Developing Synthetic Peptide-Based Inhibitors of Human Growth Hormone Receptor
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
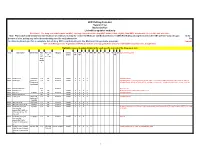
Drug Code List
HCPCS/Drug Code List Version 13.2 Revised 6/1/21 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Go to data.medicaid.gov for a complete list of drug NDCs participating in the Medicaid drug rebate program. Consult with each Managed Care Organization (MCO) about their coverage guidelines and prior authroization requirements, if applicable. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI ID DC Special Instructions req. of Limits OP OP TF for measure drug rebate ? 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmacological Management of Acromegaly: a Current Perspective
Neurosurg Focus 29 (4):E14, 2010 Pharmacological management of acromegaly: a current perspective SUNIL MANJILA , M.D.,1 Osmo N D C. WU, B.A.,1 FAH D R. KHAN , M.D., M.S.E.,1 ME H ree N M. KHAN , M.D.,2 BAHA M. AR A F AH , M.D.,2 AN D WA rre N R. SE L M AN , M.D.1 1Department of Neurological Surgery, The Neurological Institute, and 2Division of Clinical and Molecular Endocrinology, University Hospitals Case Medical Center, Cleveland, Ohio Acromegaly is a chronic disorder of enhanced growth hormone (GH) secretion and elevated insulin-like growth factor–I (IGF-I) levels, the most frequent cause of which is a pituitary adenoma. Persistently elevated GH and IGF-I levels lead to substantial morbidity and mortality. Treatment goals include complete removal of the tumor causing the disease, symptomatic relief, reduction of multisystem complications, and control of local mass effect. While trans- sphenoidal tumor resection is considered first-line treatment of patients in whom a surgical cure can be expected, pharmacological therapy is playing an increased role in the armamentarium against acromegaly in patients unsuitable for or refusing surgery, after failure of surgical treatment (inadequate resection, cavernous sinus invasion, or transcap- sular intraarachnoid invasion), or in select cases as primary treatment. Three broad drug classes are available for the treatment of acromegaly: somatostatin analogs, dopamine agonists, and GH receptor antagonists. Somatostatin analogs are considered as the first-line pharmacological treatment of acromegaly, although effica- cy varies among the different formulations. Octreotide long-acting release (LAR) appears to be more efficacious than lanreotide sustained release (SR). -

To Download a List of Prescription Drugs Requiring Prior Authorization
Essential Health Benefits Standard Specialty PA and QL List July 2016 The following products require prior authorization. In addition, there may be quantity limits for these drugs, which is notated below. Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, HIV SELZENTRY (maraviroc) None Cardiology Antilipemic JUXTAPID (lomitapide) 1 tab/day PRALUENT (alirocumab) 2 syringes/28 days REPATHA (evolocumab) 3 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 3 tabs/day FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) Soln None REVATIO (sildenafil) Tabs 3 tabs/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day UPTRAVI (selexipag) 2 tabs/day UPTRAVI (selexipag) Pack 2 packs/year VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Central Nervous System Anticonvulsants SABRIL (vigabatrin) pack None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) 20 cartridges/30 days Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Electrolyte & Renal Agents Diuretics KEVEYIS (dichlorphenamide) 4 tabs/day Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg -

Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future
International Journal of Molecular Sciences Review Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future Anna Kathrin Stueven 1, Antonin Kayser 1, Christoph Wetz 2, Holger Amthauer 2, Alexander Wree 1, Frank Tacke 1, Bertram Wiedenmann 1, Christoph Roderburg 1,* and Henning Jann 1 1 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Hepatology and Gastroenterology, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (A.K.S.); [email protected] (A.K.); [email protected] (A.W.); [email protected] (F.T.); [email protected] (B.W.); [email protected] (H.J.) 2 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Nuclear Medicine, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (C.W.); [email protected] (H.A.) * Correspondence: [email protected]; Tel.: +49-30-450-553022 Received: 3 May 2019; Accepted: 19 June 2019; Published: 22 June 2019 Abstract: In recent decades, the incidence of neuroendocrine tumors (NETs) has steadily increased. Due to the slow-growing nature of these tumors and the lack of early symptoms, most cases are diagnosed at advanced stages, when curative treatment options are no longer available. Prognosis and survival of patients with NETs are determined by the location of the primary lesion, biochemical functional status, differentiation, initial staging, and response to treatment. Somatostatin analogue (SSA) therapy has been a mainstay of antisecretory therapy in functioning neuroendocrine tumors, which cause various clinical symptoms depending on hormonal hypersecretion. Beyond symptomatic management, recent research demonstrates that SSAs exert antiproliferative effects and inhibit tumor growth via the somatostatin receptor 2 (SSTR2). -

