(SOP) for Responding Toterrorist Attacks Using CHEMICAL WEAPONS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brief Summary
B R I EF SUMMARY This Project is for Common Bio- Medical Waste Treatment, Storage & Disposal Facility is proposed to be established by Wise Ecocare & Farmtech Pvt. Ltd at Plot no. E 35, Khamgaon MIDC, Dist. Buldhana. A Common Bio-medical Waste Treatment and Disposal Facility (CBWTF) is a set up where biomedical waste generated from member health care facilities is imparted necessary treatment to reduce adverse effects that this waste may pose on human health and environment. The present proposal is to obtain Environmental Clearance for CBWTF which is spread over an area of 3629 Sq. mtr at plot in Khamgaon MIDC. The treated recyclable waste will finally be sent for disposal in a secured landfill or for recycling. Brief Project Summary Sr. No Particulars Details 1 Name of Company Wise Ecocare &Farmtech Pvt. Ltd. 2 Products Not Applicable as facility is CBMWTSDF 3 Location Plot No. E-35, Khamgaon MIDC, Village Sutala(BK), Taluka Khamgaon, District: Buldhana 4 Name of the project Proposed Common Bio- Medical Waste Treatment, Storage & Disposal Facility (CBMWTSDF) 5 Total land area of the plot 3629 Sq. mtr. 6 Fresh Water requirement Proposed fresh water requirement = 18 cmd from MIDC 7 Power Power Requirement -100 KW Source: MSEDCL 8 Waste water quantity DomesticSewage: 1.90cmd trade Effluent: 9.60 cmd 9 Project cost Estimate ~ Rs2.38Crores The proposed project is establishing a CBMWTSDF, which is a part of the Common Hazardous Waste Treatment, Storage and Disposal facilities (TSDFs) and falls under Category B, schedule 7 (da) as per the EIA notification 14th Sep,2006 and its subsequent amendments dated 17thApril, 2015, under Bio- Medical Waste Treatment Facility. -

District Taluka Center Name Contact Person Address Phone No Mobile No
District Taluka Center Name Contact Person Address Phone No Mobile No Mhosba Gate , Karjat Tal Karjat Dist AHMEDNAGAR KARJAT Vijay Computer Education Satish Sapkal 9421557122 9421557122 Ahmednagar 7285, URBAN BANK ROAD, AHMEDNAGAR NAGAR Anukul Computers Sunita Londhe 0241-2341070 9970415929 AHMEDNAGAR 414 001. Satyam Computer Behind Idea Offcie Miri AHMEDNAGAR SHEVGAON Satyam Computers Sandeep Jadhav 9881081075 9270967055 Road (College Road) Shevgaon Behind Khedkar Hospital, Pathardi AHMEDNAGAR PATHARDI Dot com computers Kishor Karad 02428-221101 9850351356 Pincode 414102 Gayatri computer OPP.SBI ,PARNER-SUPA ROAD,AT/POST- 02488-221177 AHMEDNAGAR PARNER Indrajit Deshmukh 9404042045 institute PARNER,TAL-PARNER, DIST-AHMEDNAGR /221277/9922007702 Shop no.8, Orange corner, college road AHMEDNAGAR SANGAMNER Dhananjay