Drugs Affecting Muscular-Skeletal System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Scottish Medicines Consortium
Scottish Medicines Consortium diclofenac 1% gel patches (Voltarol Gel PatchÒ) No. (199/05) Novartis 9 September 2005 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHS Scotland. The advice is summarised as follows: ADVICE: following a full submission Diclofenac 1% gel patch (Voltarol Gel PatchÒ) is not recommended for use within NHS Scotland for the local symptomatic treatment of pain in epicondylitis and ankle sprain. Diclofenac gel patch provides analgesia similar to that obtained with a topical gel formulation of this drug. However, on a gram per gram basis, patches cost over 40% more than the gel formulation. Overleaf is the detailed advice on this product. Chairman, Scottish Medicines Consortium 1 Diclofenac 1% gel patch (Voltarol Gel Patch®) Licensed indication under review Local symptomatic treatment of pain in epicondylitis and ankle sprain in adults. Dosing information under review Epicondylitis: one application morning and night for up to fourteen days. Ankle sprain: one application per day for up to three days. UK launch date 1 October 2005 Comparator medications Conditions included in the indications of diclofenac 1% gel patch, epicondylitis (tennis elbow) and ankle sprain could be treated topically with gel formulations of other non-steroidal anti- inflammatory drugs (NSAIDs), including diclofenac, ibuprofen, piroxicam, ketoprofen and felbinac or systemically with oral formulations of these drugs -

United States Patent (19) 11 Patent Number: 5,955,504 Wechter Et Al
USOO5955504A United States Patent (19) 11 Patent Number: 5,955,504 Wechter et al. (45) Date of Patent: Sep. 21, 1999 54 COLORECTAL CHEMOPROTECTIVE Marnett, “Aspirin and the Potential Role of Prostaglandins COMPOSITION AND METHOD OF in Colon Cancer, Cancer Research, 1992; 52:5575–89. PREVENTING COLORECTAL CANCER Welberg et al., “Proliferation Rate of Colonic Mucosa in Normal Subjects and Patients with Colonic Neoplasms: A 75 Inventors: William J. Wechter; John D. Refined Immunohistochemical Method.” J. Clin Pathol, McCracken, both of Redlands, Calif. 1990; 43:453-456. Thun et al., “Aspirin Use and Reduced Risk of Fatal Colon 73 Assignee: Loma Linda University Medical Cancer." N Engl J Med 1991; 325:1593-6. Center, Loma Linda, Calif. Peleg, et al., “Aspirin and Nonsteroidal Anti-inflammatory Drug Use and the Risk of Subsequent Colorectal Cancer.” 21 Appl. No.: 08/402,797 Arch Intern Med. 1994, 154:394–399. 22 Filed: Mar 13, 1995 Gridley, et al., “Incidence of Cancer among Patients With Rheumatoid Arthritis J. Natl Cancer Inst 1993 85:307-311. 51) Int. Cl. .......................... A61K 31/19; A61K 31/40; Labayle, et al., “Sulindac Causes Regression Of Rectal A61K 31/42 Polyps. In Familial Adenomatous Polyposis” Gastroenterol 52 U.S. Cl. .......................... 514/568; 514/569; 514/428; ogy 1991 101:635-639. 514/416; 514/375 Rigau, et al., “Effects Of Long-Term Sulindac Therapy On 58 Field of Search ..................................... 514/568, 570, Colonic Polyposis” Annals of Internal Medicine 1991 514/569, 428, 416, 375 11.5:952-954. Giardiello.et al., “Treatment Of Colonic and Rectal 56) References Cited Adenomas With Sulindac In Familial Adenomatous Poly U.S. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Acemetacin.Pdf
Methods and Findings in Experimental and Clinical Pharmacology 2010, 32(2): ???-??? THOMSON REUTERS Copyright © 2010 Prous Science, S.A.U. or its licensors. All rights reserved. CCC: 0379-0355/2010 DOI: 10.1358/mf.2010.32.2.1423883 ORIGINAL ARTICLE ACEMETACIN ANTINOCICEPTIVE MECHANISM IS NOT RELATED TO NO OR K+ CHANNEL PATHWAYS. M. Gil-Flores1, M.I. Ortiz2, G. Castañeda-Hernández1 and A.E. Chávez-Piña1 1Departamento de Farmacología, Centro de Investigación y de Estudios Avanzados del Instituto Politécnico Nacional, México, D.F., México. 2Área Académica de Medicina del Instituto de Ciencias de la Salud, Universidad Autónoma del Estado de Hidalgo, Pachuca, Hidalgo, México SUMMARY Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of acute gout and inflammation. However, its use is limited due to side effects. Acemetacin is a prodrug of indomethacin that exhibits better gastric tolerability in preclinical and clinical tri- als. The aim of this study was to examine if the systemic administration of acemetacin involved the sequential participation of nitric oxide (NO) or K+ channel pathways to confer its antinociceptive effect, as compared to indomethacin. The antinociceptive effect of both drugs was studied with the formalin test. Equimolar doses of acemetacin or indomethacin were administered orally. The intraplantar administra- tion of either L-NAME, glibenclamide, apamin or charybdotoxin plus indomethacin or acemetacin was studied using the formalin test and the anti-inflammatory and antihyperalgesic effects were measured. The antinociceptive effect of acemetacin or indomethacin was not sig- nificantly different when pretreatment with L-NAME, glibenclamide, apamin or charybdotoxin was done. The antihyperalgesic and anti- inflammatory effects were also similar for both indomethacin and acemetacin. -

