William B. Schwartz Division of Nephrology 2020 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
I I I Vswit • I Of. All In. Imvt-Nlim:Klranli-L«Imt Itulun Hutmoovaruiuhiit Fnotl Ketort. > Royai.Bakinn F>Nwnicncn.,Ti
vSwit m •i iii ii m Mta. ' LcwIh Banden la on the alok Hal — Mr. aud: Mn.'Chaa. Brunk of Lealle :'IIni.'a«<t. Joiiaa iHOii tbe:Kalii.—Mta. vlaltud at A. Dubuta' Friday.—D«- Bobert DIH and. lira: Nathen Boae of Witt OuHola^whu' Hiaa beeu taaublng :RIvtw TutNulay.—Harrle Fox waa: lir aolionl near Parma; la homo again.— ;Batou Ranlda nn hnHlneiw laHt week. Ma«Kle Barr, who'liaa Juat returned J. N. SMITH —LuriiarJ Oawitt vli>lted hia awn In from Dakota, and Beitlia Rumory are Mills Dry fioods Company. 'jMkauii Friday.—Jamea Oardiier and vlaitlUKlii tbia vIoliilty.-Tbe anoial Wishes to call your atten- wife or nMi> Bunkerlilll vlalted M. al Jaa.llarr'a waa a aueoeaa, 810.90 be Ji Bowdlab Friday.-JaniM Naah re* ing ralaed wblcli will be uaed to get a this week to his SPECIAL Mutty hurt btahiind at Pottcr'a mill globe fur tbe aebuol. SALE of iotliatlie lalald III* fora few dava.-^ Tb« party Blveu by Irvln Hadly at VOL. XXXV.-NO. 3. Fllehbarg. MASON, MICH.. THURSDAY, JANUARY 19. 1893. WHOLE NO. 1776. Nortb I>a1lt Hotel Friday evening waa well attended. There will be an* Cliaa. Pnxann and wife are visiting WHAT IS QOINQ ON PANTS otber one there Friday aveuing, Jan. at II. R. Puxaun'a.—Meinhera nf the grange are preiiarlng a play for tbe IS. All aiecoKllallyliiviied. Supper THIS WEEK AT M. D. Q. O'S. Lard wanted at the bakery In the Warm ineala SO cents. At near future.—Tlianka totlie NBWBfor Sixty pair of $6.50 Pants roatau VUI'I* ABD VMITttBS- will beeerved at U. -

Ontario County Marriage Records 1908-1935 (Files)
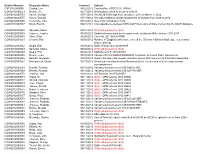
Ontario County Marriage Records 1908-1935 (Files) License Groom Last Name Groom First Name Bride Last Name Bride First Name Year Number Bin ABBEY W. CHANCEY MARKS ABIGAIL A. 1909 545 AM24-019 ABBOTT MICHAEL MOSES CATHERINE 1909 347 AM24-006 ABBOTT SAMUEL JACOB SALOOM 1913 2254 AM24-032 ABBOTT STANLEY FREI EVELYN 1929 1146 AM24-073 ABEL CARL J. FREI ALBERTINA 1909 578 AM24-019 ABEL PERRY H. BAKER ETHEL M. 1912 1654 AM24-017 ABERCROMBE VAUGH F. WOODCOCK ROBY 1927 398 AM24-059 ABESHENE ARTHUR WALTERS VINA 1932 2036 AM24-088 ABRAHAM JOHN BROWN MARY 1908 52 AM24-005 ABRAHAM ALBERT A. BARRY ELIZABETH 1912 1900 AM24-018 ABRAMSKY MORRIS GRUSKIN SYLVIA 1932 4031 AM24-102 ACE ELMER GETMAN CAROL 1934 5701 AM24-130 ACHESON RALPH H. STERLING MARIE E. 1911 1306 AM24-004 ACQUILANO DOMINIC TAYLOR HELEN 1934 5596 AM24-130 ADAM GEORGE S. BLEYER JOSEPHINE A. 1909 375 AM24-006 ADAM JOHN TOWERS CARRIE 1927 543 AM24-059 ADAMS FRED PENNER NINA 1908 98 AM24-005 ADAMS FRED M. DONNELLY ETHEL M. 1912 1629 AM24-017 ADAMS MILLER BAUM ELIZABETH 1912 1687 AM24-017 ADAMS ARTHUR L. BURNETT BERTHA B. 1914 2352 AM24-032 ADAMS LESTER G. LEWIS BERTHA M. 1926 162 AM24-045 ADAMS FLOYD MARSH HELEN 1931 1820 AM24-088 ADAMS HAROLD ARGETSINGER LUCILE 1932 1992 AM24-088 ADAMS THOMAS GAUDET EMMA 1934 5597 AM24-130 ADAMSON WILLIAM GOODMAN CARRIE 1928 646 AM24-060 ADAMSON FREDERICK MELIOUS AGNES 1930 1363 AM24-074 ADSITT ARNOLD SMITH MARY 1929 1011 AM24-073 ADSITT FLOYD KEAR DOROTHY 1934 5477 AM24-116 AEBERSOLD ELMER J. -

OIPA in India