computer Swapnil Waghchaure Sangamner, Dist- 02425-220704 9850528920 Ahmednagar. Pin- 422605 Near S.T. Stand,4,First Floor Nagarpalika Shopping Center,New Nagar Road, 02425-226981/82 AHMEDNAGAR SANGAMNER Shubham Computers Yogesh Bhagwat 9822069547 Sangamner, Tal. Sangamner, Dist /7588025925 Ahmednagar Opposite OLD Nagarpalika AHMEDNAGAR KOPARGAON Cybernet Systems Shrikant Joshi 02423-222366 / 223566 9763715766 Building,Kopargaon – 423601 Near Bus Stand, Behind Hotel Prashant, AHMEDNAGAR AKOLE Media Infotech Sudhir Fargade 02424-222200 7387112323 Akole, Tal Akole Dist Ahmadnagar K V Road ,Near Anupam photo studio W 02422-226933 / AHMEDNAGAR SHRIRAMPUR Manik Computers Sachin SONI 9763715750 NO 6 ,Shrirampur 9850031828 HI-TECH Computer -

Sr No Age Sex Address
RTPCR SR NO AGE SEX ADDRESS Manjalkhed Kasaba 1 35 M Chandur Rly 2 70 F Ram Nagr Chandur Rly 3 60 F Indira Nagar Chandur Rly 4 36 M Athwadi Bazar Chandur Rly 5 25 M Baslapur Chandur Rly 6 17 M Kawatha Kadu Chandur Rly 7 53 M Shivaji Nagar Chandur Rly 8 50 F Songaon Chandur Rly 9 30 m Songaon Chandur Rly Shirajgaon Korde Chandur 10 57 M Rly 11 70 M Amduri Chandur Rly 12 70 F Palaskhed Chandur Rly 13 60 M Bori Chandur Rly Mahalaxmi Nagar Chandur 14 44 M Rly Juna Motor Stand Chandur 15 32 M Rly 16 33 F Sardar Chowk Chandur Rly 17 42 F Shivaji Nagar Chandur Rly 18 31 M Kazipura Chandur Rly 19 36 F Baggi Chandur Rly 20 25 F Dhanraj Nagar Chandur Rly 21 65 F Chandurwadi Chandur Rly Manjalkhed Kasaba 22 50 F Chandur Rly Manjalkhed Kasaba 23 60 M Chandur Rly 24 12 F Chandurwadi Chandur Rly 25 9 M Chandurwadi Chandur Rly 26 27 M Ravi Nagar Morshi 27 55 M Gedampura Morshi 28 42 F Gandhi Chowk Morshi 29 25 F Chikhal Sawangi Morshi 30 54 M Manimpur Morshi 31 62 M Talni Morshi 32 38 M Nerpingai Morshi 33 34 F Nerpingai Morshi 34 59 M Naya Wathoda Morshi 35 46 M Ambada Morshi 36 54 F Simbhora Chowk Morshi 37 66 M Dapori Morshi 38 42 M Dapori Morshi 39 40 M Chikhal Sawangi Morshi 40 55 F Chikhal Sawangi Morshi 41 35 M Om Nagar Morshi 42 30 M Ashtagaon Morshi 43 28 M Ambada Morshi 44 26 M Hiwarkhed Morshi 45 48 M Dapori Morshi 46 35 F Kshams Colony Morshi 47 20 F Kshams Colony Morshi 48 19 M Chikhal Sawangi Morshi 49 30 M Durgwada Morshi 50 75 M Ramjibaba Nagar Morshi 51 28 M Udkhed Morshi 52 50 F Udkhed Morshi 53 24 F Udkhed Morshi 54 50 M Hiwarkhed -

Reg. No Name in Full Residential Address Gender Contact No. Email Id Remarks 9421864344 022 25401313 / 9869262391 Bhaveshwarikar
