Neural Control of Swallowing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE DIGESTIVE SYSTEM: Introduction and Upper GI
THE DIGESTIVE SYSTEM: Introduction and upper GI Dalay Olson Ph.D Office: Jackson Hall 3-120 Office hours: Monday 2-3pm INTRODUCTION TO GI LEARNING OBJECTIVES 3 Distinguish between the wall layers of the esophagus and those classically represented by the small intestine. ESOPHAGUS STRUCTURE UPPER THIRD ESOPHAGUS STRUCTURE LOWER TWO-THIRDS 4 Describe the voluntary and reflex components of swallowing. PHASES OF SWALLOWING Swallowing is integrated in the medulla oblongata. Voluntary Phase Pharyngeal Phase Esophageal Phase The swallowing reflex requires input from sensory afferent nerves, somatic motor nerves and autonomic nerves. VOLUNTARY PHASE The tongue pushes the bolus of food back and upwards towards the back of the mouth. Once the food touches the soft palate and the back of the mouth it triggers the swallowing reflex. This is the stimulus! PHARYNGEAL PHASE • Once the food touches the soft palate and the back of the mouth it triggers the swallowing reflex. This is the stimulus! • The medulla oblongata (control center) then initiates the swallowing reflex causing the soft palate to elevate, closing of the glottis and opening of the esophageal sphincter (response). • Once the food moves into the esophagus the sphincter closes once again. The glottis then opens again and breathing resumes. ESOPHAGEAL PHASE 1. Food moves along the esophagus by peristalsis (waves of smooth muscle contractions) • If the food gets stuck, short reflexes will continue peristalsis. • Myogenic reflex (you will learn about this later) produces contractions that move food forward. 2. As the bolus of food moves toward the stomach the lower esophageal sphincter relaxes and opens allowing the food to move into the stomach. -

The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’S Disease
life Review The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’s Disease Gianfranco Natale 1,2,* , Larisa Ryskalin 1 , Gabriele Morucci 1 , Gloria Lazzeri 1, Alessandro Frati 3,4 and Francesco Fornai 1,4 1 Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, 56126 Pisa, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (G.L.); [email protected] (F.F.) 2 Museum of Human Anatomy “Filippo Civinini”, University of Pisa, 56126 Pisa, Italy 3 Neurosurgery Division, Human Neurosciences Department, Sapienza University of Rome, 00135 Rome, Italy; [email protected] 4 Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) Neuromed, 86077 Pozzilli, Italy * Correspondence: [email protected] Abstract: The gastrointestinal (GI) tract is provided with a peculiar nervous network, known as the enteric nervous system (ENS), which is dedicated to the fine control of digestive functions. This forms a complex network, which includes several types of neurons, as well as glial cells. Despite extensive studies, a comprehensive classification of these neurons is still lacking. The complexity of ENS is magnified by a multiple control of the central nervous system, and bidirectional communication between various central nervous areas and the gut occurs. This lends substance to the complexity of the microbiota–gut–brain axis, which represents the network governing homeostasis through nervous, endocrine, immune, and metabolic pathways. The present manuscript is dedicated to Citation: Natale, G.; Ryskalin, L.; identifying various neuronal cytotypes belonging to ENS in baseline conditions. -