Regulatory Mechanisms of Somatostatin Expression
International Journal of Molecular Sciences Review Regulatory Mechanisms of Somatostatin Expression Emmanuel Ampofo * , Lisa Nalbach, Michael D. Menger and Matthias W. Laschke Institute for Clinical & Experimental Surgery, Saarland University, 66421 Homburg/Saar, Germany; [email protected] (L.N.); [email protected] (M.D.M.); [email protected] (M.W.L.) * Correspondence: [email protected]; Tel.: +49-6841-162-6561; Fax: +49-6841-162-6553 Received: 25 May 2020; Accepted: 9 June 2020; Published: 11 June 2020 Abstract: Somatostatin is a peptide hormone, which most commonly is produced by endocrine cells and the central nervous system. In mammals, somatostatin originates from pre-prosomatostatin and is processed to a shorter form, i.e., somatostatin-14, and a longer form, i.e., somatostatin-28. The two peptides repress growth hormone secretion and are involved in the regulation of glucagon and insulin synthesis in the pancreas. In recent years, the processing and secretion of somatostatin have been studied intensively. However, little attention has been paid to the regulatory mechanisms that control its expression. This review provides an up-to-date overview of these mechanisms. In particular, it focuses on the role of enhancers and silencers within the promoter region as well as on the binding of modulatory transcription factors to these elements. Moreover, it addresses extracellular factors, which trigger key signaling pathways, leading to an enhanced somatostatin expression in health and disease. Keywords: somatostatin; pre-prosomatostatin; δ-cells; central nervous system (CNS); gut; hypothalamus; cAMP resonse element (CRE); pancreas/duodenum homeobox protein (PDX)1; paired box protein (PAX)6; growth hormone (GH); brain-derived neurotrophic factor (BDNF); glutamateric system; pancreas 1. -

Hypothalamic-Pituitary Axes
Hypothalamic-Pituitary Axes Hypothalamic Factors Releasing/Inhibiting Pituitary Anterior Pituitary Hormones Circulating ACTH PRL GH Hormones February 11, 2008 LH FSH TSH Posterior Target Pituitary Gland and Hormones Tissue Effects ADH, oxytocin The GH/IGF-I Axis Growth Hormone Somatostatin GHRH Hypothalamus • Synthesized in the anterior lobe of the pituitary gland in somatotroph cells PITUITARY • ~75% of GH in the pituitary and in circulation is Ghrelin 191 amino acid single chain peptide, 2 intra-molecular disulfide bonds GH Weight; 22kD • Amount of GH secreted: IGF-I Women: 500 µg/m2/day Synthesis IGF- I Men: 350 µg/m2/day LIVER Local IGF-I Synthesis CIRCULATION GH Secretion: Primarily Pulsatile Pattern of GH Secretion Regulation by two hypothalamic in a Healthy Adult hormones 25 Sleep 20 Growth - SMS Hormone 15 Somatostatin Releasing GHRH + GH (µg/L) Hormone Inhibitory of 10 Stimulatory of GH Secretion GH Secretion 05 0 GHRH induces GH Somatostatin: Decreases to allow 0900 2100 0900 synthesis and secretion Clocktime GH secretory in somatotrophs Bursts GH From: “Acromegaly” by Alan G. Harris, M.D. 1 Other Physiological Regulators of GH Secretion Pharmacologic Agents Used to Stimulate GH Secretion Amino Sleep Exercise Stress Acids Fasting Glucose Stimulate hypothalamic GHRH or Inhibit Somatostatin Hypothalamus GHRH SMS Hypoglycemia(Insulin) Pituitary L-dopa Arginine Clonidine GHRH + - SMS Pyridostigmine GH Target Tissues Metabolic & Growth Promoting GH Effects IGF-I Insulin-like growth factor I (IGF-I) Major Determinants of Circulating -

