Muscles Involved in Respiration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part 1 the Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3
ECA1 7/18/06 6:30 PM Page 1 Part 1 The Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3 Surface anatomy and surface markings The experienced clinician spends much of his working life relating the surface anatomy of his patients to their deep structures (Fig. 1; see also Figs. 11 and 22). The following bony prominences can usually be palpated in the living subject (corresponding vertebral levels are given in brackets): •◊◊superior angle of the scapula (T2); •◊◊upper border of the manubrium sterni, the suprasternal notch (T2/3); •◊◊spine of the scapula (T3); •◊◊sternal angle (of Louis) — the transverse ridge at the manubrio-sternal junction (T4/5); •◊◊inferior angle of scapula (T8); •◊◊xiphisternal joint (T9); •◊◊lowest part of costal margin—10th rib (the subcostal line passes through L3). Note from Fig. 1 that the manubrium corresponds to the 3rd and 4th thoracic vertebrae and overlies the aortic arch, and that the sternum corre- sponds to the 5th to 8th vertebrae and neatly overlies the heart. Since the 1st and 12th ribs are difficult to feel, the ribs should be enu- merated from the 2nd costal cartilage, which articulates with the sternum at the angle of Louis. The spinous processes of all the thoracic vertebrae can be palpated in the midline posteriorly, but it should be remembered that the first spinous process that can be felt is that of C7 (the vertebra prominens). The position of the nipple varies considerably in the female, but in the male it usually lies in the 4th intercostal space about 4in (10cm) from the midline. -

Slipping Rib Syndrome
Slipping Rib Syndrome Jackie Dozier, BS Edited by Lisa E McMahon, MD FACS FAAP David M Notrica, MD FACS FAAP Case Presentation AA is a 12 year old female who presented with a 7 month history of right-sided chest/rib pain. She states that the pain was not preceded by trauma and she had never experienced pain like this before. She has been seen in the past by her pediatrician, chiropractor, and sports medicine physician for her pain. In May 2012, she was seen in the ER after having manipulations done on her ribs by a sports medicine physician. Pain at that time was constant throughout the day and kept her from sleeping. However, it was relieved with hydrocodone/acetaminophen in the ER. Case Presentation Over the following months, the pain became progressively worse and then constant. She also developed shortness of breath. She is a swimmer and says she has had difficulty practicing due to the pain and SOB. AA was seen by a pediatric surgeon and scheduled for an interventional pain management service consult for a test injection. Following good temporary relief by local injection, she was scheduled costal cartilage removal to treat her pain. What is Slipping Rib Syndrome? •Slipping Rib Syndrome (SRS) is caused by hypermobility of the anterior ends of the false rib costal cartilages, which leads to slipping of the affected rib under the superior adjacent rib. •SRS an lead to irritation of the intercostal nerve or strain of the muscles surrounding the rib. •SRS is often misdiagnosed and can lead to months or years of unresolved abdominal and/or thoracic pain. -