OIPA in India Recipient: HE President of India, New Delhi, HE Vice President of India, New Delhi., Hon'ble Prime Minister of India, The Secretary, Ministry of Environment and Forest, Director, AWD, The Ministry of Home Affairs, Hon'ble Ch. Bhupinder Hooda, Chief Minister of Haryana, The Chairman, State Committee for Slaughter Houses, Haryana, Hon'ble Minister of Home Affairs, Hon'ble Chief Secretary to Govt. of Haryana, The Cabinet Secretary to Govt. of India, Ho'ble Smt. Jayanthi Natrajan, The Wildlife Crime Control Bureau, Hon'ble Speaker, Haryana Assembly, HE Governor of Haryana, Shri Deepender Hooda, MP, Shri Rahul Gandhi, Vice President, AICC, The Member Secretary, State Committee for Slaughter Houses, Shri B.K. Hariprasad, General Secretary, AICC, and OIPA in India Letter: Greetings, Naresh Kadyan: Man of Many distinctions Greetings, Where as Gandhian Ideologist, philosopher, environmentalist and social reformer Naresh Kadyan, founder Chairman of the People for Animals (PFA) Haryana – www.pfaharyana.in , representing Italy based, United Nations affiliated the International Organisation for Animal Protection - OIPA in India – www.oipa.org needs recognition in the field of RTI, Disaster Management, animal rights and their welfare read with Wildlife conservation category. Naresh Kadyan, C-38, Rose Apartment, sector-14, Prashant Vihar, Rohini, Delhi - 110085 was born on 10th October, 1961 in village Siwana, now in Jhajjar District of Haryana, he is a Master Trainer of the Animal Welfare Board of India, had been Nodal Inspecting Authority for Haryana and adjoining areas of Rajasthan of the Animal Welfare Division (Govt. of India), Nominee of the CPCSEA, Masters in Journalism and Mass Communication along with Post Graduate Diploma in J&MC, Diploma in Footwear Technology along with Advance course with ‘Distinction’ as well, elected as Member of the Clothing and Footwear Institute, London on November 8th, 1988. -

Balloon Assisted Technique in Peripheral Interventions: a Use- Ful Tool
Pozzi Mucelli F, et al., J Angiol Vasc Surg 2019, 4: 022 DOI: 10.24966/AVS-7397/100022 HSOA Journal of Angiology & Vascular Surgery Case Report technique is rarely reported [2-5]. We describe some original applica- Balloon Assisted Technique in tions of BAT of our experience. Peripheral Interventions: A Cases Description Giant aneurysm of pancreatic-duodenal artery. Female, 65 yrs Useful Tool Abdominal CT exam identified a 5 cm aneurysm of pancreatic-du- Pozzi Mucelli Fabio, Pozzi Mucelli Roberta Antea* , Sacconi odenal artery probably due to occlusion of the origin of the celiac Francesca, Braini Massimiliano, Belgrano Manuel Gianvalerio trunk caused by Dunbar Syndrome. Follow-up CT demonstrated a and Cova Maria Assunta mild enlargement of the aneurysm and for this reason an endovascular Department of Radiology, Azienda Sanitaria Universitaria Integrata di treatment was proposed. Coiling of the aneurysm was rejected due to Trieste, Trieste, Italy the risk of occlusion of the parent artery feeding the gastroduodenal, hepatic and splenic artery and we considered to exclude the aneurysm with a flow-diverter stent. Procedure was done in local anesthesia Abstract using brachial approach. After Superior Mesenteric Artery (SMA) catheterization a 6F guiding catheter (Envoy Cardinal Health) was Balloon Assisted Technique (BAT) consists in the use of a balloon advanced at the origin of the pancreatic-duodenal artery, close to the catheter advanced in a parallel fashion to main catheter in the same aneurysm (Figure 1a). A .014 guidewire (V14 Boston) was advanced artery to overcome problems during endovascular interventions. We describe three different cases of BAT. The first case is an example distally to the aneurysm, but with a large “loop” inside it (Figure 1b). -

Annual Report Mission Statement Report from the President and Chair
