Access and Usage of Long Lasting Insecticidal Nets (LLIN) in Rural Communities of Benue State, Nigeria Justice Adaji and Obi Ekpeme Gabriel*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IOM Nigeria DTM Flash Report NCNW 37 (31 January 2021)
FLASH REPORT #37: POPULATION DISPLACEMENT DTM North West/North Central Nigeria Nigeria 25 - 31 JANUARY 2021 Casualties: Movement Trigger: 160 Individuals 9 Individuals Armed attacks OVERVIEW The crisis in Nigeria’s North Central and North West zones, which involves long-standing tensions between NIGER REPUBLIC ethnic and religious groups; attacks by criminal Kaita Mashi Mai'adua Jibia groups; and banditry/hirabah (such as kidnapping and Katsina Daura Zango Dutsi Faskari Batagarawa Mani Rimi Safana grand larceny along major highways) led to a fresh Batsari Baure Bindawa wave of population displacement. 134 Kurfi Charanchi Ingawa Sandamu Kusada Dutsin-Ma Kankia Following these events, a rapid assessment was Katsina Matazu conducted by DTM (Displacement Tracking Matrix) Dan Musa Jigawa Musawa field staff between 25 and 31 January 2021, with the Kankara purpose of informing the humanitarian community Malumfashi Katsina Kano Faskari Kafur and government partners in enabling targeted Bakori response. Flash reports utilise direct observation and Funtua Dandume Danja a broad network of key informants to gather represen- Sabuwa tative data and collect information on the number, profile and immediate needs of affected populations. NIGERIA Latest attacks affected 160 individuals, including 14 injuries and 9 fatalities, in Makurdi LGA of Benue State and Faskari LGA of Katsina State. The attacks caused Kaduna people to flee to neighbouring localities. SEX (FIG. 1) Plateau Federal Capital Territory 39% Nasarawa X Affected Population 61% Male Makurdi International border Female 26 State Guma Agatu Benue Makurdi LGA Apa Gwer West Tarka Oturkpo Gwer East Affected LGAs Gboko Ohimini Konshisha Ushongo The map is for illustration purposes only. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

REQUEST for PROPOSAL Living Income Benchmarking
REQUEST FOR PROPOSAL Living Income Benchmarking (LIB) Study in Nigeria 1 1.0 General Information This document is being issued in order to solicit applications from potential [firms or consultants] to conduct a living income benchmarking study. The activity entails collecting data in four states in Nigeria, precisely in Ogun State (Odeda Local Government Area - LGA, Ijebu-Ode LGA, Ewekoro LGA, and Odogbolu LGA), Edo State (Ikpoba Okha LGA, Oredo LGA, Egor LGA), Benue State (Agatu LGA, Guma LGA, Gwer-East LGA, Gwer-West LGA, Logo LGA, Okpokwu LGA, Ogbadigbo LGA, and Kwande LGA), and Nasarawa State (Awe LGA, Doma LGA, Lafia LGA, Obi LGA). It will require at least 19 qualitative interviews (19 Focus Group Discussions and 57 Key Informant Interviews), 19 market surveys and an extensive secondary data review. Ultimately, HI anticipates the consultant to consolidate the LIBs based on cost similarities in the States, LGAs or location (Rural/Urban). The terms of reference contain background information, the desired methodology, including objectives, the timeframe, and a list of deliverables. This document also contains information about the kind of expertise that Heifer seeks for this activity and guidance on how to submit a proposal to conduct the activity. Heifer anticipates awarding a fixed award for the study and make payments based on submission and Heifer’s approval of deliverables. The award agreement will include a payment schedule with specific deliverables; all payments require 10 business days processing after approval of deliverables. 1.1 Background of Heifer International Heifer Project International (HPI) is a global non-profit working to end hunger and poverty and care for the Earth by using sustainable practices and engaging smallholder farmers in agricultural development. -

