Regulatory Mechanisms of Somatostatin Expression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Endocrine System Brightside July, 2019 by Dr
The Endocrine System Brightside July, 2019 By Dr. Derek Conte How does the body regulate and balance itself from minute to minute, hour to hour and month to month? What is it that allows the food we eat to be utilized for growth, healing and energy? What causes the female egg to drop each month or a mother’s milk to flow? The answer is the endocrine system, which is comprised of the hypothalamus, pituitary gland, pineal gland, thyroid and parathyroid glands, thymus gland, the adrenals, pancreas, ovaries and testes. The brain signals these specialized glands to release hormones to initiate essential chemical actions that sustain life. The word “endocrine” literally means “to cry inside” and that is exactly what happens when the endocrine system works. An example is growth hormone (GH) or somatotropin, responsible for growth and tissue repair. During exercise or when we have low blood sugar or high blood amino acid levels, the hypothalamus leaks (“cries”) growth hormone releasing hormone (GHRH) through very small vessels into the anterior pituitary gland which then leaks growth hormone into the general circulation, acting on cells for growth or replacement of old or damaged tissues. Pro ballplayers looking for an edge have been using growth hormone. The hormone that shuts this process off is called growth hormone inhibiting hormone (GHIH) or somatostatin (“growth stop”), released when blood sugar levels are high. If there ever is an excess of growth hormone, it can result in gigantism or acromegaly depending on whether its onset occurred before or after the growth plates in the bones have closed around the age of 17. -

Growth Hormone Booklet
GROWTH HORMONE AND PRADER-WILLISECOND EDITION SYNDROME A REFerence For FaMILies and Care ProViders Donald G. Goranson, Jr., Editor Growth Hormone and Prader-Willi Syndrome — Second Edition Published By: Prader-Willi Syndrome Association (Usa) 8588 Potter Park Drive, Suite 500 Sarasota, Florida 34238 Toll Free: 800-926-4797 Local: 941-312-0400 Fax: 941-312-0142 www.pwsausa.org © Copyright 2011 A Reference for Families and Care Providers Growth HORMONE AND PraderSECOND-WILLI EDITION Syndrome A REFerence For FaMILies and Care ProViders Donald G. Goranson, Jr., Editor Growth Hormone and Prader-Willi Syndrome — Second Edition A Reference for Families and Care Providers CONTENTS Acknowledgments....................................................................... 5 Introduction and History .............................................................. 7 Prader-Willi Syndrome and Growth ...................................................... 9 Effects of Growth Hormone Treatment in Children with PWS ................................ 20 What Is Involved in Growth Hormone Treatment? .......................................... 26 Questions, Wisdom and Survey Data from our Families ..................................... 34 Appendix: A. Overview of Prader-Willi Syndrome................................................ 40 B. Information Resources on Prader-Willi Syndrome .................................... 42 C. Information Resources on Growth Hormone Use and Products ........................ 43 D. Glossary of Terms ............................................................ -

Autism and Gastrointestinal Symptoms Karoly Horvath, MD, Phd and Jay A
Autism and Gastrointestinal Symptoms Karoly Horvath, MD, PhD and Jay A. Perman, MD Address In the last decade, the focus in autism research migrated Department of Pediatrics, University of Maryland School of Medicine, from psychological studies to exploration of the biologic 22 South Greene Street, N5W70, Box 140, Baltimore, basis of this devastating disorder. Studies using neuro- MD 21201-1595, USA. E-mail: [email protected] imaging and brain autopsy, as well as immunologic, genetic, metabolic, and gastrointestinal research efforts, have Current Gastroenterology Reports 2002, 4:251–258 Current Science Inc. ISSN 1522–8037 resulted in a significant amount of new information. Copyright © 2002 by Current Science Inc. However, this biologic research is still in the evolutionary stage, with many controversies, especially in brain and genetic research. For example, no consensus has been Autism is a collection of behavioral symptoms reached regarding the brain areas responsible for autism. characterized by dysfunction in social interaction and The gastrointestinal tract is an easier target for investi- communication in affected children. It is typically gation than the brain. However, only two studies of associated with restrictive, repetitive, and stereotypic gastrointestinal symptoms in autism were reported prior behavior and manifests within the first 3 years of life. to 1996. In 1971, a report of 15 randomly selected autistic The cause of this disorder is not known. Over the patients described six children who had bulky, odorous, past decade, a significant upswing in research has or loose stools, or intermittent diarrhea, and one with celiac occurred to examine the biologic basis of autism. disease [2]. -