And Signifor LAR (Pasireotide) Prior Authorization with Quantity Limit
Signifor (pasireotide) and Signifor LAR (pasireotide) Prior Authorization with Quantity Limit Program Summary Signi for is the only target in this prior authorization program. Signifor LAR is not targeted in this pharmacy prior authorization program. This program applies to Commercial, NetResults A series, SourceRx, and Health Insurance Marketplace formularies. OBJECTIVE The intent of the Signifor (pasireotide) and Signifor LAR Prior Authorization (PA) program is to appropriately select patients for treatment according to product labeling and/or clinical studies and/or clinical practice guidelines. The program will approve for doses within the set limit. Doses above the set limit will be approved if the requested quantity is below the FDA limit and cannot be dose optimized or when the quantity is above the FDA limit and the prescriber has submitted documentation in support of therapy with a higher dose for the intended diagnosis. TARGET DRUGS Signifor (pasireotide) PRIOR AUTHORIZATION CRITERIA FOR APPROVAL Initial Evaluation Signifor will be approved for INITIAL USE when ALL of the following are met: 1. If Signifor, ONE of the following: A. The patient has a diagnosis of Cushing’s disease and ONE of the following: I. The patient has had recurrence or persistence after pituitary surgical resection OR II. The patient is not a candidate for pituitary surgical resection OR B. The patient has another FDA approved diagnosis AND 2. If Signifor LAR, ONE of the following: A. The patient has a diagnosis of acromegaly and ONE of the following: I. The use of requested agent is for adjunctive therapy with irradiation to alleviate acromegaly symptoms OR II. -

A Comparison Between Octreotide-LAR and Lanreotide-SR in the Chronic Treatment of Acromegaly
European Journal of Endocrinology (1999) 141 267–271 ISSN 0804-4643 CLINICAL STUDY A comparison between octreotide-LAR and lanreotide-SR in the chronic treatment of acromegaly R Cozzi, D Dallabonzana, R Attanasio, M Barausse and G Oppizzi Division of Endocrinology, Niguarda Hospital, Milan, Italy (Correspondence should be addressed to R Cozzi, Division of Endocrinology, Ospedale Niguarda, Piazza Ospedale Maggiore 3, I-20162 Milano, Italy; Email: [email protected]) Abstract Background: At present long-acting somatostatin analogs represent the first-line medical treatment of acromegaly. These drugs produce stable suppression of GH in most sensitive patients and IGF-I normalization in many; they also increase the compliance of acromegalic patients. The recent availability of octreotide (OC)-LAR, a somatostatin analog to be administered at 28-day intervals, has prompted us to compare, in the same group of patients, its effects and those of another somatostatin analog already available, lanreotide-SR (LSR, to be administered at 14-day intervals). Patients: Twelve somatostatin analog-sensitive acromegalic patients with active disease were enrolled in a prospective open sequential study after giving their informed consent. After chronic treatment with LSR (6–24 months), the patients were changed to treatment with OC-LAR, without wash-out. LSR had been administered at individually tailored dosages (30 mg i.m. at 7–21-day intervals, median 10 days – every 7 days in seven patients, 10 days in two patients, 14 days in two patients and 21 days in one patient) according to GH and IGF-I responses. Disease stability was obtained, as shown by maximal GH/IGF-I suppression without any significant hormonal change between the last two control measurements. -