Reg. No Name in Full Residential Address Gender Contact No. Email id Remarks 10001 SALPHALE VITTHAL AT POST UMARI (MOTHI) TAL.DIST- Male DEFAULTER SHANKARRAO AKOLA NAME REMOVED 444302 AKOLA MAHARASHTRA 10002 JAGGI RAMANJIT KAUR J.S.JAGGI, GOVIND NAGAR, Male DEFAULTER JASWANT SINGH RAJAPETH, NAME REMOVED AMRAVATI MAHARASHTRA 10003 BAVISKAR DILIP VITHALRAO PLOT NO.2-B, SHIVNAGAR, Male DEFAULTER NR.SHARDA CHOWK, BVS STOP, NAME REMOVED SANGAM TALKIES, NAGPUR MAHARASHTRA 10004 SOMANI VINODKUMAR MAIN ROAD, MANWATH Male 9421864344 RENEWAL UP TO 2018 GOPIKISHAN 431505 PARBHANI Maharashtra 10005 KARMALKAR BHAVESHVARI 11, BHARAT SADAN, 2 ND FLOOR, Female 022 25401313 / bhaveshwarikarmalka@gma NOT RENEW RAVINDRA S.V.ROAD, NAUPADA, THANE 9869262391 il.com (WEST) 400602 THANE Maharashtra 10006 NIRMALKAR DEVENDRA AT- MAREGAON, PO / TA- Male 9423652964 RENEWAL UP TO 2018 VIRUPAKSH MAREGAON, 445303 YAVATMAL Maharashtra 10007 PATIL PREMCHANDRA PATIPURA, WARD NO.18, Male DEFAULTER BHALCHANDRA NAME REMOVED 445001 YAVATMAL MAHARASHTRA 10008 KHAN ALIMKHAN SUJATKHAN AT-PO- LADKHED TA- DARWHA Male 9763175228 NOT RENEW 445208 YAVATMAL Maharashtra 10009 DHANGAWHAL PLINTH HOUSE, 4/A, DHARTI Male 9422288171 RENEWAL UP TO 05/06/2018 SUBHASHKUMAR KHANDU COLONY, NR.G.T.P.STOP, DEOPUR AGRA RD. 424005 DHULE Maharashtra 10010 PATIL SURENDRANATH A/P - PALE KHO. TAL - KALWAN Male 02592 248013 / NOT RENEW DHARMARAJ 9423481207 NASIK Maharashtra 10011 DHANGE PARVEZ ABBAS GREEN ACE RESIDENCY, FLT NO Male 9890207717 RENEWAL UP TO 05/06/2018 402, PLOT NO 73/3, 74/3 SEC- 27, SEAWOODS, -

A Detailed District Survey Report of Amravati
DSR- AMRAVATI A Detailed District Survey Report of Amravati Collector office; Amravati. 1 DSR- AMRAVATI Index Preface 1. Introduction 2. Overview of mining activity in the district 3. List of the Mining Leases in the district 4. Details of Royalty or Revenue received in last three years 5. Details of Production of sand or minor mineral in last three years 6. Deposition of sediments in the rivers of the district 7. General profile of the district 8. Land utilization pattern in the district 9. Physiography of the district 10. Rainfall 11. Geology and Mineral wealth 12. Major and Minor Rivers of the District 13. General recommendation 2 DSR- AMRAVATI Preface In Compliance to the Notification Issued by the Ministry Of Environment, Forest and Climate change Dated 15.01.2016, the preparation of District survey report of River bed mining and other minor minerals is in accordance appendix 10 of the notification. It is also mentioned here that the procedure of preparation of District Survey Report is as per notification guidelines. Every efforts have been made to cover sand mining locations, area & overview of mining activity in the district with all its relevant features pertaining to geology & mineral wealth in replenish able and non- replenish able areas of rivers, stream and other sand sources. This report will be a model and guiding document which is a compendium of available mineral resources, geographical set up, environmental and ecological set up of the district and is based on data of various departments, published reports, and websites. The data may vary due to floods, heavy rains and other natural calamities. -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -
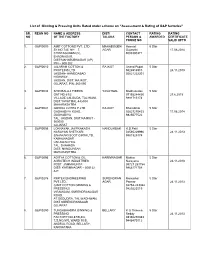
List of Ginning & Pressing Units Rated Under Scheme on “Assessment
List of Ginning & Pressing Units Rated under scheme on “Assessment & Rating of G&P factories” SR. REGN NO NAME & ADDRESS DIST/ CONTACT RATING RATING NO OF THE FACTORY TALUKA PERSON & AWARDED CERTIFICATE PHONE NO VALID UPTO 1. G&P/0009 AMIT COTTONS PVT. LTD MAHABOOBN Hemant 5 Star SY.NO.745, NH – 7, AGAR Gujarathi 17.08.2014 CHINTAGUDEM (V), 9000300371 EHADNAGAR, DIST:MAHABUBNAGAR (AP) PIN – 509 202 2. G&P/0010 JALARAM COTTON & RAJKOT Anand Popat 5 Star PROTEINS LTD 9426914910 24.11.2013 JASDAN- AHMEDABAD 02821222201 HIGHWAY, JASDAN, DIST: RAJKOT, GUJARAT, PIN: 360 050 3. G&P/0034 SHRI BALAJI FIBERS YAVATMAL Madhusudan 5 Star GAT NO:61/2 07153244430 27.6.2015 VILLAGE LALGUDA, TAL:WANI, 9881715174 DIST:YAVATMAL-445304 MAHARASHTRA 4. G&P/0041 GIRIRAJ COTEX P.LTD RAJKOT Bharatbhai 5 Star GADHADIYA ROAD, 02827270453 17.08.2014 GADHADIYA 9825077522 TAL: JASDAN, DIST;RAJKOT - 360050 GUJARAT 5. G&P/0056 LOKNAYAK JAYPRAKASH NANDURBAR R.D.Patil 5 Star NARAYAN SHETKARI 02565229996 24.11.2013 SAHAKARI SOOT GIRNI LTD, 9881925174 KAMALNAGAR UNTAWAD HOL TAL. SHAHADA DIST: NANDURBAR MAHARASHTRA 6. G&P/0096 ADITYA COTTON & OIL KARIMNAGAR Mukka 5 Star AGROTECH INDUSTRIES Narayana 24.11.2013 POST: JAMMIKUNTA 08727 253754 DIST: KARIMNAGAR – 505122 9866171754 A.P. 7. G&P/027 6 RIMTEX ENGINEERING SURENDRAN Manubhai 5 Star PVT.LTD., AGAR Parmar 24.11.2013 (UNIT COTTON GINNING & 02752-243322 PRESSING) 9825223519 VIRAMGAM, SURENDRANAGAR ROAD, AT.DEDUDRA, TAL.WADHWAN, DIST SURENDRANAGAR GUJARAT 8. G&P/0290 TUNGABHADRA GINNING & BELLARY K G Thimma 5 Star PRESSING Reddy 24.11.2013 FACTORY,NO.87/B,3/4, 08392250383 T.S.NO.970, WARD 10 B, 9448470112 ANDRAL ROAD, BELLARY, KARNATAKA 9. -

The Maharashtra State Co-Operative Bank Ltd., Mumbai
Akot SSG Ltd.-Tender The Authorised Officer Of The Maharashtra State Co-operative Bank Ltd., Mumbai (Incorporating TheVidarbha Co-Op Bank Ltd.) Sir Vithaldas Thackersey Memorial Bldg., 9, Maharashtra Chamber of Commerce Lane, Fort, Mumbai – 400 001., Maharashtra Reference No. MSCB/DIRR/SEC- 46/380/2020-21 dated 12/01/2021 For Sale of Assets Of AKOT TALUKA SAHAKARI SOOT GIRNI LTD., VILLAGE- JOGBAN, AKOT- HIWARKHED ROAD, TAL. AKOT, DIST. AKOLA, MAHARASHTRA Under Securitisation and Reconstruction of Financial Assets and Enforcement of Security Interest Act, 2002 And Security Interest (Enforcement) Rules, 2002 1 | P a g e Akot SSG Ltd.