2009 Annual Report mission statement report from the president and chair American Near East Refugee Aid (ANER A) advances the well-being of people in the West Bank, Gaza, Lebanon and Jordan. Through partnerships and close consultation with local groups and communities, ANERA responds to economic, health and educational needs with sustainable solutions and also delivers humanitarian aid during emergencies. Committed. Since 1968, ANERA — a U.S.-based, nonprofit organization — has been expanding programs throughout Gaza, the West Bank, and Lebanon to reach more Palestinian families in need. Our education, health, and job creation programs help many thousands of people every year. Ready. ANERA is ready to respond to changing conditions on the ground with flexibility and resiliency. We work with over 200 local partners and have a staff of engineers, medical professionals, I.T. specialists, educators and international development experts. Respected. We earn respect with the results we deliver. ANERA’s Board includes retired diplomats, international business executives, noted scholars, and citizen activists. All have chosen to join ANERA because of our mission and our ability to efficiently deliver programs and relief. Trusted. From a Lebanese businesswoman in London to the U.S. Agency for International Development, thousands of donors from around the world trust us because they know their money is safe and spent on their intended purpose: to help people in need. A farmer near Qalqilia, in the West Bank, shows off some of his new crop of tomatoes, grown in a greenhouse ANERA constructed on his land. LizDemarest report from the president and chair Although we could say this every year, Fiscal Year 2009 tested ANERA’s resiliency. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

Font Selection
JJ IIIIII SSSSSS 0000 3333 555555 888 AAAA JJ IIIIII SS SS 0 00 3 3 5 8 8 AAAAAA JJ II SSS 0 0 0 33 55555 888 AA AA JJ JJ II SSS 0 0 0 3 5 8 8 AAAAAA JJJJJJ IIIIII SS SS 00 0 3 3 5 8 8 AAAAAA JJJJ IIIIII SSSSSS 0000 3333 55555 888 AA AA JJ 0000 0000 0000 9999 2222 3333 3333 JJ 0 00 0 00 0 00 9 9 22 22 3 3 3 3 JJ 0 0 0 0 0 0 0 0 0 9 99 22 33 33 JJ JJ 0 0 0 0 0 0 0 0 0 999 9 222 3 3 JJJJJJ 00 0 00 0 00 0 9 22 3 3 3 3 JJJJ 0000 0000 0000 9 222222 3333 3333 * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * * START RMTSCPA SC7054 REPORT ROOM C11A 10.25.22 AM 28 SEP 2020 * *2 J0009233 JIS0358A TPSCPA H111 ACCTNG PR17 JIS0358A J0009233 2* BMIRRPT CITY & COUNTY OF SAN FRANCISCO COURT MANAGEMENT SYSTEM REPORT # 7054 RUN 09/28/20 @ 10:25 PAGE 1 *------------------------------------------------------------------------------- (CC7054. -

Phonographic Performance Company of Australia Limited Control of Music on Hold and Public Performance Rights Schedule 2
PHONOGRAPHIC PERFORMANCE COMPANY OF AUSTRALIA LIMITED CONTROL OF MUSIC ON HOLD AND PUBLIC PERFORMANCE RIGHTS SCHEDULE 2 001 (SoundExchange) (SME US Latin) Make Money Records (The 10049735 Canada Inc. (The Orchard) 100% (BMG Rights Management (Australia) Orchard) 10049735 Canada Inc. (The Orchard) (SME US Latin) Music VIP Entertainment Inc. Pty Ltd) 10065544 Canada Inc. (The Orchard) 441 (SoundExchange) 2. (The Orchard) (SME US Latin) NRE Inc. (The Orchard) 100m Records (PPL) 777 (PPL) (SME US Latin) Ozner Entertainment Inc (The 100M Records (PPL) 786 (PPL) Orchard) 100mg Music (PPL) 1991 (Defensive Music Ltd) (SME US Latin) Regio Mex Music LLC (The 101 Production Music (101 Music Pty Ltd) 1991 (Lime Blue Music Limited) Orchard) 101 Records (PPL) !Handzup! Network (The Orchard) (SME US Latin) RVMK Records LLC (The Orchard) 104 Records (PPL) !K7 Records (!K7 Music GmbH) (SME US Latin) Up To Date Entertainment (The 10410Records (PPL) !K7 Records (PPL) Orchard) 106 Records (PPL) "12"" Monkeys" (Rights' Up SPRL) (SME US Latin) Vicktory Music Group (The 107 Records (PPL) $Profit Dolla$ Records,LLC. (PPL) Orchard) (SME US Latin) VP Records - New Masters 107 Records (SoundExchange) $treet Monopoly (SoundExchange) (The Orchard) 108 Pics llc. (SoundExchange) (Angel) 2 Publishing Company LCC (SME US Latin) VP Records Corp. (The 1080 Collective (1080 Collective) (SoundExchange) Orchard) (APC) (Apparel Music Classics) (PPL) (SZR) Music (The Orchard) 10am Records (PPL) (APD) (Apparel Music Digital) (PPL) (SZR) Music (PPL) 10Birds (SoundExchange) (APF) (Apparel Music Flash) (PPL) (The) Vinyl Stone (SoundExchange) 10E Records (PPL) (APL) (Apparel Music Ltd) (PPL) **** artistes (PPL) 10Man Productions (PPL) (ASCI) (SoundExchange) *Cutz (SoundExchange) 10T Records (SoundExchange) (Essential) Blay Vision (The Orchard) .DotBleep (SoundExchange) 10th Legion Records (The Orchard) (EV3) Evolution 3 Ent. -