Jcem2957.Pdf
SPECIAL FEATURE Clinical Review A Critical Analysis of Clinically Available Somatostatin Analog Formulations for Therapy of Acromegaly Robert D. Murray and Shlomo Melmed Department of Endocrinology (R.D.M.), Leeds Teaching Hospitals National Health Service Trust, Leeds LS9 7TF, United Kingdom; and Department of Medicine (S.M.), Cedars Sinai Medical Center, University of California Los Angeles School of Medicine, Los Angeles, Downloaded from https://academic.oup.com/jcem/article/93/8/2957/2598353 by guest on 24 September 2021 California 90048 Context: Short and long-acting somatostatin (SRIF) analogs are approved for clinical use in acro- megaly. Recent analysis of the relative efficacy of octreotide LAR and lanreotide SR on the GH-IGF-I axis in acromegaly favored octreotide LAR in the secondary treatment of patients not preselected by SRIF responsiveness. A novel aqueous formulation of lanreotide, lanreotide Autogel (ATG), has recently been approved and is the predominant (and only in the United States) formulation of lanreotide used clinically. Objective: We performed a critical review of SRIF analog treatment to establish the relative efficacy of three clinically available SRIF analog preparations, octreotide LAR, lanreotide SR, and lanreotide ATG (Somatuline depot in the United States) in control of the GH-IGF-I axis in acromegaly. Data Sources: Data were drawn from MEDLINE and the bibliography of analyses of long-acting SRIF analogs. Data Collection: We reviewed the largest studies of sc octreotide, octreotide LAR, and lanreotide SR, all that included biochemical end-point data for lanreotide ATG, and studies that directly compared the efficacy of octreotide LAR and lanreotide SR. Data Synthesis: Caveats considered included differences in baseline GH and IGF-I values, patient selection, and interassay and intraassay variability, confounding the analysis. -

V3.23 Durable Medical Equipment, Supplies, Vision and Hearing Hardware Nationwide by HCPCS Code
TABLE K. — DURABLE MEDICAL EQUIPMENT, SUPPLIES, VISION AND HEARING HARDWARE NATIONWIDE- CHARGES BY HCPCS CODE v3.23 (January - December 2018) PAGE 1 of 95 Status/ Usage HCPCS Code Modifier 1 HCPCS Code Description Charge GAAF Category Indicator 2 A0100 Blank NONEMERGENCY TRANSPORT TAXI Blank $20.81 HCPCS - Non-Drugs A0110 Blank NONEMERGENCY TRANSPORT BUS Blank $61.62 HCPCS - Non-Drugs A0120 Blank NONER TRANSPORT MINI-BUS Blank $183.09 HCPCS - Non-Drugs A0130 Blank NONER TRANSPORT WHEELCH VAN Blank $85.54 HCPCS - Non-Drugs A0140 Blank NONEMERGENCY TRANSPORT AIR Blank $1,211.38 HCPCS - Non-Drugs A0160 Blank NONER TRANSPORT CASE WORKER Blank $2.42 HCPCS - Non-Drugs A0170 Blank TRANSPORT PARKING FEES/TOLLS Blank $303.72 HCPCS - Non-Drugs A0180 Blank NONER TRANSPORT LODGNG RECIP Blank $809.69 HCPCS - Non-Drugs A0190 Blank NONER TRANSPORT MEALS RECIP Blank $181.99 HCPCS - Non-Drugs A0398 Blank ALS ROUTINE DISPOSBLE SUPPLS Blank $132.93 HCPCS - Non-Drugs A0422 Blank AMBULANCE 02 LIFE SUSTAINING Blank $126.28 HCPCS - Non-Drugs A4206 Blank 1 CC STERILE SYRINGE&NEEDLE Blank $0.94 HCPCS - Non-Drugs A4207 Blank 2 CC STERILE SYRINGE&NEEDLE Blank $0.94 HCPCS - Non-Drugs A4208 Blank 3 CC STERILE SYRINGE&NEEDLE Blank $0.94 HCPCS - Non-Drugs A4209 Blank 5+ CC STERILE SYRINGE&NEEDLE Blank $0.94 HCPCS - Non-Drugs A4210 Blank NONNEEDLE INJECTION DEVICE Blank $1,233.33 HCPCS - Non-Drugs A4211 Blank SUPP FOR SELF-ADM INJECTIONS Blank $57.07 HCPCS - Non-Drugs A4212 Blank NON CORING NEEDLE OR STYLET Blank $13.31 HCPCS - Non-Drugs A4213 Blank 20+ CC SYRINGE ONLY -