The October 13, 2010 Landslides on the Azenge Mountain in Imande Ukusu, Nkomon Disrict, Benue State, Nigeria
Environment and Ecology Research 2(3): 113-121, 2014 http://www.hrpub.org DOI: 10.13189/eer.2014.020301 The October 13, 2010 Landslides on the Azenge Mountain in Imande Ukusu, Nkomon Disrict, Benue State, Nigeria Ako Thomas Agbor*, Abba Francis Mohammed, Onoduku usman Shehu, Nuhu Waziri Musa, Alabi Adekola A., Mamodu Adegbe Department of Geology, School of Natural and Applied Sciences, Federal University of Technology, Minna, Nigeria *Correspondent author: [email protected] Copyright © 2014 Horizon Research Publishing All rights reserved. Abstract A swarm of 14 landslides occurred Landslides are geological phenomenon which occurs as a spontaneously within the Azenge Mountain on November result of ground movement, rock falls, and failure of unstable 13th, 2010 between the hours of 1 and 6 am after torrential slopes; sand and debris flow on slope and can cause a lot of rains. The landslides were studied using interviews, field damages with direct and indirect effect on human settlements observations and laboratory study of the soil samples and physical infrastructure [1]. According to [ 2 ] landslide collected from the major landslide site. Results of the study describes a wide variety of processes that result in the show that the event that was reported by many local media in downward and outward movement of slope forming Nigeria as volcanic eruption was a spontaneous massive materials including rocks, soil, artificial fills or a slope movement along the mountainous terrain of Imande combination of them. Landslides are common in areas where Ukusu, Mon village. About 1,123,918 m3 of rock and debris slope stability has been compromised. -

X-Raying the Impact of Grazers/Cultivators’ Conflict on the Management of Secondary Schools in Benue State
X-RAYING THE IMPACT OF GRAZERS/CULTIVATORS’ CONFLICT ON THE MANAGEMENT OF SECONDARY SCHOOLS IN BENUE STATE Prof. Adejo Okwori Department of Educational Foundations, Benue State University, Makurdi Gbough, Samuel Aondowase Department of Educational Foundations, Benue State University, Makurdi Abstract This study investigated impact of grazers/cultivators’ conflict on the management of secondary schools in Benue state, Nigeria. Two research questions and two hypotheses guided the study. Descriptive survey research design was adopted for the study. The population of the study comprised 5110 teachers in 297 grant-aided secondary schools in Benue State. A sample of 511 teachers was used for the study. The selection was done using a simple random sampling technique. A 10-item structured four-point rating scale questionnaire titled “Grazers/Cultivators Conflict Questionnaire (GCCQ)” was used for data collection. The instrument was validated by two experts, one in Educational Management from Benue State University, Makurdi and a second expert in Measurement and Evaluation from Federal University of Agriculture, Makurdi. The reliability of the instrument yielded a coefficient of 0.82 which indicated that the instrument was reliable for usage. Descriptive statistics of mean and standard deviation were used to answer the research questions. The hypotheses were tested using chi-square (χ2) test of goodness of fit at 0.05 level of significance. The findings indicated that grazers/cultivators conflict has significant impact on school facilities and the lives of teachers and students in secondary schools in Benue State, Nigeria. It was recommended among others that Government at all levels should find a way of encouraging mass education among the grazers and cultivators. -

“Blackfly” in Ikov Ward of Ushongo Local Government Area of Benue State of Nigeria
International Journal of Education and Research Vol. 6 No. 5 May 2018 Environmental Conditions favouring Growth of “Blackfly” in Ikov Ward of Ushongo Local Government Area of Benue State of Nigeria. Upa, Callistus Terungwa Department of Geography, College of Education, Katsina-Ala, P.M.B 2008, Katsina –Ala Local Government Area, Benue State of Nigeria. [email protected], 08139745190 Abstract-The purpose of the study is to examine the environmental conditions favouring the growth of “black fly” resulting to the disease Onchocerciasis in Ikov ward of Ushongo Local Government Area of Benue State, Nigeria. Data was collected on the disease, Environmental Conditions Favouring the Growth of Blackfly, Blackfly species, Physicochemical Parameters and Density of Simuliids in rivers in the study area. The results of the study showed that both physicochemical and ecological parameters constitute the major environmental conditions in the area and they influenced the density of simuliids. For methodology, Aquatic stages of simulium were sampled covering 5 kindred areas of study area. Water samples were collected from the 5 rivers and analysed. Questionnaires were distributed in the 5 kindred areas to acquire relevant information about the breading sites. The study concluded that the dominance of Simulium damnosum complex, in the study area presents potential risk for the area. Keywords – Amire - Ukiriki river basin, Blackfly, Disease, Environmental Conditions, Onchocerciasis. 1. INTRODUCTION Onchocerciasis ranks as one of the most formidable infectious disease of the world, occurring mostly in savannah and rain forest area of Africa. It is also known as “river blindness” the parasitic disease is caused by filarial worm oncherca volvulus and transmitted by blood sucking blackflies of genus simulium which breed in rapidly flowing rivers. -