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -
Download Product Insert (PDF)
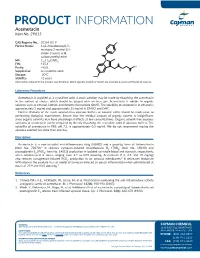
PRODUCT INFORMATION Acemetacin Item No. 29615 CAS Registry No.: 53164-05-9 Cl Formal Name: 1-(4-chlorobenzoyl)-5- methoxy-2-methyl-1H- indole-3-acetic acid, O carboxymethyl ester N MF: C21H18ClNO6 FW: 415.8 O OH Purity: ≥98% O Supplied as: A crystalline solid O Storage: -20°C O Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Acemetacin is supplied as a crystalline solid. A stock solution may be made by dissolving the acemetacin in the solvent of choice, which should be purged with an inert gas. Acemetacin is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of acemetacin in ethanol is approximately 3 mg/ml and approximately 25 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of acemetacin can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of acemetacin in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Acemetacin is a non-steroidal anti-inflammatory drug (NSAID) and a prodrug form of indomethacin 1 (Item No. 70270). It reduces zymosan-induced thromboxane B2 (TXB2; Item No. 19030) and prostaglandin E2 (PGE2; Item No. 14010) production in isolated rat whole blood and stomach, respectively, when administered at doses ranging from 2.7 to 83.8 µmol/kg. -

Diclofenac Topical Patch Gel Solution Monograph
Diclofenac Topical Patch, Gel and Solution National Drug Monograph March 2016 VHA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Action Diclofenac is the only nonsteroidal antiinflammatory drug (NSAID) approved in the U.S. for topical application. The mechanism of diclofenac is believed to be inhibition of prostaglandin synthesis, primarily by nonselectively inhibiting cyclooxygenase. The agents covered in this review are the four diclofenac topical products approved for analgesic purposes: Diclofenac epolamine / hydroxyethylpyrrolidine patch (DEHP) 1.3% approved in January 2007 Diclofenac sodium topical gel 1%, approved in October 2007 Diclofenac sodium topical solution 1.5% with dimethyl sulfoxide (DMSO, 45.5% w/w), approved in November 2009 Diclofenac sodium topical solution 2% with dimethyl sulfoxide (DMSO, 45.5% w/w), approved in January 2014 Indication(s) Under Review in this document (may include off Solution 1.5% Solution 2% label) Patch 1.3% Gel 1% (Drops) (MDP) Topical treatment Relief of the pain of Treatment of signs Treatment of the Also see Table 1 Product Descriptions of acute pain due osteoarthritis of joints and symptoms of pain of below. to minor strains, amenable to topical osteoarthritis of the osteoarthritis of sprains, and treatment, such as the knee(s) the knee(s) contusions knees and those of the hands. -

