific intensity is very similar except it depends upon direction and frequency as well as location. Units of specific intensity are: erg s-1 cm-2 Hz-1 steradian-1 Same as Fn Another, more intuitive name for the specific intensity is brightness. ASTR 3730: Fall 2003 Simple relation between the flux and the specific intensity: Consider a small area dA, with light rays passing through it at all angles to the normal to the surface n: n o In If q = 90 , then light rays in that direction contribute zero net flux through area dA. q For rays at angle q, foreshortening reduces the effective area by a factor of cos(q). -

Area of Polygons and Complex Figures
Geometry AREA OF POLYGONS AND COMPLEX FIGURES Area is the number of non-overlapping square units needed to cover the interior region of a two- dimensional figure or the surface area of a three-dimensional figure. For example, area is the region that is covered by floor tile (two-dimensional) or paint on a box or a ball (three- dimensional). For additional information about specific shapes, see the boxes below. For additional general information, see the Math Notes box in Lesson 1.1.2 of the Core Connections, Course 2 text. For additional examples and practice, see the Core Connections, Course 2 Checkpoint 1 materials or the Core Connections, Course 3 Checkpoint 4 materials. AREA OF A RECTANGLE To find the area of a rectangle, follow the steps below. 1. Identify the base. 2. Identify the height. 3. Multiply the base times the height to find the area in square units: A = bh. A square is a rectangle in which the base and height are of equal length. Find the area of a square by multiplying the base times itself: A = b2. Example base = 8 units 4 32 square units height = 4 units 8 A = 8 · 4 = 32 square units Parent Guide with Extra Practice 135 Problems Find the areas of the rectangles (figures 1-8) and squares (figures 9-12) below. 1. 2. 3. 4. 2 mi 5 cm 8 m 4 mi 7 in. 6 cm 3 in. 2 m 5. 6. 7. 8. 3 units 6.8 cm 5.5 miles 2 miles 8.7 units 7.25 miles 3.5 cm 2.2 miles 9. -

Right Triangles and the Pythagorean Theorem Related?
Activity Assess 9-6 EXPLORE & REASON Right Triangles and Consider △ ABC with altitude CD‾ as shown. the Pythagorean B Theorem D PearsonRealize.com A 45 C 5√2 I CAN… prove the Pythagorean Theorem using A. What is the area of △ ABC? Of △ACD? Explain your answers. similarity and establish the relationships in special right B. Find the lengths of AD‾ and AB‾ . triangles. C. Look for Relationships Divide the length of the hypotenuse of △ ABC VOCABULARY by the length of one of its sides. Divide the length of the hypotenuse of △ACD by the length of one of its sides. Make a conjecture that explains • Pythagorean triple the results. ESSENTIAL QUESTION How are similarity in right triangles and the Pythagorean Theorem related? Remember that the Pythagorean Theorem and its converse describe how the side lengths of right triangles are related. THEOREM 9-8 Pythagorean Theorem If a triangle is a right triangle, If... △ABC is a right triangle. then the sum of the squares of the B lengths of the legs is equal to the square of the length of the hypotenuse. c a A C b 2 2 2 PROOF: SEE EXAMPLE 1. Then... a + b = c THEOREM 9-9 Converse of the Pythagorean Theorem 2 2 2 If the sum of the squares of the If... a + b = c lengths of two sides of a triangle is B equal to the square of the length of the third side, then the triangle is a right triangle. c a A C b PROOF: SEE EXERCISE 17. Then... △ABC is a right triangle. -