Russian Society of Angiologists and Vascular Surgeons Invites You to Take Part in the XXXVI International Conference on June 18-20, 2020 in Korston Hotel in Kazan
Dear colleagues! Organizing Committee of the Russian Society of Angiologists and Vascular Surgeons invites you to take part in the XXXVI International Conference on June 18-20, 2020 in Korston Hotel in Kazan. The conference will cover all developments in angiology, vascular and endovascular surgery, as well as phlebology. Our conference encompasses a wide range of topics, as usual. The program will include round tables, video broadcasting, interactive educational programs, trainings and workshops on various branches of vascular surgery. Objectives of the conference: • getting to know world trends in vascular surgery, • finding more about new technologies, including endovascular ones, • introducing new methods for diagnostics of vascular diseases, • exploring long-term results of open and endovascular interventions, • exploring potential complications and errors of various surgical techniques, • evaluating short-term and long-term results of reconstructions, and • wide exchange of experience in vascular procedures. Conference provider: Russian society of angiologists and vascular surgeons Conference agenda: I. Surgical treatment for brachiocephalic arteries: • emergency and scheduled carotid procedures in patients with cerebrovascular accidents and transient ischemic attacks, vertebrobasilar insufficiency of various nature, and approach to concomitant interventions. II. Surgery of aorta: surgical treatment for aneurysms and dissections of thoracic aorta (emergency and scheduled interventions), • emergency and scheduled treatment for abdominal aorta aneurysms, • inflammatory diseases of aorta and aortic branches, • aortic dysplasia and new approaches to treatment, • hybrid aortic repair. III. Long-term results and comparison of surgical methods for various locations. IV. Surgical treatment for aorto-ileac area and visceral aortic branches. Selecting the treatment option. V. Surgical treatment for lower limb arteries. VI. -
Control Number Requester Name Scanned Subject CNT2012000005 Guidos, Lori 06/22/2012 Contract No
Control Number Requester Name Scanned Subject CNT2012000005 Guidos, Lori 06/22/2012 Contract No. HSSCCG11J00088 COW2012000553 Melton, K.E. 05/31/2012 Information related to Vacancy 624276 COW2012000554 Vance, Donald 05/31/2012 All USCIS FOIA logs from January 1, 2011 to March 1, 2012 COW2012000555 Vance, Donald 05/31/2012 Records relating to all USCIS payment to Verizon from 2009 to 2010 COW2012000556 Ciccarone, Lilin 05/16/2012 New York Immigration Fund COW2012000557 Mock, Brentin 06/01/2012 Correspondence between DHS and Fl Secretary of State concerning the SAVE database COW2012000558 Zamudio, Maria 06/01/2012 Withheld pursuant to (b)(6) COW2012000559 Holmes, Jennifer 06/05/2012 Statistical Information on decsions made by Asylum Officers from 1991-2011 COW2012000560 Viker, Elliot 06/05/2012 Case No. 201106424 PRMI COW2012000561 Choucri, Mai 06/06/2012 Number of Egyptians who have entered the US from 1990 to include age, sex, marital status, and city COW2012000562 Siegal, Erin 06/06/2012 DOS referral Case 201001905 COW2012000563 Zamudio, Maria 06/06/2012 Withheld pursuant to (b)(6) COW2012000564 Siegal, Erin 06/06/2012 DOS Referral F-2010-00014 COW2012000565 Newell, Jean 06/07/2012 Vacancy ID CIS-596922-FDNS/NSC to include Selection Panel Documents COW2012000566 Estrella, Alejandro 06/07/2012 Inquiry into how many people and their names that requester is financially supporting COW2012000567 Montgomery, David 06/10/2012 All documents submitted by Manassas Ballet Theater and related congressional correspondence COW2012000568 Debrito, Ricardo -