Netter's Anatomy Flash Cards – Section 7 – List 4Th Edition
Netter's Anatomy Flash Cards – Section 7 – List 4th Edition https://www.memrise.com/course/1577594/ Section 7 Lower Limb (72 cards) Plate 7-1 Hip (Coxal) Bone: Lateral View 1.1 Posterior superior iliac spine 1.2 Posterior inferior iliac spine 1.3 Greater sciatic notch 1.4 Body of ilium 1.5 Body of ischium 1.6 Ischial tuberosity 1.7 Pubic tubercle 1.8 Acetabulum 1.9 Iliac crest Plate 7-2 Hip (Coxal) Bone: Medial View 2.1 Wing (ala) of ilium (iliac fossa) 2.2 Pecten pubis (pectineal line) 2.3 Ramus of ischium 2.4 Lesser sciatic notch 2.5 Ischial spine 2.6 Articular surface (for sacrum) 2.7 Iliac tuberosity Plate 7-3 Hip Joint: Lateral View 3.1 Lunate (articular) surface of acetabulum 3.2 Articular cartilage 3.3 Head of femur 3.4 Ligament of head of femur (cut) 3.5 Obturator membrane 3.6 Acetabular labrum (fibrocartilaginous) Plate 7-4 Hip Joint: Anterior and Posterior Views 4.1 Iliofemoral ligament (Y ligament of Bigelow) 4.2 Pubofemoral ligament 4.3 Iliofemoral ligament 4.4 Ischiofemoral ligament Plate 7-5 Femur 5.1 Greater trochanter 5.2 Shaft (body) 5.3 Lateral epicondyle 5.4 Lateral condyle 5.5 Medial condyle 5.6 Medial epicondyle 5.7 Adductor tubercle 5.8 Linea aspera (Medial lip; Lateral lip) 5.9 Lesser trochanter 5.10 Intertrochanteric crest 5.11 Neck 5.12 Head Plate 7-6 Tibia and Fibula 6.1 Lateral condyle 6.2 Apex, Head, and Neck of fibula 6.3 Fibula 6.4 Lateral malleolus 6.5 Medial malleolus 6.6 Tibia 6.7 Tibial tuberosity 6.8 Medial condyle 6.9 Superior articular surfaces (medial and lateral facets) 6.10 Malleolar fossa of lateral -
33. Spinal Nerves. Cervical Plexus
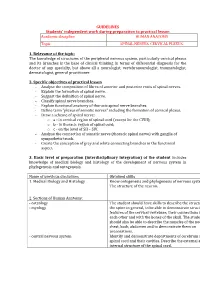
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic SPINAL NERVES. CERVICAL PLEXUS. 1. Relevance of the topic: The knowledge of structures of the peripheral nervous system, particularly cervical plexus and its branches is the base of clinical thinking in terms of differential diagnosis for the doctor of any specialty, but above all a neurologist, vertebroneurologist, traumatologist, dermatologist, general practitioner. 2. Specific objectives of practical lesson - Analyse the composition of fibres of anterior and posterior roots of spinal nerves. - Explain the formation of spinal nerve. - Suggest the definition of spinal nerve. - Classify spinal nerve branches. - Explain functional anatomy of thoracic spinal nerve branches. - Define term "plexus of somatic nerves" including the formation of cervical plexus. - Draw a scheme of spinal nerve: o а - in cervical region of spinal cord (except for the CVIII); o b - in thoracic region of spinal cord; o c - on the level of SII – SIV. - Analyse the connection of somatic nerve (thoracic spinal nerve) with ganglia of sympathetic trunk. - Create the conception of grey and white connecting branches in the functional aspect. 3. Basic level of preparation (interdisciplinary integration) of the student includes knowledge of medical biology and histology of the development of nervous system in phylogenesis and ontogenesis. Name of previous disciplines Obtained skills 1. Medical Biology and Histology Know ontogenesis and phylogenesis of nervous system. The structure of the neuron. 2. Sections of Human Anatomy: - osteology The student should have skills to describe the structure of - myology the spine in general, to be able to demonstrate structural features of the cervical vertebrae, their connections with each other and with the bones of the skull. -

The Supra-Iliac Anterior Quadratus Lumborum Block
Can J Anesth/J Can Anesth https://doi.org/10.1007/s12630-019-01312-z REPORTS OF ORIGINAL INVESTIGATIONS The supra-iliac anterior quadratus lumborum block: a cadaveric study and case series Le bloc du muscle carre´ des lombes ante´rieur par approche supra-iliaque : une e´tude cadave´rique et une se´rie de cas Hesham Elsharkawy, MD, MBA, MSc . Kariem El-Boghdadly, MBBS, BSc, FRCA, EDRA, MSc . Theresa J. Barnes, MD, MPH . Richard Drake, PhD . Kamal Maheshwari, MD, MPH . Loran Mounir Soliman, MD . Jean-Louis Horn, MD . Ki Jinn Chin, MD, FRCPC Received: 9 July 2018 / Revised: 10 December 2018 / Accepted: 10 December 2018 Ó Canadian Anesthesiologists’ Society 2019 Abstract Methods Ultrasound-guided bilateral supra-iliac anterior Purpose The local anesthetic injectate spread with fascial QL blocks were performed with 30 mL of India ink dye in plane blocks and corresponding clinical outcomes may six fresh adult cadavers. Cadavers were subsequently vary depending on the site of injection. We developed and dissected to determine distribution of the dye. In five evaluated a supra-iliac approach to the anterior quadratus patients undergoing hip surgery, a unilateral supra-iliac lumborum (QL) block and hypothesized that this single anterior QL block with 25 mL ropivacaine 0.5% followed injection might successfully block the lumbar and sacral by a continuous catheter infusion was performed. Patients plexus in cadavers and provide analgesia for patients were clinically assessed daily for block efficacy. undergoing hip surgery. Results The cadaveric injections showed consistent dye involvement of the majority of the branches of the lumbar plexus, including the femoral nerve, lateral femoral cutaneous nerve, ilioinguinal nerve, and iliohypogastric Permission to use images was obtained from the Cleveland Clinic nerve. -