IDP Biological Systems Gastrointestinal System
IDP Biological Systems Gastrointestinal System Section Coordinator: Jerome W. Breslin, PhD, Assistant Professor of Physiology, MEB 7208, 504-568-2669, [email protected] Overall Learning Objectives 1. Characterize the important anatomical features of the GI system in relation to GI function. 2. Describe the molecular and cellular mechanisms underlying GI motility. Highlight the neural and endocrine regulatory mechanisms. Characterize the different types of GI motility in different segments of the GI tract. 3. Define the major characteristics and temporally relate the cephalic, gastric, and intestinal phases of GI tract regulation. 4. For carbohydrates, proteins, fats, vitamins, minerals, and oral drugs, differentiate the processes of ingestion, digestion, absorption, secretion, and excretion, including the location in the GI tract where each process occurs. 5. Contrast the sympathetic and parasympathetic modulation of the enteric nervous system and the effector organs of the GI tract. 6. Describe the similarities and differences in regulating gastrointestinal function by nerves, hormones, and paracrine regulators. Include receptors, proximity, and local vs. global specificity. 7. Understand the basic mechanisms underlying several common GI disorders and related treatment strategies. Learning Objectives for Specific Hours: Hour 1 – Essential Concepts: Cellular transport mechanisms and Mechanisms of Force Generation 1. Describe the composition of cell membranes and how distribution of phospholipids and proteins influence membrane permeability of ions, hydrophilic, and hydrophobic compounds. 2. Using a cell membrane as an example, define a reflection coefficient, and explain how the relative permeability of a cell to water and solutes will generate osmotic pressure. Contrast the osmotic pressure generated across a cell membrane by a solution of particles that freely cross the membrane with that of a solution with the same osmolality, but particles that cannot cross the cell membrane. -

Questions on Human Anatomy
Standard Medical Text-books. ROBERTS’ PRACTICE OF MEDICINE. The Theory and Practice of Medicine. By Frederick T. Roberts, m.d. Third edi- tion. Octavo. Price, cloth, $6.00; leather, $7.00 Recommended at University of Pennsylvania. Long Island College Hospital, Yale and Harvard Colleges, Bishop’s College, Montreal; Uni- versity of Michigan, and over twenty other medical schools. MEIGS & PEPPER ON CHILDREN. A Practical Treatise on Diseases of Children. By J. Forsyth Meigs, m.d., and William Pepper, m.d. 7th edition. 8vo. Price, cloth, $6.00; leather, $7.00 Recommended at thirty-five of the principal medical colleges in the United States, including Bellevue Hospital, New York, University of Pennsylvania, and Long Island College Hospital. BIDDLE’S MATERIA MEDICA. Materia Medica, for the Use of Students and Physicians. By the late Prof. John B Biddle, m.d., Professor of Materia Medica in Jefferson Medical College, Phila- delphia. The Eighth edition. Octavo. Price, cloth, $4.00 Recommended in colleges in all parts of the UnitedStates. BYFORD ON WOMEN. The Diseases and Accidents Incident to Women. By Wm. H. Byford, m.d., Professor of Obstetrics and Diseases of Women and Children in the Chicago Medical College. Third edition, revised. 164 illus. Price, cloth, $5.00; leather, $6.00 “ Being particularly of use where questions of etiology and general treatment are concerned.”—American Journal of Obstetrics. CAZEAUX’S GREAT WORK ON OBSTETRICS. A practical Text-book on Midwifery. The most complete book now before the profession. Sixth edition, illus. Price, cloth, $6.00 ; leather, $7.00 Recommended at nearly fifty medical schools in the United States. -

Pathophysiology, 6Th Edition
McCance: Pathophysiology, 6th Edition Chapter 38: Structure and Function of the Digestive System Key Points – Print SUMMARY REVIEW The Gastrointestinal Tract 1. The major functions of the gastrointestinal tract are the mechanical and chemical breakdown of food and the absorption of digested nutrients. 2. The gastrointestinal tract is a hollow tube that extends from the mouth to the anus. 3. The walls of the gastrointestinal tract have several layers: mucosa, muscularis mucosae, submucosa, tunica muscularis (circular muscle and longitudinal muscle), and serosa. 4. Except for swallowing and defecation, which are controlled voluntarily, the functions of the gastrointestinal tract are controlled by extrinsic and intrinsic autonomic nerves (enteric plexus) and intestinal hormones. 5. Digestion begins in the mouth, with chewing and salivation. The digestive component of saliva is α-amylase, which initiates carbohydrate digestion. 6. The esophagus is a muscular tube that transports food from the mouth to the stomach. The tunica muscularis in the upper part of the esophagus is striated muscle, and that in the lower part is smooth muscle. 7. Swallowing is controlled by the swallowing center in the reticular formation of the brain. The two phases of swallowing are the oropharyngeal phase (voluntary swallowing) and the esophageal phase (involuntary swallowing). 8. Food is propelled through the gastrointestinal tract by peristalsis: waves of sequential relaxations and contractions of the tunica muscularis. 9. The lower esophageal sphincter opens to admit swallowed food into the stomach and then closes to prevent regurgitation of food back into the esophagus. 10. The stomach is a baglike structure that secretes digestive juices, mixes and stores food, and propels partially digested food (chyme) into the duodenum. -