Acromegaly Caused by a Growth Hormone- Releasing Hormone Secreting Carcinoid Tumour of the Lung: the Effect of Octreotide Treatment
CAsE rEPorT Acromegaly caused by a growth hormone- releasing hormone secreting carcinoid tumour of the lung: the effect of octreotide treatment C.M. de Jager1,*, L.J.M. de Heide1, G. van den Berg4, A. Wolthuis2, W.D. van Schelven3 Departments of 1Internal Medicine, 2Clinical Chemistry and 3Nuclear Medicine, Leeuwarden Medical Centre, the Netherlands, 4Department of Endocrinology, University Medical Centre Groningen, University of Groningen, the Netherlands, *corresponding author (currently: Department of Internal Medicine, University Medical Centre Groningen): +31 (0)50-361 61 61, e-mail: [email protected] AbsTract in acromegaly, the overproduction of growth hormone tumour of the lung, whose pituitary MRI and the presence is usually caused by a pituitary adenoma. We report a of a lesion in the lung led us to the possibility of this 74-year-old woman with acromegaly caused by ectopic rare cause of acromegaly. The response to a long-acting overproduction of growth hormone-releasing hormone somatostatin analogue will be reported as well. (GHrH), a rare diagnosis. The GHrH appeared to be produced by a carcinoid tumour of the lung. Treatment with monthly long-acting octreotide resulted in a reduction CAsE rEPorT in the symptoms and normalisation of the insulin-like growth factor-i, which has been maintained for more than A 74-year-old woman was referred to the hospital with two years now. A review of literature concerning causes anaemia caused by iron deficiency (haemoglobin 3.6 and treatment of ectopic GHrH-producing tumours is mmol/l, normal 7.2-9.0, MCV 59 fl, normal 81-96, ferritin presented. -

How Are Growth Hormone and Insulin-Like Growth Factor-1 Reported As Markers for Drug Effectiveness in Clinical Acromegaly Resear
Pituitary (2018) 21:310–322 https://doi.org/10.1007/s11102-018-0884-4 How are growth hormone and insulin-like growth factor-1 reported as markers for drug effectiveness in clinical acromegaly research? A comprehensive methodologic review Michiel J. van Esdonk1,2 · Eline J. M. van Zutphen1 · Ferdinand Roelfsema3 · Alberto M. Pereira3 · Piet H. van der Graaf1,4 · Nienke R. Biermasz3 · Jasper Stevens5 · Jacobus Burggraaf1,2 Published online: 31 March 2018 © The Author(s) 2018 Abstract Objective In rare disease research, most randomized prospective clinical trials can only use limited number of patients and are comprised of highly heterogeneous populations. Therefore, it is crucial to report the results in such a manner that it allows for comparison of treatment effectiveness and biochemical control between studies. The aim of this review was to investigate the current methods that are being applied to measure and report growth hormone (GH) and insulin-like growth factor-1 (IGF-1) as markers for drug effectiveness in clinical acromegaly research. Search strategy A systematic search of recent prospective and retrospective studies, published between 2012 and 2017, that studied the effects of somatostatin analogues or dopamine agonists in acromegaly patients was performed. The markers of interest were GH, IGF-1, and the suppression of GH after an oral glucose tolerance test (OGTT). Additionally, the use of pharmacokinetic (PK) measurements in these studies was analyzed. The sampling design, cut-off for biochemical control, reported units, and used summary statistics were summarized. Results A total of 49 articles were selected out of the 263 screened abstracts. IGF-1 concentrations were measured in all 49 studies, GH in 45 studies, and an OGTT was performed in 11 studies.