Structure of the Human Body
STRUCTURE OF THE HUMAN BODY Vertebral Levels 2011 - 2012 Landmarks and internal structures found at various vertebral levels. Vertebral Landmark Internal Significance Level • Bifurcation of common carotid artery. C3 Hyoid bone Superior border of thyroid C4 cartilage • Larynx ends; trachea begins • Pharynx ends; esophagus begins • Inferior thyroid A crosses posterior to carotid sheath. • Middle cervical sympathetic ganglion C6 Cricoid cartilage behind inf. thyroid a. • Inferior laryngeal nerve enters the larynx. • Vertebral a. enters the transverse. Foramen of C 6. • Thoracic duct reaches its greatest height C7 Vertebra prominens • Isthmus of thyroid gland Sternoclavicular joint (it is a • Highest point of apex of lung. T1 finger's breadth below the bismuth of the thyroid gland T1-2 Superior angle of the scapula T2 Jugular notch T3 Base of spine of scapula • Division between superior and inferior mediastinum • Ascending aorta ends T4 Sternal angle (of Louis) • Arch of aorta begins & ends. • Trachea ends; primary bronchi begin • Heart T5-9 Body of sternum T7 Inferior angle of scapula • Inferior vena cava passes through T8 diaphragm T9 Xiphisternal junction • Costal slips of diaphragm T9-L3 Costal margin • Esophagus through diaphragm T10 • Aorta through diaphragm • Thoracic duct through diaphragm T12 • Azygos V. through diaphragm • Pyloris of stomach immediately above and to the right of the midline. • Duodenojejunal flexure to the left of midline and immediately below it Tran pyloric plane: Found at the • Pancreas on a line with it L1 midpoint between the jugular • Origin of Superior Mesenteric artery notch and the pubic symphysis • Hilum of kidneys: left is above and right is below. • Celiac a. -

The Neuroanatomy of Female Pelvic Pain
Chapter 2 The Neuroanatomy of Female Pelvic Pain Frank H. Willard and Mark D. Schuenke Introduction The female pelvis is innervated through primary afferent fi bers that course in nerves related to both the somatic and autonomic nervous systems. The somatic pelvis includes the bony pelvis, its ligaments, and its surrounding skeletal muscle of the urogenital and anal triangles, whereas the visceral pelvis includes the endopelvic fascial lining of the levator ani and the organ systems that it surrounds such as the rectum, reproductive organs, and urinary bladder. Uncovering the origin of pelvic pain patterns created by the convergence of these two separate primary afferent fi ber systems – somatic and visceral – on common neuronal circuitry in the sacral and thoracolumbar spinal cord can be a very dif fi cult process. Diagnosing these blended somatovisceral pelvic pain patterns in the female is further complicated by the strong descending signals from the cerebrum and brainstem to the dorsal horn neurons that can signi fi cantly modulate the perception of pain. These descending systems are themselves signi fi cantly in fl uenced by both the physiological (such as hormonal) and psychological (such as emotional) states of the individual further distorting the intensity, quality, and localization of pain from the pelvis. The interpretation of pelvic pain patterns requires a sound knowledge of the innervation of somatic and visceral pelvic structures coupled with an understand- ing of the interactions occurring in the dorsal horn of the lower spinal cord as well as in the brainstem and forebrain. This review will examine the somatic and vis- ceral innervation of the major structures and organ systems in and around the female pelvis. -