APUS Commencement Program 2020
COMMENCEMENT 2020 CONGRATULATIONSto the Class of 2020! You have successfully completed the requirements of your respective degree programs and now join the ranks of over 93,000 other American Military University (AMU) and American Public University (APU) alumni. You should be very proud of this accomplishment! This year’s graduating class comprises more than 11,000 graduates. The paths that each of you took to reach this accomplishment are quite diferent. Many of you studied while serving our country, domestically and abroad. Some of you studied between shifs at your local fre and rescue departments. Others studied while at home, raising your families and/or working full-time. Regardless of the route you took, you persevered; you earned your degree. At American Public University System (APUS), we appreciate your trust in us to provide you with a quality education relevant to your careers and lives afer graduation. With feedback from each of you during your time spent as students, we have been able to continuously improve our courses, programs, processes, and practices. From our beginnings nearly 30 years ago when we ofered a single master’s degree to today where we ofer more than 200 associate, bachelor’s, master’s, and doctoral degrees, our decisions resulted from listening to you, our students and alumni. We understand the challenges of balancing work, family, and college and are aware of the sacrifces made in order to reach your academic goal. Cherish this moment and celebrate this occasion with your family, friends, and classmates. Recognize your achievement for the major milestone this accomplishment represents. -

November 5, 2020 at 12:00 P.M
NOTICE OF PONTIAC CITY COUNCIL MEETING November 5, 2020 at 12:00 p.m. THE MEETING WILL BE HELD ELECTRONICALLY The City Council of the City of Pontiac will hold a Study Session on November 5, 2020 at 12:00 p.m. This meeting will be held electronically as allowed by the amended Open Meetings Act. The agenda of the Study Session is attached. The Pontiac City Council gives notice of the following: 1. Procedures. The public may view the meeting electronically through the following method. http://pon tiac.mi. us/coun cil/pontiactv /index. php 2. Public Comment. For individuals who desire to make a public comment, please submit your name and comment in writing to [email protected]. Additionally, you may submit your public comment in writing directly to the Office of the City Clerk during regular business hours. All public comments must be received no later than 11 :30 a.m. on November 5, 2020. Public comments are limited to three (3) minutes. The City Clerk will read your comments during the public comment section of the meeting. 3. Persons with Disabilities. Persons with disabilities may participate in the meeting through the methods set forth in paragraph 2. Individuals with disabilities requiring auxiliary aids or services in order to attend electronically should notify the Interim City Clerk, Garland Doyle at (248) 758-3200 or [email protected] at least 24 hours in advance of the meeting. Dated 10-31-2020, 5:00 p.m. Garland S. Doyle, Interim City Clerk City of Pontiac 47450 Woodward Ave.