-Tender TABLE OF CONTENTS I. COPY OF THE NOTICE OF SALE ……………………………………………………………………………………….3 II. COPY OF POSSESSION NOTICE………………………………………………………………………………………..5 III. INTRODUCTION ……………………………………………………………………………………………………………..6 IV. DETAILS OF SECURED ASSETS- IMMOVABLE ASSETS/PROPERTIES…………………………………...7 V. DETAILS OF SECURED ASSETS- MOVABLE ASSETS AND MACHINERY…………………………………9 VI. OUTSTANDING DUES OF THE SECURED CREDITIORS….…………………………..……………………….12 VII. TERMS AND CONDITIONS………………………….……………………………………………………………………13 VIII. BRIEF DETAILS OF BID/OFFER DOCUMENT.……………………………………………………………….......18 IX. FORM OF BID/OFFER………………………………………………………………………………………………………19 X. FORM OF APPENDIX TO THE BID/OFFER (DECLARATION BY THE BIDDER)……………………….20 XI. FORMAT FOR SUBMISSION OF PROFILE OF THE BIDDER/COMPANY/FIRM/PARTY………….22 XII. DEED OF UNDERTAKING CUM INDEMNITY…………..………………………………………………………….24 2 | P a g e Akot SSG Ltd.-Tender I. Copy of the Notice for Sale THE MAHARASHTRA STATE CO-OPERATIVE BANK LTD., MUMBAI (Incorporating The Vidarbha Co-Op Bank Ltd.) (Schedule Bank) Head Office: 2nd Floor, Sir Vithaldas Thackersey Memorial Bldg., 9, Maharashtra Chamber of Commerce Lane, Fort, Mumbai – 400 001, Post Box No. 472 Tel Nos. 91-022-22822217/22876020. -

Power Evacuation Capacity Available in MSETCL Substations As on 17.02.2020
Power evacuation capacity available in MSETCL substations as on 17.02.2020 Note: The availability of power evacuation capacity and issuance of grid connectivity will be governed by following conditions: a) The capacity mentioned for substations is indicative only and does not guarantee the grid connectivity feasibility at that substation. b) Grid connectivity feasibility will be confirmed after application by developer for grid connectivity and after technical feasibility & detailed Load Flow Study. c) The availability of required feeder bays at substation, space available inside switchyard, issues of line corridor, ROW, building control line etc. needs to to be checked separately at the time of joint survey for technical feasibility. d) The data provided is given as on date which may change in future due to changes in grid structure and change in power flow dynamics at that time. e) The grid connectivity applications will be processed as per prevailing GOM RE Policy & methodology formulated under policy and Grid Connectivity Procedure under MERC Open Access Regulation-2016. Sr. Cluster Source Name of the Substation Dist. Latitude Longitude No. Capacity 1 132/33/11kV Gondia Gondia 21.47807 80.13654 220/132/33kV 2 132/33kV Amgaon Gondia 21.37273 80.39122 80MW Kawalewada 3 132/33/11kV Madgi Bhandara 21.33576 79.779193 4 132/33kV Sakoli Bhandara 21.090255 80.000614 5 132/33kV Kardha Bhandara 21.1388 79.673 6 132/33kV Gose khurd Bhandara 20.874845 79.621687 7220/132/33/11kV 132/33kV Asgaon Bhandara 20.803388 79.725639 80MW 8Bhandara 132/33kV -