Growth and Growth Hormone I
Pediat. Res. 2: 43-63 (1968) Dwarfism, constitutional hypoglycemia dwarfism, psychosocial insulin gonadal dysgenesis maternal depriva- growth hormone tion syndrome growth retardation panhypopituitarism Growth and Growth Hormone I. Changes in Serum Level of Growth Hormone Following Hypoglycemia in 134 Children with Growth Retardation S.L.KAPLAN, C.A.L.ABRAMS, J.J.BELL, F.A.CONTE and M.M.GRUMBACH[41] Department of Pediatrics, University of California, San Francisco Medical Center, San Francisco, California, and College of Physicians and Surgeons, Columbia University, New York, New York, USA Extract The change in levels of growth hormone in serum (SGH) following insulin-induced hypoglycemia was evaluated in 134 prepubertal children with growth retardation and 10 control subjects with normal growth patterns by radioimmunoassay, utilizing 131I-HGH and rabbit antiserum to human growth hormone. Mean maximum growth hormone concentration (m^g/ml) at any time during the test was: 10 Control subjects 12.4 53 Hypopituitarism 2.5 m^g or less in 52/53 20 Constitutional shortness of stature 12.5 22 Primordial dwarfism 12.1 9 XO gonadal dysgenesis 13.4 5 Delayed adolescence 11.8 5 Maternal deprivation 16.7 9 Psychosocial dwarfism 10.9 11 Miscellaneous disorders 7.0 Among factors found to affect the SGH response to insulin-induced hypoglycemia were: a) elevated fasting concentration of SGH which appeared to alter the responsiveness to stimulation; and b) age. The mean maximum SGH concentration of the control subjects following insulin-induced hypo- glycemia was 12.4 m^Mg/ml. In 52/53 patients with hypopituitarism, the SGH concentration was 1 m/*g or less at rest, with no increase or an increase to a maximum of 2.5 m^Mg/ml following hypoglycemia. -

HORMONES and SPORT Insulin, Growth Hormone and Sport
13 HORMONES AND SPORT Insulin, growth hormone and sport P H Sonksen Guy’s, King’s and St Thomas’ School of Medicine, St Thomas’ Hospital, London SE1 7EH, UK; Email: [email protected] Abstract This review examines some interesting ‘new’ histories of blood rather than urine samples. The first method has a insulin and reviews our current understanding of its window of opportunity lasting about 24 h after an injec- physiological actions and synergy with GH in the regu- tion and is most suitable for ‘out of competition’ testing. lation of metabolism and body composition. It reviews the The second method has reasonable sensitivity for as long as history of GH abuse that antedates by many years the 2 weeks after the last injection of GH and is uninfluenced awareness of endocrinologists to its potent anabolic actions. by extreme exercise and suitable for post-competition Promising methods for detection of GH abuse have been samples. This method has a greater sensitivity in men than developed but have yet to be sufficiently well validated to in women. The specificity of both methods seems accept- be ready for introduction into competitive sport. So far, ably high but lawyers need to decide what level of there are two promising avenues for detecting GH abuse. scientific probability is needed to obtain a conviction. Both The first uses immunoassays that can distinguish the methods need further validation before implementation. isomers of pituitary-derived GH from the monomer of Research work carried out as part of the fight against recombinant human GH. The second works through doping in sport has opened up a new and exciting area of demonstrating circulating concentrations of one or more endocrinology. -