Calculus Formulas and Theorems
Formulas and Theorems for Reference I. Tbigonometric Formulas l. sin2d+c,cis2d:1 sec2d l*cot20:<:sc:20 +.I sin(-d) : -sitt0 t,rs(-//) = t r1sl/ : -tallH 7. sin(A* B) :sitrAcosB*silBcosA 8. : siri A cos B - siu B <:os,;l 9. cos(A+ B) - cos,4cos B - siuA siriB 10. cos(A- B) : cosA cosB + silrA sirrB 11. 2 sirrd t:osd 12. <'os20- coS2(i - siu20 : 2<'os2o - I - 1 - 2sin20 I 13. tan d : <.rft0 (:ost/ I 14. <:ol0 : sirrd tattH 1 15. (:OS I/ 1 16. cscd - ri" 6i /F tl r(. cos[I ^ -el : sitt d \l 18. -01 : COSA 215 216 Formulas and Theorems II. Differentiation Formulas !(r") - trr:"-1 Q,:I' ]tra-fg'+gf' gJ'-,f g' - * (i) ,l' ,I - (tt(.r))9'(.,') ,i;.[tyt.rt) l'' d, \ (sttt rrJ .* ('oqI' .7, tJ, \ . ./ stll lr dr. l('os J { 1a,,,t,:r) - .,' o.t "11'2 1(<,ot.r') - (,.(,2.r' Q:T rl , (sc'c:.r'J: sPl'.r tall 11 ,7, d, - (<:s<t.r,; - (ls(].]'(rot;.r fr("'),t -.'' ,1 - fr(u") o,'ltrc ,l ,, 1 ' tlll ri - (l.t' .f d,^ --: I -iAl'CSllLl'l t!.r' J1 - rz 1(Arcsi' r) : oT Il12 Formulas and Theorems 2I7 III. Integration Formulas 1. ,f "or:artC 2. [\0,-trrlrl *(' .t "r 3. [,' ,t.,: r^x| (' ,I 4. In' a,,: lL , ,' .l 111Q 5. In., a.r: .rhr.r' .r r (' ,l f 6. sirr.r d.r' - ( os.r'-t C ./ 7. /.,,.r' dr : sitr.i'| (' .t 8. tl:r:hr sec,rl+ C or ln Jccrsrl+ C ,f'r^rr f 9. -

Abnormally Enlarged Singular Thebesian Vein in Right Atrium
Open Access Case Report DOI: 10.7759/cureus.16300 Abnormally Enlarged Singular Thebesian Vein in Right Atrium Dilip Kumar 1 , Amit Malviya 2 , Bishwajeet Saikia 3 , Bhupen Barman 4 , Anunay Gupta 5 1. Cardiology, Medica Institute of Cardiac Sciences, Kolkata, IND 2. Cardiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 3. Anatomy, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 4. Internal Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 5. Cardiology, Vardhman Mahavir Medical College (VMMC) and Safdarjung Hospital, New Delhi, IND Corresponding author: Amit Malviya, [email protected] Abstract Thebesian veins in the heart are subendocardial venoluminal channels and are usually less than 0.5 mm in diameter. The system of TV either opens a venous (venoluminal) or an arterial (arterioluminal) channel directly into the lumen of the cardiac chambers or via some intervening spaces (venosinusoidal/ arteriosinusoidal) termed as sinusoids. Enlarged thebesian veins are reported in patients with congenital heart disease and usually, multiple veins are enlarged. Very few reports of such abnormal enlargement are there in the absence of congenital heart disease, but in all such cases, they are multiple and in association with coronary artery microfistule. We report a very rare case of a singular thebesian vein in the right atrium, which was abnormally enlarged. It is important to recognize because it can be confused with other cardiac structures like coronary sinus during diagnostic or therapeutic catheterization and can lead to cardiac injury and complications if it is attempted to cannulate it or pass the guidewires. -

Difference Between Angular Momentum and Pseudoangular
Difference between angular momentum and pseudoangular momentum Simon Streib Department of Physics and Astronomy, Uppsala University, Box 516, SE-75120 Uppsala, Sweden (Dated: March 16, 2021) In condensed matter systems it is necessary to distinguish between the momentum of the con- stituents of the system and the pseudomomentum of quasiparticles. The same distinction is also valid for angular momentum and pseudoangular momentum. Based on Noether’s theorem, we demonstrate that the recently discussed orbital angular momenta of phonons and magnons are pseudoangular momenta. This conceptual difference is important for a proper understanding of the transfer of angular momentum in condensed matter systems, especially in spintronics applications. In 1915, Einstein, de Haas, and Barnett demonstrated experimentally that magnetism is fundamentally related to angular momentum. When changing the magnetiza- tion of a magnet, Einstein and de Haas observed that the magnet starts to rotate, implying a transfer of an- (a) gular momentum from the magnetization to the global rotation of the lattice [1], while Barnett observed the in- verse effect, magnetization by rotation [2]. A few years later in 1918, Emmy Noether showed that continuous (b) symmetries imply conservation laws [3], such as the con- servation of momentum and angular momentum, which links magnetism to the most fundamental symmetries of nature. Condensed matter systems support closely related con- Figure 1. (a) Invariance under rotations of the whole system servation laws: the conservation of the pseudomomentum implies conservation of angular momentum, while (b) invari- and pseudoangular momentum of quasiparticles, such as ance under rotations of fields with a fixed background implies magnons and phonons. -

