Lumbosacral Plexus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ischaemic Lumbosacral Plexopathy in Acute Vascular Compromise:Case Report
Parapkgia 29 (1991) 70-75 © 1991 International Medical Soci<ty of Paraplegia Paraplegia L-_________________________________________________ � Ischaemic Lumbosacral Plexopathy in Acute Vascular Compromise: Case Report D.X. Cifu, MD, K.D. Irani, MD Department of Physical Medicine, Baylor College of Medicine, Houston, Texas, USA. Summary Anterior spinal artery syndrome (ASAS) is a well reported cause of spinal cord injury (SCI) following thoracoabdominal aortic surgery. The resultant deficits are often incom plete, typically attributed to the variable nature of the vascular distribution. Our Physi cal Medicine and Rehabilitation (PM and Rehabilitation) service was consulted about a 36-year-old patient with generalised deconditioning, 3 months after a stab wound to the left ventricle. Physical examination revealed marked lower extremity weakness, hypo tonia, hyporeflexia, and a functioning bowel and bladder. Further questioning disclosed lower extremity dysesthesias. Nerve conduction studies showed slowed velocities, pro longed distal latencies and decreased amplitudes of all lower extremity nerves. Electro myography revealed denervation of all proximal and distal lower extremity musculature, with normal paraspinalis. Upper extremity studies were normal. Recently, 3 cases of ischaemic lumbosacral plexopathy, mimicking an incomplete SCI, have been reported. This distinction is particularly difficult in the poly trauma patient with multiple musculo skeletal injuries or prolonged recuperation time, in addition to a vascular insult, as in this patient. The involved anatomical considerations will be discussed. A review of the elec trodiagnostic data from 30 patients, with lower extremity weakness following acute ischaemia, revealed a 20% incidence of spinal cord compromise, but no evidence of a plexopathy. Key words: Ischaemia; Lumbosacral plexopathy; Electromyography. Recent advances in cardiovascular and trauma surgery have led to increased survi val of patients following cardiac and great vessel trauma or insult. -

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -
4-Brachial Plexus and Lumbosacral Plexus (Edited).Pdf
Color Code Brachial Plexus and Lumbosacral Important Doctors Notes Plexus Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of this lecture, the students should be able to : Describe the formation of brachial plexus (site, roots) List the main branches of brachial plexus Describe the formation of lumbosacral plexus (site, roots) List the main branches of lumbosacral plexus Describe the important Applied Anatomy related to the brachial & lumbosacral plexuses. Brachial Plexus Formation Playlist o It is formed in the posterior triangle of the neck. o It is the union of the anterior rami (or ventral) of the 5th ,6th ,7th ,8th cervical and the 1st thoracic spinal nerves. o The plexus is divided into 5 stages: • Roots • Trunks • Divisions • Cords • Terminal branches Really Tired? Drink Coffee! Brachial Plexus A P A P P A Brachial Plexus Trunks Divisions Cords o Upper (superior) trunk o o Union of the roots of Each trunk divides into Posterior cord: C5 & C6 anterior and posterior From the 3 posterior division divisions of the 3 trunks o o Middle trunk Lateral cord: From the anterior Continuation of the divisions of the upper root of C7 Branches and middle trunks o All three cords will give o Medial cord: o Lower (inferior) trunk branches in the axilla, It is the continuation of Union of the roots of the anterior division of C8 & T1 those will supply their respective regions. the lower trunk The Brachial Plexus Long Thoracic (C5,6,7) Anterior divisions Nerve to Subclavius(C5,6) Posterior divisions Dorsal Scapular(C5) Suprascapular(C5,6) upper C5 trunk Lateral Cord C6 middle (2LM) trunk C7 lower C8 trunk T1 Posterior Cord (ULTRA) Medial Cord (4MU) In the PowerPoint presentation this slide is animated. -