Anatomy-Nerve Tracking
INJECTABLES ANATOMY www.aestheticmed.co.uk Nerve tracking Dr Sotirios Foutsizoglou on the anatomy of the facial nerve he anatomy of the human face has received enormous attention during the last few years, as a plethora of anti- ageing procedures, both surgical and non-surgical, are being performed with increasing frequency. The success of each of those procedures is greatly dependent on Tthe sound knowledge of the underlying facial anatomy and the understanding of the age-related changes occurring in the facial skeleton, ligaments, muscles, facial fat compartments, and skin. The facial nerve is the most important motor nerve of the face as it is the sole motor supply to all the muscles of facial expression and other muscles derived from the mesenchyme in the embryonic second pharyngeal arch.1 The danger zone for facial nerve injury has been well described. Confidence when approaching the nerve and its branches comes from an understanding of its three dimensional course relative to the layered facial soft tissue and being aware of surface anatomy landmarks and measurements as will be discussed in this article. Aesthetic medicine is not static, it is ever evolving and new exciting knowledge emerges every day unmasking the relationship of the ageing process and the macroscopic and microscopic (intrinsic) age-related changes. Sound anatomical knowledge, taking into consideration the natural balance between the different facial structures and facial layers, is fundamental to understanding these changes which will subsequently help us develop more effective, natural, long-standing and most importantly, safer rejuvenating treatments and procedures. The soft tissue of the face is arranged in five layers: 1) Skin; 2) Subcutaneous fat layer; 3) Superficial musculoaponeurotic system (SMAS); 4) Areolar tissue or loose connective tissue (most clearly seen in the scalp and forehead); 5) Deep fascia formed by the periosteum of facial bones and the fascial covering of the muscles of mastication (lateral face). -

Earthworm Dissection External Anatomy Examine Your Earthworm and Determine the Dorsal and Ventral Sides
Name(s): ___________________________________________Date:________ Earthworm Dissection External Anatomy Examine your earthworm and determine the dorsal and ventral sides. Locate the two openings on the ventral surface of the earthworm. Locate the openings toward the anterior of the worm which are the s perm ducts. Locate the openings near the clitellum which are the g enital setae . Locate the dark line that runs down the dorsal side of the worm, this is the dorsal blood vessel. The ventral blood vessel can be seen on the underside of the worm, though it is usually not as dark . Locate the worm’s anus on the far posterior end of the worm. Note the swelling of the earthworm near its anterior side - this is the clitellum. Label the earthworm pictured. A_____________________________ B _____________________________ C _____________________________ D _____________________________ Internal Anatomy 1. Place the specimen in the dissecting pan D ORSAL side up. 2. Locate the clitellum and insert the tip of the scissors about 3 cm posterior. 3. Cut carefully all the way up to the head. Try to keep the scissors pointed up, and only cut through the skin. 4. Spread the skin of the worm out, use a teasing needle to gently tear the s epta (little thread like structures that hold the skin to organs below it) 5. Place pins in the skin to hold it apart – set them at an angle so they aren’t in the way of your view. Reproductive System The first structures you probably see are the s eminal vesicles. They are cream colored and located toward the anterior of the worm. -
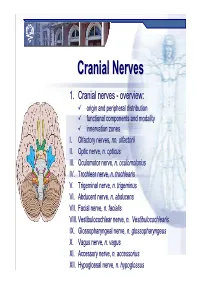
Cranial Nervesnerves
CranialCranial NervesNerves 1. Cranial nerves - overview: origin and peripheral distribution functional components and modality innervation zones I. Olfactory nerves, nn. olfactorii II. Optic nerve, n. opticus III. Oculomotor nerve, n. oculomotorius IV. Trochlear nerve, n. trochlearis V. Trigeminal nerve, n. trigeminus VI. Abducent nerve, n. abducens VII. Facial nerve, n. facialis VIII. Vestibulocochlear nerve, n. Vestibulocochlearis IX. Glossopharyngeal nerve, n. glossopharyngeus X. Vagus nerve, n. vagus XI. Accessory nerve, n. accessorius XII. Hypoglossal nerve, n. hypoglossus Cranial nerves CranialCranial nervesnerves 0. N. terminalis I. N. olfactorius II. N. opticus III. N. oculomotorius IV. N. trochlearis V. N. trigeminus VI. N. abducens VII. N. facialis VIII. N. vestibulocochlearis IX. N. glossopharyngeus X. N. vagus XI. N. accessorius XII. N. hypoglossus Prof. Dr. Nikolai Lazarov 2 Cranial nerves FunctionalFunctional classificationclassification purely sensory (afferent ): n. olfactorius n. opticus n. vestibulocochlearis purely motor (efferent): n. oculomotorius n. trochlearis n. abducens n. accessorius n. hypoglossus mixed (sensory&motor ): n. trigeminus n. facialis n. glossopharyngeus n. vagus autonomic (parasympathetic( ): n. oculomotorius n. facialis n. glossopharyngeus n. vagus Prof. Dr. Nikolai Lazarov 3 Cranial nerves AnatomicAnatomic relationshipsrelationships Location within the brainstem: ventrally: n. olfactorius n. opticus n. oculomotorius n. abducens n. hypoglossus laterally: n. trigeminus -

Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Enteric Nervous System (ENS): 1) Myenteric (Auerbach) plexus & 2) Submucosal (Meissner’s) plexus à both triggered by sensory neurons with chemo- and mechanoreceptors in the mucosal epithelium; effector motors neurons of the myenteric plexus control contraction/motility of the GI tract, and effector motor neurons of the submucosal plexus control secretion of GI mucosa & organs. Although ENS neurons can function independently, they are subject to regulation by ANS. Autonomic Nervous System (ANS): 1) parasympathetic (rest & digest) – can innervate the GI tract and form connections with ENS neurons that promote motility and secretion, enhancing/speeding up the process of digestion 2) sympathetic (fight or flight) – can innervate the GI tract and inhibit motility & secretion by inhibiting neurons of the ENS Sections and dimensions of the GI tract (alimentary canal): Esophagus à ~ 10 inches Stomach à ~ 12 inches and holds ~ 1-2 L (full) up to ~ 3-4 L (distended) Duodenum à first 10 inches of the small intestine Jejunum à next 3 feet of small intestine (when smooth muscle tone is lost upon death, extends to 8 feet) Ileum à final 6 feet of small intestine (when smooth muscle tone is lost upon death, extends to 12 feet) Large intestine à 5 feet General Histology of the GI Tract: 4 layers – Mucosa, Submucosa, Muscularis Externa, and Serosa Mucosa à epithelium, lamina propria (areolar connective tissue), & muscularis mucosae Submucosa à areolar connective tissue Muscularis externa à skeletal muscle (in select parts of the tract); smooth muscle (at least 2 layers – inner layer of circular muscle and outer layer of longitudinal muscle; stomach has a third layer of oblique muscle under the circular layer) Serosa à superficial layer made of areolar connective tissue and simple squamous epithelium (a.k.a. -