Residential Square Footage Guidelines
R e s i d e n t i a l S q u a r e F o o t a g e G u i d e l i n e s North Carolina Real Estate Commission North Carolina Real Estate Commission P.O. Box 17100 • Raleigh, North Carolina 27619-7100 Phone 919/875-3700 • Web Site: www.ncrec.gov Illustrations by David Hall Associates, Inc. Copyright © 1999 by North Carolina Real Estate Commission. All rights reserved. 7,500 copies of this public document were printed at a cost of $.000 per copy. • REC 3.40 11/1/2013 Introduction It is often said that the three most important factors in making a home buying decision are “location,” “location,” and “location.” Other than “location,” the single most-important factor is probably the size or “square footage” of the home. Not only is it an indicator of whether a particular home will meet a homebuyer’s space needs, but it also affords a convenient (though not always accurate) method for the buyer to estimate the value of the home and compare it to other properties. Although real estate agents are not required by the Real Estate License Law or Real Estate Commission rules to report the square footage of properties offered for sale (or rent), when they do report square footage, it is essential that the information they give prospective purchasers (or tenants) be accurate. At a minimum, information concerning square footage should include the amount of living area in the dwelling. The following guidelines and accompanying illustrations are designed to assist real estate brokers in measuring, calculating and reporting (both orally and in writing) the living area contained in detached and attached single-family residential buildings. -

04. the Cardiac Cycle/Wiggers Diagram
Part I Anaesthesia Refresher Course – 2018 4 University of Cape Town The Cardiac Cycle The “Wiggers diagram” Prof. Justiaan Swanevelder Dept of Anaesthesia & Perioperative Medicine University of Cape Town Each cardiac cycle consists of a period of relaxation (diastole) followed by ventricular contraction (systole). During diastole the ventricles are relaxed to allow filling. In systole the right and left ventricles contract, ejecting blood into the pulmonary and systemic circulations respectively. Ventricles The left ventricle pumps blood into the systemic circulation via the aorta. The systemic vascular resistance (SVR) is 5–7 times greater than the pulmonary vascular resistance (PVR). This makes it a high-pressure system (compared with the pulmonary vascular system), which requires a greater mechanical power output from the left ventricle (LV). The free wall of the LV and the interventricular septum form the bulk of the muscle mass in the heart. A normal LV can develop intraventricular pressures up to 300 mmHg. Coronary perfusion to the LV occurs mainly in diastole, when the myocardium is relaxed. The right ventricle receives blood from the venae cavae and coronary circulation, and pumps it via the pulmonary vasculature into the LV. Since PVR is a fraction of SVR, pulmonary arterial pressures are relatively low and the wall thickness of the right ventricle (RV) is much less than that of the LV. The RV thus resembles a passive conduit rather than a pump. Coronary perfusion to the RV occurs continuously during systole and diastole because of the low intraventricular and intramural pressures. In spite of the anatomical differences, the mechanical behaviour of the RV and LV is very similar. -

Functions of the Heart • Generaqon of Blood Pressure • Rouqng of Blood
Functions of the Heart • Generaon of blood pressure • Rou'ng of blood • Ensuring unidirecon flow of blood • Regula'on of blood supply 1 2 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduc'on or display. CO2 O2 Pulmonary circuit O2-poor, CO2-rich O2-rich, blood CO2-poor blood Systemic circuit CO2 O2 3 4 5 6 7 8 9 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduc'on or display. Le AV (bicuspid) valve Right AV (tricuspid) valve Fibrous skeleton Openings to coronary arteries AorCc valve Pulmonary valve (a) 10 11 12 13 14 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduc'on or display. 10 1 Blood enters right atrium from superior and inferior venae cavae. 2 Blood in right atrium flows through right Aorta Le pulmonary AV valve into right ventricle. 11 artery 3 Contracon of right ventricle forces 5 5 pulmonary valve open. 4 Blood flows through pulmonary valve 9 Pulmonary trunk Superior into pulmonary trunk. vena cava 4 Le pulmonary 6 5 Blood is distributed by right and le veins pulmonary arteries to the lungs, where it Right 6 unloads CO and loads O . pulmonary 2 2 Le atrium veins 1 AorCc valve 6 Blood returns from lungs via pulmonary veins to leE atrium. 3 7 Le AV 7 Blood in le atrium flows through le AV Right (bicuspid) valve 8 valve into leE ventricle. atrium Le ventricle 2 8 Contracon of leE ventricle (simultaneous with Right AV step 3 ) forces aorCc valve open. (tricuspid) valve 9 Blood flows through aorCc valve into Right ascending aorta.