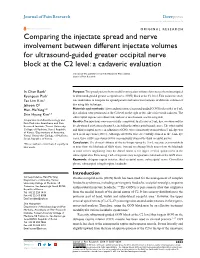
Comparing the Injectate Spread and Nerve
Journal name: Journal of Pain Research Article Designation: Original Research Year: 2018 Volume: 11 Journal of Pain Research Dovepress Running head verso: Baek et al Running head recto: Ultrasound-guided GON block open access to scientific and medical research DOI: http://dx.doi.org/10.2147/JPR.S17269 Open Access Full Text Article ORIGINAL RESEARCH Comparing the injectate spread and nerve involvement between different injectate volumes for ultrasound-guided greater occipital nerve block at the C2 level: a cadaveric evaluation In Chan Baek1 Purpose: The spread patterns between different injectate volumes have not yet been investigated Kyungeun Park1 in ultrasound-guided greater occipital nerve (GON) block at the C2 level. This cadaveric study Tae Lim Kim1 was undertaken to compare the spread pattern and nerve involvements of different volumes of Jehoon O2 dye using this technique. Hun-Mu Yang2,* Materials and methods: After randomization, ultrasound-guided GON blocks with 1 or 5 mL dye solution were performed at the C2 level on the right or left side of five fresh cadavers. The Shin Hyung Kim1,* suboccipital regions were dissected, and nerve involvement was investigated. 1 Department of Anesthesiology and Results: Ten injections were successfully completed. In all cases of 5 mL dye, we observed the Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University deeply stained posterior neck muscles, including the suboccipital triangle space. The suboccipital College of Medicine, Seoul, Republic and third occipital nerves, in addition to GONs, were consistently stained when 5-mL dye was 2 of Korea; Department of Anatomy, used in all injections (100%). Although all GONs were successfully stained in the 1-mL dye Yonsei University College of Medicine, Seoul, Republic of Korea cases, three of five injections (60%) concomitantly stained the third occipital nerves. -

Anatomy-Nerve Tracking
INJECTABLES ANATOMY www.aestheticmed.co.uk Nerve tracking Dr Sotirios Foutsizoglou on the anatomy of the facial nerve he anatomy of the human face has received enormous attention during the last few years, as a plethora of anti- ageing procedures, both surgical and non-surgical, are being performed with increasing frequency. The success of each of those procedures is greatly dependent on Tthe sound knowledge of the underlying facial anatomy and the understanding of the age-related changes occurring in the facial skeleton, ligaments, muscles, facial fat compartments, and skin. The facial nerve is the most important motor nerve of the face as it is the sole motor supply to all the muscles of facial expression and other muscles derived from the mesenchyme in the embryonic second pharyngeal arch.1 The danger zone for facial nerve injury has been well described. Confidence when approaching the nerve and its branches comes from an understanding of its three dimensional course relative to the layered facial soft tissue and being aware of surface anatomy landmarks and measurements as will be discussed in this article. Aesthetic medicine is not static, it is ever evolving and new exciting knowledge emerges every day unmasking the relationship of the ageing process and the macroscopic and microscopic (intrinsic) age-related changes. Sound anatomical knowledge, taking into consideration the natural balance between the different facial structures and facial layers, is fundamental to understanding these changes which will subsequently help us develop more effective, natural, long-standing and most importantly, safer rejuvenating treatments and procedures. The soft tissue of the face is arranged in five layers: 1) Skin; 2) Subcutaneous fat layer; 3) Superficial musculoaponeurotic system (SMAS); 4) Areolar tissue or loose connective tissue (most clearly seen in the scalp and forehead); 5) Deep fascia formed by the periosteum of facial bones and the fascial covering of the muscles of mastication (lateral face). -