Lubricants in Pharmaceutical Solid Dosage Forms
Lubricants 2014, 2, 21-43; doi:10.3390/lubricants2010021 OPEN ACCESS lubricants ISSN 2075-4442 www.mdpi.com/journal/lubricants Review Lubricants in Pharmaceutical Solid Dosage Forms Jinjiang Li * and Yongmei Wu Drug Product Science & Technology, Bristol-Myers Squibb Corporation, 1 Squibb Dr., New Brunswick, NJ 08903, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-732-227-6584; Fax: +1-732-227-3784. Received: 18 December 2013; in revised form: 21 January 2014 / Accepted: 24 January 2014 / Published: 25 February 2014 Abstract: Lubrication plays a key role in successful manufacturing of pharmaceutical solid dosage forms; lubricants are essential ingredients in robust formulations to achieve this. Although many failures in pharmaceutical manufacturing operations are caused by issues related to lubrication, in general, lubricants do not gain adequate attention in the development of pharmaceutical formulations. In this paper, the fundamental background on lubrication is introduced, in which the relationships between lubrication and friction/adhesion forces are discussed. Then, the application of lubrication in the development of pharmaceutical products and manufacturing processes is discussed with an emphasis on magnesium stearate. In particular, the effect of its hydration state (anhydrate, monohydrate, dihydrate, and trihydrate) and its powder characteristics on lubrication efficiency, as well as product and process performance is summarized. In addition, the impact of lubrication on the dynamics of compaction/compression processes and on the mechanical properties of compacts/tablets is presented. Furthermore, the online monitoring of magnesium stearate in a blending process is briefly mentioned. Finally, the chemical compatibility of active pharmaceutical ingredient (API) with magnesium stearate and its reactive impurities is reviewed with examples from the literature illustrating the various reaction mechanisms involved. -

United States Patent (19) 11 4,360,518 Rovee Et Al
United States Patent (19) 11 4,360,518 Rovee et al. 45) Nov. 23, 1982 54 TOPICAL ANTI-INFLAMMATORY DRUG Primary Examiner-Stanley J. Friedman THERAPY . 57) ABSTRACT 75) Inventors: David T. Rovee, Bridgewater; John A pharmaceutical composition for topical treatment of R. Marvel; James A. Mezick, both of cutaneous disorders or disruptions characterized by East Brunswick, all of N.J. skin inflammation or hyperproliferative epidermal ac 73) Assignee: Johnson & Johnson, New Brunswick, tivity comprises the combination of a topically active N.J. anti-inflammatory corticosteroid and a non-steroidal 21 Appl. No.: 244,569 anti-inflammatory agent which is an inhibitor of prosta glandin synthetase selected from the group consisting of 22 Filed: Mar. 17, 1981 the hydratropic acid derivatives; acetylsalicylic acid; the pyrazolone derivatives; the fenamic acid deriva Related U.S. Application Data tives; the aroyl-substituted pyrroles and the substituted 60) Division of Ser. No. 64,311, Aug. 6, 1979, abandoned, arylacetohydroxamic acids in a pharmaceutically ac which is a division of Ser. No. 788,453, Apr. 20, 1977, ceptable topical vehicle. Treatment of above cutaneous Pat. No. 4,185, 100, which is a continuation-in-part of disorders may also be effected by concurrent therapy Ser. No. 685,942, May 13, 1976, abandoned. using separate applications of corticosteroid and non 51) Int. Cl. ...................... A61K 31/19; A61K 31/56 steroid. (52) U.S. Cl. ..................................... 424/240; 424/317 58) Field of Search ................................ 424/317, 240 18 Claims, No Drawings 4,360,518 1 2 Ziboh, V. A. and Snyder, D. S. 1974 Naturally occur TOPICAL ANTI-NFLAMMATORY ORUG ring and synthetic inhibitors of prostaglandin synthetase THERAPY of the skin. -

Fatal Hepatitis Associated with Diclofenac
Gut: first published as 10.1136/gut.27.11.1390 on 1 November 1986. Downloaded from Gut, 1986, 27, 1390-1393 Case reports Fatal hepatitis associated with diclofenac E G BREEN, J McNICHOLL, E COSGROVE, J MCCABE, AND F M STEVENS From the Department of Medicine, Regional Hospital, Galway, Eire SUMMARY Non-steroidal anti-inflammatory agents (NSAIDS) are a well recognised cause of hepatotoxicity. Diclofenac, a relatively new NSAID, was first introduced into the UK in 1979. Five cases of hepatitis have recently been reported, principally in the French literature. -5 We report the first fulminant case of hepatitis in the English literature in a patient taking diclofenac and indomethacin. Diclofenac is a member of the arylalkanoic group of 100 mg per day for five weeks. Ferrous sulphate one NSAIDS (Fig. 1). Three other agents in this group tablet daily was added on 16 May. The patient was have been shown to be significantly hepatotoxic. admitted to hospital on 26 June. A week before this Ibufenac was withdrawn from circulation because of he had felt unwell with anorexia, nausea, abdominal the frequent rise in transaminases,6 7 the use of discomfort, and dark urine. On admission he was benoxaprofen was stopped in Britain after 10 icteric, the liver edge was palpable 4 cm below the patients died with hepatitis8 9 and more recently a costal margin and there were no signs of chronic fatal case of hepatitis due to pirprofen has been liver disease. Ultrasound showed early ascites with reported."' Early reports about diclofenac showed no obstruction of the biliary tract.