35. Lumbar Plexus. Sacral Plexus. Coccygeal Plexus
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic LUMBAR PLEXUS. SACRAL PLEXUS. COCCYGEAL PLEXUS 1. Relevance of the topic Lumbar, sacral and coccygeal plexuses innervate the skin of the abdomen, lower back and lower extremities and all the muscles of the lower limbs. Acquired knowledge is the basis for many fields of practical medicine, such as neurology, surgery and traumatology. 2. Specific objectives After the lesson the student should know and be able to: - describe the sources of the formation of the lumbar plexus; - classify the nerves of the lumbar plexus; - to be able to demonstrate and define the branches of the lumbar plexus; - describe sources of sacral plexus formation; - classify sacral plexus nerves; - be able to demonstrate and identify short and long branches of the sacral plexus; - describe the sources of formation coccygeal plexus; - classify coccygeal plexus nerves; - be able to demonstrate and identify branches of coccygeal plexus; - to explain the innervation of muscles and skin in the areas of the lower back and lower extremity. 3. Basic level of preparation For practical this lesson a student should know and be able: - to know the anatomy of the spine, pelvis, lower extremities; - to analyze and show large and small pelvis, their bones; - to analyze and demonstrate bones and joints of the lower limbs; - to demonstrate muscles of the abdomen, perineum, pelvic girdle and lower limbs; - to know the anatomy (external and internal structure) of the spinal cord; - to know the spinal nerve anatomy. 4. Tasks for independent work during preparation for the classes 4.1. -

1 the Thoracic Wall I
AAA_C01 12/13/05 10:29 Page 8 1 The thoracic wall I Thoracic outlet (inlet) First rib Clavicle Suprasternal notch Manubrium 5 Third rib 1 2 Body of sternum Intercostal 4 space Xiphisternum Scalenus anterior Brachial Cervical Costal cartilage plexus rib Costal margin 3 Subclavian 1 Costochondral joint Floating ribs artery 2 Sternocostal joint Fig.1.3 3 Interchondral joint Bilateral cervical ribs. 4 Xiphisternal joint 5 Manubriosternal joint On the right side the brachial plexus (angle of Louis) is shown arching over the rib and stretching its lowest trunk Fig.1.1 The thoracic cage. The outlet (inlet) of the thorax is outlined Transverse process with facet for rib tubercle Demifacet for head of rib Head Neck Costovertebral T5 joint T6 Facet for Tubercle vertebral body Costotransverse joint Sternocostal joint Shaft 6th Angle rib Costochondral Subcostal groove joint Fig.1.2 Fig.1.4 A typical rib Joints of the thoracic cage 8 The thorax The thoracic wall I AAA_C01 12/13/05 10:29 Page 9 The thoracic cage Costal cartilages The thoracic cage is formed by the sternum and costal cartilages These are bars of hyaline cartilage which connect the upper in front, the vertebral column behind and the ribs and intercostal seven ribs directly to the sternum and the 8th, 9th and 10th ribs spaces laterally. to the cartilage immediately above. It is separated from the abdominal cavity by the diaphragm and communicates superiorly with the root of the neck through Joints of the thoracic cage (Figs 1.1 and 1.4) the thoracic inlet (Fig. -

Quadratus Lumborum Blocks
REGIONAL ANAESTHESIA Tutorial433 Quadratus Lumborum Blocks Ro´ isı´ n Nee†1, John McDonnell2 1Regional Fellow, Galway University Hospital, Galway, Ireland 2Consultant Anaesthetist, Galway University Hospital, Galway, Ireland Edited by: Dr. Su Cheen Ng, University College Hospital London, UK Dr. Gillian Foxall, Consultant Anaesthetist, Royal Surrey County Hospital, Guildford, UK †Corresponding author e-mail: [email protected] Published 29 September 2020 KEY POINTS Quadratus lumborum blocks (QLB) are a variation on transversus abdominis plane (TAP) blocks. Four different approaches to ultrasound-guided QLB have been described. QLB can be used to provide adjuvant analgesia for abdominal, orthopaedic, gynaecological and urological surgery. They can be performed in the lateral or supine position with a wedge under the patient’s hip. The shamrock sign of the psoas, erector spinae and the quadratus lumborum muscles around the transverse process on ultrasound allows identification of the needle insertion point. INTRODUCTION Dr. Rafa Blanco first described quadratus lumborum blocks (QLBs) in 20071 as a ‘‘no pops’’ transversus abdominis plane (TAP) block. It has been proposed as a more consistent method of accomplishing somatic as well as visceral analgesia of the abdomen than the TAP block and may provide an extended sensory blockade between T4 and L1. It can be used as an adjuvant technique for analgesia but does not provide adequate blockade to be used for anaesthesia. The QLB was developed to address the fact that as ultrasound imaging for regional anaesthesia has become more widespread, the tendency has been to move the injection point of the TAP block more anterior on the abdominal wall as compared with the original landmark technique, which is at the Triangle of Petit. -