Shoulder Anatomy & Clinical Exam
MSK Ultrasound - Spine - Incheon Terminal Orthopedic Private Clinic Yong-Hyun, Yoon C,T-spine Basic Advanced • Medial branch block • C-spine transforaminal block • Facet joint block • Thoracic paravertebral block • C-spine intra-discal injection • Superficial cervical plexus block • Vagus nerve block • Greater occipital nerve block(GON) • Third occipital nerve block(TON) • Hydrodissection • Brachial plexus(1st rib level) • Suboccipital nerve • Stellate ganglion block(SGB) • C1, C2 nerve root, C2 nerve • Brachial plexus block(interscalene) • Recurrent laryngeal nerve • Serratus anterior plane • Cervical nerve root Cervical facet joint Anatomy Diagnosis Cervical facet joint injection C-arm Ultrasound Cervical medial branch Anatomy Nerve innervation • Medial branch • Same level facet joint • Inferior level facet joint • Facet joint • Dual nerve innervation Cervical medial branch C-arm Ultrasound Cervical nerve root Anatomy Diagnosis • Motor • Sensory • Dermatome, myotome, fasciatome Cervical nerve root block C-arm Ultrasound Stallete ganglion block Anatomy Injection Vagus nerve Anatomy Injection L,S-spine Basic Advanced • Medial branch block • Lumbar sympathetic block • Facet joint block • Lumbar plexus block • Superior, inferior hypogastric nerve block • Caudal block • Transverse abdominal plane(TAP) block • Sacral plexus block • Epidural block • Hydrodissection • Interlaminal • Pudendal nerve • Transforaminal injection • Genitofemoral nerve • Superior, inferior cluneal nerve • Rectus abdominal sheath • Erector spinae plane Lumbar facet -
Cranial Nervesnerves
CranialCranial NervesNerves 1. Cranial nerves - overview: origin and peripheral distribution functional components and modality innervation zones I. Olfactory nerves, nn. olfactorii II. Optic nerve, n. opticus III. Oculomotor nerve, n. oculomotorius IV. Trochlear nerve, n. trochlearis V. Trigeminal nerve, n. trigeminus VI. Abducent nerve, n. abducens VII. Facial nerve, n. facialis VIII. Vestibulocochlear nerve, n. Vestibulocochlearis IX. Glossopharyngeal nerve, n. glossopharyngeus X. Vagus nerve, n. vagus XI. Accessory nerve, n. accessorius XII. Hypoglossal nerve, n. hypoglossus Cranial nerves CranialCranial nervesnerves 0. N. terminalis I. N. olfactorius II. N. opticus III. N. oculomotorius IV. N. trochlearis V. N. trigeminus VI. N. abducens VII. N. facialis VIII. N. vestibulocochlearis IX. N. glossopharyngeus X. N. vagus XI. N. accessorius XII. N. hypoglossus Prof. Dr. Nikolai Lazarov 2 Cranial nerves FunctionalFunctional classificationclassification purely sensory (afferent ): n. olfactorius n. opticus n. vestibulocochlearis purely motor (efferent): n. oculomotorius n. trochlearis n. abducens n. accessorius n. hypoglossus mixed (sensory&motor ): n. trigeminus n. facialis n. glossopharyngeus n. vagus autonomic (parasympathetic( ): n. oculomotorius n. facialis n. glossopharyngeus n. vagus Prof. Dr. Nikolai Lazarov 3 Cranial nerves AnatomicAnatomic relationshipsrelationships Location within the brainstem: ventrally: n. olfactorius n. opticus n. oculomotorius n. abducens n. hypoglossus laterally: n. trigeminus -

The Spinal Nerves That Constitute the Plexus Lumbosacrales of Porcupines (Hystrix Cristata)