6. the Pharynx the Pharynx, Which Forms the Upper Part of the Digestive Tract, Consists of Three Parts: the Nasopharynx, the Oropharynx and the Laryngopharynx
6. The Pharynx The pharynx, which forms the upper part of the digestive tract, consists of three parts: the nasopharynx, the oropharynx and the laryngopharynx. The principle object of this dissection is to observe the pharyngeal constrictors that form the back wall of the vocal tract. Because the cadaver is lying face down, we will consider these muscles from the back. Figure 6.1 shows their location. stylopharyngeus suuperior phayngeal constrictor mandible medial hyoid bone phayngeal constrictor inferior phayngeal constrictor Figure 6.1. Posterior view of the muscles of the pharynx. Each of the three pharyngeal constrictors has a left and right part that interdigitate (join in fingerlike branches) in the midline, forming a raphe, or union. This raphe forms the back wall of the pharynx. The superior pharyngeal constrictor is largely in the nasopharynx. It has several origins (some texts regard it as more than one muscle) one of which is the medial pterygoid plate. It assists in the constriction of the nasopharynx, but has little role in speech production other than helping form a site against which the velum may be pulled when forming a velic closure. The medial pharyngeal constrictor, which originates on the greater horn of the hyoid bone, also has little function in speech. To some extent it can be considered as an elevator of the hyoid bone, but its most important role for speech is simply as the back wall of the vocal tract. The inferior pharyngeal constrictor also performs this function, but plays a more important role constricting the pharynx in the formation of pharyngeal consonants. -

Surgical Treatment of Bronchial Asthma by Resection of the Laryngeal Nerve
Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, Massoud Mirshahi To cite this version: Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, et al.. Surgical treatment of bronchial asthma by resection of the laryngeal nerve. BMC Surgery, BioMed Central, 2015, 15 (1), pp.109. 10.1186/s12893-015-0093-2. inserm-01264486 HAL Id: inserm-01264486 https://www.hal.inserm.fr/inserm-01264486 Submitted on 29 Jan 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Kurbon et al. BMC Surgery (2015) 15:109 DOI 10.1186/s12893-015-0093-2 TECHNICAL ADVANCE Open Access Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon1, Hamza Dodariyon1, Abdumalik Davlatov1, Sitora Janobilova1, Amu Therwath2 and Massoud Mirshahi1,2* Abstract Background: Management of asthma in chronically affected patients is a serious health problem. Our aim was to show that surgical treatment of chronic bronchial asthma by unilateral resection of the internal branch of the superior laryngeal nerve (ib-SLN) is an adequateand lasting remedial response. Patients and methods: In a retrospective study, 41 (26 male and 15 female) patients with bronchial chronic asthma were treated surgically during the period between 2005 and 2013. -

Diabetic Ketoacidosis Associated with Guillain-Barre Syndromewith
CASE REPORT Diabetic Ketoacidosis Associated with Guillain-Barre Syndromewith AutonomicDysfunction Setsuko Fujiwara, Hiroyuki Oshika, Kenzo Motoki, Kenji Kubo*, Yukiaki Ryujin*, Masahiro Shinozaki**, Takuzo Hano*** and Ichiro Nishio*** Abstract Case Report A37-year-old womanwas admitted in a comatosestate, In March 1996, a 37-year-old womanwas admitted to Koyo after exhibiting fever and diarrhea. Diabetic ketoacidosis Hospital in a comatose state after fever, diarrhea and vomiting was diagnosed due to an increased blood glucose level (672 of 1-week duration. Diabetes mellitus was diagnosed in 1990, mg/dl), metabolic addosis, and positive urinary ketone bod- and the patient had taken anti-diabetic drugs for five years, but ies. On the fifth hospital day, despite recovery from the criti- follow-up was discontinued in 1995. She had no episodes of cal state of ketoacidosis, the patient suffered from dyspha- neurological deficit or fainting and was workingas a nurse. gia, hypesthesia and motor weakness, followed by respira- On admission, Kussmaul's breathing, blood pressure of 96/ tory failure. Cerebrospinal fluid analysis was suggestive of 56 mmHg,and a heart rate of 122/min were observed. DKA Guillain-Barre syndrome (GBS). Autonomic dysfunction was diagnosed on the basis of an increased blood glucose level was manifested as tachycardia and mild hypertension in (672 mg/dl), severe metabolic acidosis (arterial blood gas analy- the acute stage. Marked orthostatic hypotension persisted sis: pH 6.703, PCO2 13.8 mmHg, PO2 281.4 mmHg, HCO3 1.7 long after paresis was improved, indicating an atypical clini- jjmol//, BE -36.3 jimol//) and urinary ketone bodies. Other labo- cal course of GBS.