Sonographic Tracking of Trunk Nerves: Essential for Ultrasound-Guided Pain Management and Research
Journal name: Journal of Pain Research Article Designation: Perspectives Year: 2017 Volume: 10 Journal of Pain Research Dovepress Running head verso: Chang et al Running head recto: Sonographic tracking of trunk nerve open access to scientific and medical research DOI: http://dx.doi.org/10.2147/JPR.S123828 Open Access Full Text Article PERSPECTIVES Sonographic tracking of trunk nerves: essential for ultrasound-guided pain management and research Ke-Vin Chang1,2 Abstract: Delineation of architecture of peripheral nerves can be successfully achieved by Chih-Peng Lin2,3 high-resolution ultrasound (US), which is essential for US-guided pain management. There Chia-Shiang Lin4,5 are numerous musculoskeletal pain syndromes involving the trunk nerves necessitating US for Wei-Ting Wu1 evaluation and guided interventions. The most common peripheral nerve disorders at the trunk Manoj K Karmakar6 region include thoracic outlet syndrome (brachial plexus), scapular winging (long thoracic nerve), interscapular pain (dorsal scapular nerve), and lumbar facet joint syndrome (medial branches Levent Özçakar7 of spinal nerves). Until now, there is no single article systematically summarizing the anatomy, 1 Department of Physical Medicine sonographic pictures, and video demonstration of scanning techniques regarding trunk nerves. and Rehabilitation, National Taiwan University Hospital, Bei-Hu Branch, In this review, the authors have incorporated serial figures of transducer placement, US images, Taipei, Taiwan; 2National Taiwan and videos for scanning the nerves in the trunk region and hope this paper helps physicians University College of Medicine, familiarize themselves with nerve sonoanatomy and further apply this technique for US-guided Taipei, Taiwan; 3Department of Anesthesiology, National Taiwan pain medicine and research. -

Subcostal TAP, Rectus Sheath
Station 4: Traditional Transversus Abdominis Plane (TAP), Subcostal TAP, Rectus Sheath Station Faculty: Traditional TAP: Adam Amundson, MD David Olsen, MD Indications: o Surgeries that involve the lower abdominal segment (below umbilicus) ie: Pfannenstiel incision for cesarean-section. Ultrasound settings and Patient Position o High Frequency linear probe; Low Frequency linear probe if morbidly obese (38-50 mm footprint) o Supine, arms to sides, performed with patient either sedated or under general anesthesia Surface Anatomy landmarks o Rib cage, costal margin o Iliac Crest, pelvic brim o Mid-axillary line Sonoanatomy – o Start by placing the ultrasound probe between the iliac crest and costal margin at the mid-axillary line o Identify the 3 muscular layers (external oblique EO, internal oblique IO, transversus abdominis TA) and the peritoneum o TIPS: EO is generally hyperechoic, IO is the largest, TA is thin, Bowel/Peritoneum may move EO EO IO IO Superior Superior TA TA Bowel Bowel Suggested Injection Technique- TA o In-plane short axis approach, sonographically guide a 21 g 4 inch needle in between the fascial plane of the IO and TA in the posterior corner (see white arrow below). o Inject 20 mL of dilute long acting local anesthetic per side, or 30 mL if unilateral EO EO IO IO Superior Superior TA Bowel Bowel Bowel o TIP: When entering fascial planes between IO and TA the needle tip is often positioned deep and you may need to slowly pull the needle back while giving small aliquots of fluid to help define the spread of the fascial planes.