Original Paper Veterinarni Medicina, 54, 2009 (4): 194–197 The spinal nerves that constitute the plexus lumbosacrales of porcupines (Hystrix cristata) A. Aydin, G. Dinc, S. Yilmaz Faculty of Veterinary Medicine, Firat University, Elazig, Turkey ABSTRACT: In this study, the spinal nerves that constitute the plexus lumbosacrales of porcupines (Hystrix cristata) were investigated. Four porcupines (two males and two females) were used in this work. Animals were appropriately dissected and the spinal nerves that constitute the plexus lumbosacrales were examined. It was found that the plexus lumbosacrales of the porcupines was formed by whole rami ventralis of L1, L2, L3, L4, S1 and a fine branch from T15 and S2. The rami ventralis of T15 and S2 were divided into two branches. The caudal branch of T15 and cranial branch of S2 contributed to the plexus lumbosacrales. At the last part of the plexus lumbosacrales, a thick branch was formed by contributions from the whole of L4 and S1, and a branch from each of L3 and S2. This root gives rise to the nerve branches which are disseminated to the posterior legs (caudal glu- teal nerve, caudal cutaneous femoral nerve, ischiadic nerve). Thus, the origins of spinal nerves that constitute the plexus lumbosacrales of porcupine differ from rodantia and other mammals. Keywords: lumbosacral plexus; nerves; posterior legs; porcupines (Hystrix cristata) List of abbreviations M = musculus, T = thoracal, L = lumbal, S = sacral, Ca = caudal The porcupine is a member of the Hystricidae fam- were opened by an incision made along the linea ily, a small group of rodentia (Karol, 1963; Weichert, alba and a dissection of the muscles. -

New Insights in Lumbosacral Plexopathy
New Insights in Lumbosacral Plexopathy Kerry H. Levin, MD Gérard Said, MD, FRCP P. James B. Dyck, MD Suraj A. Muley, MD Kurt A. Jaeckle, MD 2006 COURSE C AANEM 53rd Annual Meeting Washington, DC Copyright © October 2006 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 PRINTED BY JOHNSON PRINTING COMPANY, INC. C-ii New Insights in Lumbosacral Plexopathy Faculty Kerry H. Levin, MD P. James. B. Dyck, MD Vice-Chairman Associate Professor Department of Neurology Department of Neurology Head Mayo Clinic Section of Neuromuscular Disease/Electromyography Rochester, Minnesota Cleveland Clinic Dr. Dyck received his medical degree from the University of Minnesota Cleveland, Ohio School of Medicine, performed an internship at Virginia Mason Hospital Dr. Levin received his bachelor of arts degree and his medical degree from in Seattle, Washington, and a residency at Barnes Hospital and Washington Johns Hopkins University in Baltimore, Maryland. He then performed University in Saint Louis, Missouri. He then performed fellowships at a residency in internal medicine at the University of Chicago Hospitals, the Mayo Clinic in peripheral nerve and electromyography. He is cur- where he later became the chief resident in neurology. He is currently Vice- rently Associate Professor of Neurology at the Mayo Clinic. Dr. Dyck is chairman of the Department of Neurology and Head of the Section of a member of several professional societies, including the AANEM, the Neuromuscular Disease/Electromyography at Cleveland Clinic. Dr. Levin American Academy of Neurology, the Peripheral Nerve Society, and the is also a professor of medicine at the Cleveland Clinic College of Medicine American Neurological Association. -

A Step Towards Stereotactic Navigation During Pelvic Surgery: 3D Nerve Topography
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Surgical Endoscopy and Other Interventional Techniques https://doi.org/10.1007/s00464-018-6086-3 A step towards stereotactic navigation during pelvic surgery: 3D nerve topography A. R. Wijsmuller1,2 · C. Giraudeau3 · J. Leroy4 · G. J. Kleinrensink5 · E. Rociu6 · L. G. Romagnolo7 · A. G. F. Melani7,8,9 · V. Agnus2 · M. Diana3 · L. Soler3 · B. Dallemagne2 · J. Marescaux2 · D. Mutter2 Received: 10 May 2017 / Accepted: 1 February 2018 © The Author(s) 2018. This article is an open access publication Abstract Background Long-term morbidity after multimodal treatment for rectal cancer is suggested to be mainly made up by nerve- injury-related dysfunctions. Stereotactic navigation for rectal surgery was shown to be feasible and will be facilitated by highlighting structures at risk of iatrogenic damage. The aim of this study was to investigate the ability to make a 3D map of the