Searching for Novel Peptide Hormones in the Human Genome Olivier Mirabeau
Searching for novel peptide hormones in the human genome Olivier Mirabeau To cite this version: Olivier Mirabeau. Searching for novel peptide hormones in the human genome. Life Sciences [q-bio]. Université Montpellier II - Sciences et Techniques du Languedoc, 2008. English. tel-00340710 HAL Id: tel-00340710 https://tel.archives-ouvertes.fr/tel-00340710 Submitted on 21 Nov 2008 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. UNIVERSITE MONTPELLIER II SCIENCES ET TECHNIQUES DU LANGUEDOC THESE pour obtenir le grade de DOCTEUR DE L'UNIVERSITE MONTPELLIER II Discipline : Biologie Informatique Ecole Doctorale : Sciences chimiques et biologiques pour la santé Formation doctorale : Biologie-Santé Recherche de nouvelles hormones peptidiques codées par le génome humain par Olivier Mirabeau présentée et soutenue publiquement le 30 janvier 2008 JURY M. Hubert Vaudry Rapporteur M. Jean-Philippe Vert Rapporteur Mme Nadia Rosenthal Examinatrice M. Jean Martinez Président M. Olivier Gascuel Directeur M. Cornelius Gross Examinateur Résumé Résumé Cette thèse porte sur la découverte de gènes humains non caractérisés codant pour des précurseurs à hormones peptidiques. Les hormones peptidiques (PH) ont un rôle important dans la plupart des processus physiologiques du corps humain. -
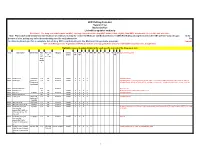
Drug Code List
HCPCS/Drug Code List Version 13.2 Revised 6/1/21 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Go to data.medicaid.gov for a complete list of drug NDCs participating in the Medicaid drug rebate program. Consult with each Managed Care Organization (MCO) about their coverage guidelines and prior authroization requirements, if applicable. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI ID DC Special Instructions req. of Limits OP OP TF for measure drug rebate ? 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmacological Management of Acromegaly: a Current Perspective
Neurosurg Focus 29 (4):E14, 2010 Pharmacological management of acromegaly: a current perspective SUNIL MANJILA , M.D.,1 Osmo N D C. WU, B.A.,1 FAH D R. KHAN , M.D., M.S.E.,1 ME H ree N M. KHAN , M.D.,2 BAHA M. AR A F AH , M.D.,2 AN D WA rre N R. SE L M AN , M.D.1 1Department of Neurological Surgery, The Neurological Institute, and 2Division of Clinical and Molecular Endocrinology, University Hospitals Case Medical Center, Cleveland, Ohio Acromegaly is a chronic disorder of enhanced growth hormone (GH) secretion and elevated insulin-like growth factor–I (IGF-I) levels, the most frequent cause of which is a pituitary adenoma. Persistently elevated GH and IGF-I levels lead to substantial morbidity and mortality. Treatment goals include complete removal of the tumor causing the disease, symptomatic relief, reduction of multisystem complications, and control of local mass effect. While trans- sphenoidal tumor resection is considered first-line treatment of patients in whom a surgical cure can be expected, pharmacological therapy is playing an increased role in the armamentarium against acromegaly in patients unsuitable for or refusing surgery, after failure of surgical treatment (inadequate resection, cavernous sinus invasion, or transcap- sular intraarachnoid invasion), or in select cases as primary treatment. Three broad drug classes are available for the treatment of acromegaly: somatostatin analogs, dopamine agonists, and GH receptor antagonists. Somatostatin analogs are considered as the first-line pharmacological treatment of acromegaly, although effica- cy varies among the different formulations. Octreotide long-acting release (LAR) appears to be more efficacious than lanreotide sustained release (SR). -

To Download a List of Prescription Drugs Requiring Prior Authorization
Essential Health Benefits Standard Specialty PA and QL List July 2016 The following products require prior authorization. In addition, there may be quantity limits for these drugs, which is notated below. Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, HIV SELZENTRY (maraviroc) None Cardiology Antilipemic JUXTAPID (lomitapide) 1 tab/day PRALUENT (alirocumab) 2 syringes/28 days REPATHA (evolocumab) 3 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 3 tabs/day FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) Soln None REVATIO (sildenafil) Tabs 3 tabs/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day UPTRAVI (selexipag) 2 tabs/day UPTRAVI (selexipag) Pack 2 packs/year VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Central Nervous System Anticonvulsants SABRIL (vigabatrin) pack None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) 20 cartridges/30 days Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Electrolyte & Renal Agents Diuretics KEVEYIS (dichlorphenamide) 4 tabs/day Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg -

DEPLETION of SOMATOSTATIN-LIKE IMMUNOREACTIVITY in the RAT CENTRAL NERVOUS SYSTEM by Cysteaminel
0270~6474/82/0202-0225$02.00/O The Journal of Neuroscience Copyright 0 Society for Neuroscience Vol. 2, No. 2, pp. 225-231 Printed in U.S.A. February 1982 DEPLETION OF SOMATOSTATIN-LIKE IMMUNOREACTIVITY IN THE RAT CENTRAL NERVOUS SYSTEM BY CYSTEAMINEl STEPHEN M. SAGAR,2 DONALD LANDRY,” WILLIAM J. MILLARD, THOMAS M. BADGER,* MICHAEL A. ARNOLD, AND JOSEPH B. MARTIN Department of Neurology and *Department of Gynecology, Massachusetts General Hospital, Boston, Massachusetts 02114 Received July 31, 1981; Accepted October 8, 1981 - Abstract Selective neurotoxins have been of value in providing a means for specifically interfering with the actions of endogenous neurotransmitter candidates. Others have shown cysteamine (CSH) to deplete the gastrointestinal tract and hypothalamus of rats of immunoreactive somatostatin, suggesting a toxic action of that compound directed against somatostatin-containing cells. The present study further defines the actions of cysteamine on somatostatin in the central nervous system (CNS). Cysteamine hydrochloride administered subcutaneously results in a depletion of somatostatin-like immunoreactivity (SLI) in the retina, brain, and cervical spinal cord of rats. The effect is demon- strable at doses of 30 mg/kg of body weight and above, occurs within 2 to 4 hr of a single injection of the drug, and is largely reversible within 1 week. The mean depletion of SLI observed within the CNS varies from 38% in cerebral cortex to 65% in cervical spinal cord 24 hr following administration of CSH, 300 mg/kg of body weight, S.C. By gel permeation chromatography, all molecular weight forms of SLI are affected, with the largest reductions in those forms that co-chromatograph with synthetic somatostatin-14 and somatostatin-28. -

Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future
International Journal of Molecular Sciences Review Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future Anna Kathrin Stueven 1, Antonin Kayser 1, Christoph Wetz 2, Holger Amthauer 2, Alexander Wree 1, Frank Tacke 1, Bertram Wiedenmann 1, Christoph Roderburg 1,* and Henning Jann 1 1 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Hepatology and Gastroenterology, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (A.K.S.); [email protected] (A.K.); [email protected] (A.W.); [email protected] (F.T.); [email protected] (B.W.); [email protected] (H.J.) 2 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Nuclear Medicine, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (C.W.); [email protected] (H.A.) * Correspondence: [email protected]; Tel.: +49-30-450-553022 Received: 3 May 2019; Accepted: 19 June 2019; Published: 22 June 2019 Abstract: In recent decades, the incidence of neuroendocrine tumors (NETs) has steadily increased. Due to the slow-growing nature of these tumors and the lack of early symptoms, most cases are diagnosed at advanced stages, when curative treatment options are no longer available. Prognosis and survival of patients with NETs are determined by the location of the primary lesion, biochemical functional status, differentiation, initial staging, and response to treatment. Somatostatin analogue (SSA) therapy has been a mainstay of antisecretory therapy in functioning neuroendocrine tumors, which cause various clinical symptoms depending on hormonal hypersecretion. Beyond symptomatic management, recent research demonstrates that SSAs exert antiproliferative effects and inhibit tumor growth via the somatostatin receptor 2 (SSTR2). -

Plasma Somatostatin and Cholecystokinin Levels in Preterm Infants and Their Mothers at Birth
0031-399819513706-0771$03.0010 PEDIATRIC RESEARCH Vol. 37, No. 6, 1995 Copyright O 1995 International Pediatric Research Foundation, Inc Printed in U.S.A. Plasma Somatostatin and Cholecystokinin Levels in Preterm Infants and Their Mothers at Birth C.-J. TORNHAGE, F. SERENIUS, K. UVNAS-MOBERG,AND T. LINDBERG Department of Pediatrics, UmeB University, UmeB [C.-J.T., F.S., T.L.] and Department of Pharmacology, Karolinska Institute, Stockholm, Sweden [K. U-M.] Regulatory gut peptides play an important role in regulating same. They were also independent of sex, birth weight, gesta- the gastrointestinal tract. Our knowledge about the pattern of tional age, umbilical cord blood pH, or glucose level. In mothers, secretion and function of these peptides is scanty in preterm but not in infants, plasma SS levels were higher after vaginal infants. Therefore, plasma somatostatin (SS) and cholecystokinin delivery than after cesarean section. After multiple birth, new- (CCK) levels were estimated just after birth in 65 mothers and 73 born plasma SS, but not plasma CCK, was significantly lower preterm infants (umbilical cord blood). The gestational age was than after single birth (9.1 + 7.7 versus 16.9 2 12.7 pmol/L). 32 (24-36 median ranges) wk and birth weight 1900 (475-3350) (Pediatr Res 37: 771-776, 1995) g. The umbilical cord blood pH was 7.32 + 0.10 (mean t- SD). After Sep-Pak-C,, semichromatography of plasma, SS and CCK Abbreviations were analyzed by RIA. Both plasma SS and CCK levels were SS, somatostatin significantly higher in infants than in mothers (SS = 14.5 i.