Arts, Peace and Conflict
Working Paper Series n˚4: Arts, Peace and Conflict Theatre for Development and the Management of Land Conflicts Amongst the Tiv of Central Nigeria by DOKI, Ama Gowon, PhD & Aondowase BOH, PhD Theatre Arts Department, Benue State University, Makurdi-Nigeria. Email: [email protected] A paper presented at July 2014 Conference "Arts, Peace and Conflict" at the Archbishop Desmond Tutu Centre for War and Peace Studies, Liverpool Hope University, UK 1 Abstract This paper examines the efficacy of Theatre for Development (TfD) as an alternative conflict management strategy that is people centred. The paper focuses on the potentials of theatre to manage land conflicts that have bedevilled Tiv land over the years. Data for the paper is randomly collected among conflict stakeholders in Tiv land. The survey design is used in order to elicit information on the conflict management strategies that have been deployed in the study area. Semi structured interviews and focused group discussion tools are used to collate information on conflict and conflict management strategies. The paper finds out that, land conflicts have persisted in Tiv land because of the top-down approaches that have been used in managing such conflicts. The top-down approaches do not get the support of conflict stakeholders as they feel alienated from them. The paper submits that, theatre for development can build the needed peace by giving voice to the voiceless in managing their differences for peace and development. Through a pilot study conducted in and around Mbatser district to test the efficacy of theatre in conflict management, the paper concludes that the development of a people centred approach in conflict management is essential to ensure that early warning signs are captured and acted upon to prevent crisis – hence prevention is better than cure. -

Aquifer Characteristics of Some Local Government Areas of Benue State, Nigeria
Nigerian Journal of Technology (NIJOTECH) Vol. 38, No. 1, January 2019, pp. 233 – 241 Copyright© Faculty of Engineering, University of Nigeria, Nsukka, Print ISSN: 0331-8443, Electronic ISSN: 2467-8821 www.nijotech.com http://dx.doi.org/10.4314/njt.v38i1.28 AQUIFER CHARACTERISTICS OF SOME LOCAL GOVERNMENT AREAS OF BENUE STATE, NIGERIA G. D. Akpen1,*, M. I. Aho2 and M. G. Adejo3 1, 2, 3, DEPARTMENT OF CIVIL ENGINEERING, UNIVERSITY OF AGRICULTURE, MAKURDI, BENUE STATE, NIGERIA E-mail addresses: [email protected], [email protected], [email protected] ABSTRACT Well pumping test results from 74 boreholes within twelve LGAs of Benue State were collated and analysed to determine the aquifer hydraulic characteristics. Cooper-Jacob’s non-uniform flow equation was used to determine the transmissivity, T, storativity, S, hydraulic conductivity, K and specific capacity, Sc of the aquifers of the study areas. The Geographical Information System (GIS) was used to generate colour coded maps of the determined hydraulics characteristics of the aquifers. The static water level (SWL) ranged from 2 to 8 m in Katsina-Ala, Ado, parts of Vandeikya and Gboko, while the rest of the study areas had SWL of 8 to 20 m with isolated areas of Konshisha and Gboko having SWL up to 38 m. Hydraulic conductivity values fall between 0.01 to 1.0 m/day in most of the study areas except Gboko and Buruku LGAs where K ranged between 1.0 to 5.0 m/day. The specific capacity of major parts of the study areas ranged from 0.01 to 10 m2/day except Konshisha, Gboko and Ushongo LGAs where the values ranged from 10.0 to 50.0 m2/day with the highest value of 83 m2/day obtained at Tse-Filla in Konshisha LGA. -
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Eurasian Journal of Agricultural Research RURAL FARMERS
Eurasian Journal of agricultural research RURAL FARMERS’ PERCEPTION OF COMMUNAL CONFLICTS IN BENUE STATE, NIGERIA ‡Kughur, P.G., †Dukut, J. and 1Katikpo, G. ‡Department of Agricultural Extension and Communication, University of Agriculture, P.M.B. 2373 Makurdi, Benue State, Nigeria. †Provostry (Farm Unit), Plateau State College of Agriculture, Garkuwa, Plateau State, Nigeria 1Department of Agricultural Education, College of Education Akwanga P.M.B. 05 Akwanga, Nassarawa State, Nigeria ‡Corresponding author and e-mail: [email protected] Abstract The study assessed rural farmers’ perception of communal conflict in Benue State. Multi- stage random sampling was adopted in selecting four Local Government Areas. In each of the local government areas selected, three villages were purposively selected based on occurrence of communal conflicts in the area. Simple random sampling was used in administering structured questionnaire through interview to the 120 respondents. Data collected were analyzed through descriptive statistics and graph. Results of the findings revealed that 57.50% of communal conflicts were caused by land disputes, 38% communal conflicts reduced development, 65% communal conflicts caused social vices and promoted negative cohesion, 62% communal conflicts reduced volume of trade, 22.09% leaders and political appointees of communities involved in communal conflicts should be removed and 12.0% land communities are fighting over it should be taken over by government. It is recommended that proper boundary demarcation should be carried out in all places to avoid communal conflicts. Keywords: Rural, farmers, perception, communal, conflicts, Benue State INTRODUCTION Conflict is that form of social interaction in which the actors seek to obtain scare reward by eliminating or weakening other contenders. -