Societies / Individuals (F)
Societies / Individuals (F) SR. MEMB NAME ADDRESS Representative Name Age Representative Address Second Representative NO. ER Gender DEFAULTER (Y/N) REMARK Name NO. 809 906 SHETKARI SAH. KHARDI VIKRI & TAL. - PATUR, DIST. AKOLA, PIN Shri Rathod Madhukar At Post Malrajura, Tal Patur, Dist M N PROCESSING STY LTD, PATUR. 444501 Hiramal Akola 810 655 HIWARKHED KRISHI PRAKRIYA AT/POST - HIWARKHED Nomination Not Recived SAH. SANSTHA HIWARKHED (RUPRAO), TAL. AKOT, DIST. N AKOLA, PIN 444001 811 658 THE COOPERATIVE GINNING & MANA(C.R.), TAL. - MURTIZAPUR, Nomination Not Recived 54 PRESSING FACTORY LTD. MANA DIST. - AKOLA, PIN - 444107 N 812 872 MURTIZAPUR CO-OP. GINNING & AT POST - MURTIZAPUR, TAL. - Nomination Not Recived PRESSING FACTORY LTD. MURTIZAPUR, DIST. AKOLA, PIN N 444107 813 907 NARNALA PARISAR BIJ UTPADAK A.P.M.C. YARD, POPAT KHED Shri Hingakar Rameshrao At.Post Kalvadi, Tal.& Dist.Akola VA PRAKRIYA SANSTHA LTD. ROAD, AKOLA, TAL. - AKOLA, Shriramji M N AKOLA DIST. - AKOLA, PIN - 444001 814 2304 TELHARA TALUKA SAHAKARI AT POST - TELHARA, TAL. - AKOT, Shri Tapre Navinchandra Talegaon Bajar Telara, Dist GINNING & PRESSING STY. LTD. DIST. AKOLA, PIN 444108 Kashinath M Akola N TELHARA 815 2308 AKOLA GINNING & PRESSING CO- NEAR MAHATMA MILLS, AT POST - Shri Dhotre Sirish Tapadiya Nagar Akola. OP FACTORY LTD. AKOLA, AKOLA, TAL.-AKOLA, PIN 444001 Vasantrao M N 816 2319 GRAM VIKAS SAH. GINNING WA AT POST. - URAL, TAL. - Shri Kale Prakash Gulabrao Shankund, Tal Dist Akola PRESSING FACTORY MARYADIT BALAPUR, DIST. - AKOLA, PIN M N AKOLA 444001 817 2424 AMARAVATI ZILLA MAHILA VIKAS MHADA FLAT, H/A-2, TOPE Smt Varade Varsha Sunil Rathi Nagar, Amravati SAH. -

Sr No Age Sex Address
RTPCR SR NO AGE SEX ADDRESS MAHENDRA COLONY 1 13 F AMT DEVARANKAR NAGAR 2 30 M AMT 3 68 F PRASAD COLONY AMT 4 33 F POTE TOWNSHIP AMT AT ANGOLA TAKDI 5 54 F JAHAGIR TQ D AMT AMBIKA NAGAR 6 35 M TAPOWAN AMT 7 18 M ANSAR NAGAR AMT Shirajgaon Korde Chandur 8 35 M Rly Sanjyot Colony Chandur 9 40 M Rly Sanjyot Colony Chandur 10 35 F Rly 11 73 M Satefal Chandur Rly 12 37 M Satefal Chandur Rly 13 74 F Ghuikhed Chandur Rly 14 47 M Satefal Chandur Rly 15 58 M Mandwa Chandur Rly 16 55 F Sadanand colony Daryapur 17 63 M YEODA DARYAPUR 18 28 m Viddut nagar amt 19 50 m Walgao amt Surkasha colony Tapowan 20 32 m get amt At po. Karala ta. Chandur ril 21 19 m amt 22 34 F Sultanpura Morshi 23 30 M Dongar Yawali Morshi 24 26 M