pelvic nerves with magnetic resonance imaging (MRI). Methods A systematic review was performed to identify a main positional reference for each pelvic nerve and plexus. The nerves were manually delineated in 20 volunteers who were scanned with a 3-T MRI. The nerve identifiability rate and the likelihood of nerve identification correctness were determined. Results The analysis included 61 studies on pelvic nerve anatomy. A main positional reference was defined for each nerve. On MRI, the sacral nerves, the lumbosacral plexus, and the obturator nerve could be identified bilaterally in all volunteers. The sympathetic trunk could be identified in 19 of 20 volunteers bilaterally (95%). -

Surgical Treatment of Bronchial Asthma by Resection of the Laryngeal Nerve
Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, Massoud Mirshahi To cite this version: Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, et al.. Surgical treatment of bronchial asthma by resection of the laryngeal nerve. BMC Surgery, BioMed Central, 2015, 15 (1), pp.109. 10.1186/s12893-015-0093-2. inserm-01264486 HAL Id: inserm-01264486 https://www.hal.inserm.fr/inserm-01264486 Submitted on 29 Jan 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Kurbon et al. BMC Surgery (2015) 15:109 DOI 10.1186/s12893-015-0093-2 TECHNICAL ADVANCE Open Access Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon1, Hamza Dodariyon1, Abdumalik Davlatov1, Sitora Janobilova1, Amu Therwath2 and Massoud Mirshahi1,2* Abstract Background: Management of asthma in chronically affected patients is a serious health problem. Our aim was to show that surgical treatment of chronic bronchial asthma by unilateral resection of the internal branch of the superior laryngeal nerve (ib-SLN) is an adequateand lasting remedial response. Patients and methods: In a retrospective study, 41 (26 male and 15 female) patients with bronchial chronic asthma were treated surgically during the period between 2005 and 2013. -

A Case Report of an Enlarged Suboccipital Nerve with Cutaneous Branch
Open Access Case Report DOI: 10.7759/cureus.2933 A Case Report of an Enlarged Suboccipital Nerve with Cutaneous Branch Sasha Lake 1 , Joe Iwanaga 2 , Rod J. Oskouian 3 , Marios Loukas 4 , R. Shane Tubbs 5 1. Anatomical Studies, St. George's, St. George, GRD 2. Medical Education and Simulation, Seattle Science Foundation, Seattle, USA 3. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 4. Anatomical Sciences, St. George's University, St. George's, GRD 5. Neurosurgery, Seattle Science Foundation, Seattle, USA Corresponding author: Joe Iwanaga, [email protected] Abstract Variations of the suboccipital nerve are infrequently reported. This nerve derived from the C1 spinal nerve is usually a small branch that primarily innervates the short suboccipital muscles. During the routine dissection of the occipital region in an adult cadaver, a vastly enlarged left-sided suboccipital nerve was identified. The nerve innervated the short suboccipital muscles and overlying semispinalis capitis in normal fashion. However, it continued cranially to end in the overlying skin of the occiput. Although not normally thought to have a cutaneous branch, recalcitrant occipital neuralgia might be due to such a variant branch. Future studies are necessary to further elucidate this proposed pathomechanism. Categories: Neurology, Pathology Keywords: suboccipital nerve, c1 nerve, occiput cutaneous innervation, sensory suboccipital nerve Introduction The suboccipital nerve is the dorsal ramus of C1. This nerve is found between the skull and atlas and within the suboccipital triangle. Here, it is positioned between the posterior arch of the atlas and vertebral artery bordering the nerve inferiorly and superiorly, respectively [1]. The suboccipital nerve innervates the rectus capitis posterior major and minor, obliquus capitis superior, obliquus capitis inferior, and semispinalis capitis.