Independent National Electoral Commission (INEC)
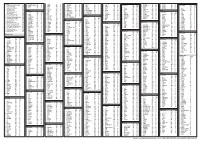
FEDERAL REPUBLIC OF NIGERIA Independent National Electoral Commission (INEC) BENUE STATE DIRECTORY OF POLLING UNITS Revised January 2015 DISCLAIMER The contents of this Directory should not be referred to as a legal or administrative document for the purpose of administrative boundary or political claims. Any error of omission or inclusion found should be brought to the attention of the Independent National Electoral Commission. INEC Nigeria Directory of Polling Units Revised January 2015 Page i Table of Contents Pages Disclaimer.............................................................................. i Table of Contents ……………………………………………… ii Foreword................................................................................ iv Acknowledgement.................................................................. v Summary of Polling Units....................................................... 1 LOCAL GOVERNMENT AREAS Ado............................................................................... 2-7 Agatu............................................................................ 8-12 Apa............................................................................... 13-17 Buruku.......................................................................... 18-25 Gboko........................................................................... 26-39 Guma............................................................................ 40-48 Gwer East..................................................................... 49-55 Gwer West................................................................... -

Co-Endemicity, Poly-Parasitism and Poverty:Need for Baseline Research and Evidence Based Intervention
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 21, Issue 1, Ver. V (Jan. 2016) PP 07-17 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Co-Endemicity, Poly-Parasitism and Poverty:Need For Baseline Research and Evidence Based Intervention. Aju-Ameh, Celina Onyawoibi. 1Faculty of Natural Sciences, Department of zoology. University of Jos, Plateau State, Nigeria. Abstract: The unseen complexity behind the emerging trend of co-endemicity and poly parasitism along with the incapacitating forces of poverty is ably set to hinder the people of Benue state from attaining their full potential.This article though not an exhaustive list seeks to explore some of the challenges needing urgent and aggressive attention. The limitations of the available data(fabricated and captured), the dearth of information and the challenging effort made at gathering evidence of better quality is clearly expressed. There is no significant difference in the living conditions of the urban poor and rural poor who are the majority. Common to both groups are lack of access to quality education, housing, clean water and health care. The three pandemic diseases Aids/HIV, Tuberculosis, Malaria [ATM] and five of the neglected tropical diseases are all endemic in this state and in some places co-exist, an assault that needs evidence based intervention. As unfathomable as the realities on ground are, I have gone through the maze to provide a panoramic view of some of these diseases, in some cases the risk factors and the extent to which obstacles hinder effective control and management of these diseases in the food basket of the nation- Benue state, Nigeria.