Hiwarkhed Morshi 25 55 m warud 26 24 F warud 27 43 m KARAJRAON 28 55 m AMDAPUR 29 35 m JARUD 30 24 F SHAHAPUR 31 28 m KURALI 32 37 m warud 33 5 F warud 34 65 m warud 35 35 m warud 36 26 m JARUD 37 60 F BENODA 38 29 F BENODA 39 28 m BENODA 40 24 m BENODA 41 44 m WARUD 42 40 M AMRAVATI 43 30 M Hiwarkhed Morshi 44 45 M Hiwarkhed Morshi 45 35 M Hiwarkhed Morshi 46 52 M Hiwarkhed Morshi 47 71 M ADGAON KHADE 48 60 F ANJANGAON SURJI 49 22 m bhatkuli 50 15 m dadhi 51 50 M Songaon Chandur Rly 52 58 M Indira Nagar Chandur Rly 53 50 F Songaon Chandur Rly 54 39 F Ghuikhed Chandur Rly 55 49 M Ghuikhed Chandur Rly 56 38 M NAVEEN NAGAR AMT 57 46 M CHAPRASHI PURA AMT 58 44 M RAMPURI CAMP AMT MAHENDRA COLONY 59 34 M AMT 60 64 F DASTUR NAGAR AMT NR GADEGADESHWAR 61 37 M MANDIR AMT RAHATGAON 62 52 F GURUKRUPA COLONY AMT AT MALKHED TQ 63 23 M CHANDUR -
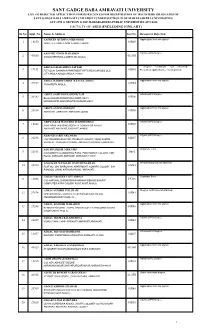
Rejected-Application-List.Pdf
SANT GADGE BABA AMRAVATI UNIVERSITY LIST OF REJECTED APPLICATION FORMS RECEIVED FOR REGISTRATION OF REGISTERD GRADUATES OF SANT GADGE BABA AMRAVATI UNIVERSITYUNDER SECTION 99 OF MAHARASHTRA UNIVERSITIES ACT,1994 & SECTION 131OF MAHARASHTRA PUBLIC UNIVERSITIES ACT,2016 FACULTY OF ARTS (INCLUDING FINE ART) Sr.No. Appl. No. Name & Address Lot No. Reason for Rejection AAFREEN QUDSIYA MEHMOOD Application form not signed 1 18850 01R09 AKOT FILE,AKOLA,AKOLA,AKOLA.444001 AAHOTE VINOD MAHADEO Attached PG Degree 2 43160 01OFR SHAMSHERPURA,JAMBHA BK,AKOLA. ABDUL GALIB ABDUL SATTAR Degree certificate not attached, 3 19151 01R01 FLT NO.A1 SAHARA APPARTMENT RPTS RD.AGAR BES OLD Prescribed application fee not deposited CITY AKOLA,AKOLA,AKOLA.444001 ABDUL RASHID ABDUL RAZZAK ABDUL Application form not signed 4 29853 01R44 TAJNAPETH AKOLA,,. ABDUL SAIFUDDNZAHEER TAJI Attached PG Degree 5 20389 01R06 BILAL NAGAR DIWANPURA WARD NO 03 MANGRULPIR,MANGRULPIR,WASHIM.44443 ABDUL SALIM SIDDIQUI Application form not signed 6 20514 01R06 AMRAVATI ,AMRAVATI,AMRAVATI.444604 ABHYANKAR WASUDEO SUKHDEORAO Attached PG Degree 7 15382 01R09 PANCHSHIL HOUSING SOCIETY CONGRESS NAGAR AMRAVATI,AMRAVATI,AMRAVATI.444606 ADASAD AARTI ARUNRAO Attached PG Degree 8 21238 01R07 C/O VIRENDRA BHOYAR, PRABHAT COLONY, NEAR ASMITA VIDYALAY, SHILANGAN ROAD, AMRAVATI,AMRAVATI,AMRAVATI. ADE SHUBHAM NIRANJAN Duplicate Form 9 11551 Du01 C/O MANISH GAJANANRAO PATIL, PANCHAWATI COLONY, VMV ROAD, AMRAVATI,AMRAVATI,AMRAVATI.444604 ADGOKAR MANGESH RAMESHWARRAO Residential proof not attached 10 33230 01R43 FLAT NO. 204, SHIROMANI APARTMENT, KONARK COLONY, B/H RANGOLI LAWN, KATHORA ROAD, AMRAVATI ,,. ADHAO ARCHANA GULABRAO Duplicate Form 11 18808 DU03 C/O HARSHAL SHRIKRISHNA MANKAR BEHIND BHARAT COMPUTER ASRA COLONY AKOT,AKOT,AKOLA.