Gaya District
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ground Water Year Book, Bihar (2015 - 2016)
का셍ााल셍 उप셍ोग हेतू For Official Use GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD जल ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पूर्वी क्षेत्र, पटना सितंबर 2016 MID-EASTERN REGION, PATNA September 2016 ` GOVT. OF INDIA जल ल MINISTRY OF WATER RESOURCES जल CENTRAL GROUND WATER BOARD ,, (2015-2016) GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) म鵍य पर्वू ी क्षेत्र, पटना MID-EASTERN REGION, PATNA सितंबर 2016 September 2016 GROUND WATER YEAR BOOK, BIHAR (2015 - 2016) CONTENTS CONTENTS Page No. List of Tables i List of Figures ii List of Annexures ii List of Contributors iii Abstract iv 1. INTRODUCTION.............................................................................................................1 2. HYDROGEOLOGY..........................................................................................................1 3. GROUND WATER SCENARIO......................................................................................4 3.1 DEPTH TO WATER LEVEL........................................................................................8 3.1.1 MAY 2015.....................................................................................................................8 3.1.2 AUGUST 2015..............................................................................................................10 3.1.3 NOVEMBER 2015........................................................................................................12 3.1.4 JANUARY 2016...........................................................................................................14 -
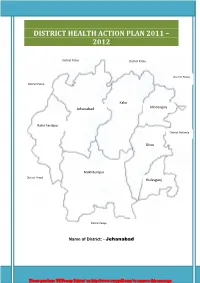
District Health Action Plan 2011 – 2012
DISTRICT HEALTH ACTION PLAN 2011 – 2012 District Patna District Patna District Patna District Patna Kako Modanganj Jehanabad Ratni Faridpur District Nalanda Ghosi Makhdumpur District Arwal Hulasganj District Gaya Name of District: - Jehanabad Please purchase 'PDFcamp Printer' on http://www.verypdf.com/ to remove this message. Acknowledgements This District Health Action plan prepared Under a Short & Hard Process of about survey of one month and this was a good Opportunity to revisit the situation of health services status and national programmes in district as well as to have a positive dialogue with departments like Public Health Engineering, Women and Child Development, Maternal and Child Health care etc. This document is an outcome of a collective effort by a number of individuals, related to our institutions and programmes:- Smt. Palka Shahni ,Chairperson of District Health Society, Jehanabad was a source of inspiration towards this effort vide her inputs to this process during D.H.S review meetings. Dr.Arvind kumar (A.C.M.O) Nodal officer for this action plan who always supported this endeavor through his guiding words and language. Mr. Nimish Manan , District Programme Manager was in incharge for the development of the DHAP(2011-12) . Mr Ravi Shankar Kumar , Distirct Planning Coordinator has given full time effort in developing DHAP(2011-12). Mr. Kaushal Kumar Jha, District Account Manager has put huge effort in financial Planning. Mr. Arvind Kumar, M&E Officer is the technical advisor for the data introduced inside this DISTRICT HEALTH ACTION PLAN. Mr. Manish Mani & Sefali from PHRN have given huge support. All district level Programme officer for various Health Programmes, B.H.Ms, M.O.I .Cs, PHCs, Field Office Staff have supported with their full participations, cooperation and learning spirit through out this process. -

Dto Name Jun 2016 Jun 2016 1Regn No V Type
DTO_NAME JUN_2016 JUN_2016_1REGN_NO V_TYPE TAX_PAID_UPTO O_NAME F_NAME ADD1 ADD2 CITY PINCODE STATUS TAX_AMOUNT PENALTY TOTAL RANCHI N N JH01BZ8715 BUS 19-08-16 KRISHNA KUMHARS/O LATE CHHOTUBARA MURIKUMHAR CHHOTASILLI MURI RANCHI SUCCESS 6414 1604 8018 RANCHI N N JH01G 4365 BUS 15-08-16 ASHISH ORAONS/O JATRU ORAONGAMARIYA SARAMPO- MURUPIRIRANCHI -PS- BURMU 000000 SUCCESS 5619 1604 7223 RANCHI N N JH01BP5656 BUS 29-06-16 SURESH BHAGATS/O KALDEV CHIRONDIBHAGAT BASTIBARIATU RANCHI SUCCESS 6414 6414 12828 RANCHI N N JH01BC8857 BUS 22-07-16 SDA HIGH SCHOOLI/C HENRY SINGHTORPA ROADKHUNTI KHUNTI , M- KHUNTI9431115173 SUCCESS 6649 3325 9974 RANCHI Y Y JH01BE4699 BUS 21-06-16 DHANESHWARS/O GANJHU MANGARSIDALU GANJHU BAHERAPIPARWAR KHELARIRANCHI , M- 9470128861 SUCCESS 5945 5945 11890 RANCHI N N JH01BF8141 BUS 19-08-16 URSULINE CONVENTI/C GIRLSDR HIGH CAMIL SCHOOL BULCKERANCHI PATH , M- RANCHI9835953187 SUCCESS 3762 941 4703 RANCHI N N JH01AX8750 BUS 15-08-16 DILIP KUMARS/O SINGH SRI NIRMALNEAR SINGH SHARDHANANDANAND NAGAR SCHOOLRANCHI KAMRE , M- RATU 9973803185SUCCESS 3318 830 4148 RANCHI Y Y JH01AZ6810 BUS 12-01-16 C C L RANCHII/C SUPDT.(M)PURCHASE COLLY MGR DEPARTMENTDARBHANGARANCHI HOUSE PH.NO- 0651-2360261SUCCESS 19242 28862 48104 RANCHI Y Y JH01AK0808 BUS 24-04-16 KAMAKHYA NARAYANS/O NAWAL SINGH KISHORECHERI KAMRE NATHKANKE SINGH RANCHI SUCCESS 4602 2504 7106 RANCHI N N JH01AE6193 BUS 04-08-16 MRS. GAYTRIW/O DEVI SRI PRADEEPKONBIR KUMARNAWATOLI GUPTA BASIAGUMLA SUCCESS 4602 2504 7106 RANCHI Y Y JH01AE0222 BUS 22-06-16 RANCHI MUNICIPALI/C CEO CORPORATIONGOVT OF JHARKHANDRANCHI RANCHI SUCCESS 2795 3019 5814 RANCHI N N JH01AE0099 BUS 06-07-16 RANCHI MUNICIPALI/C CEO CORPN.GOVT. -

State District Name of Bank Bank Branch/ Financial Literacy Centre
State District Name of Bank Branch/ Address ITI Code ITI Name ITI Address State District Phone Email Bank Financial Category Number Literacy Centre Bihar Araria State Araria Lead Bank Office, PR10000055 Al-Sahaba Industrial P Alamtala Forbesganj Bihar Araria NULL Bank of ADB Building, Training Institute India Araria, Pin- 854311 Bihar Arwal PNB ARWAL ARWAL PR10000083 Adarsh ITC P Umerabad Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000284 Shakuntalam ITC P Prasadi English Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000346 Aditya ITC P At. Wasilpur, Main Road, Bihar Arwal NULL P.O. Arwal, Bihar Arwal PNB ARWAL ARWAL PR10000396 Vikramshila Private P At. Rojapar, P.O. Arwal Bihar Arwal NULL ITI Bihar Arwal PNB ARWAL ARWAL PR10000652 Ram Bhaman Singh P At-Purani Bazar P.o+P.S- Bihar Arwal NULL Private ITI Arwal Bihar Arwal PNB ARWAL ARWAL PR10000677 Sukhdeo Institute Of P Kurtha, Arwal Bihar Arwal NULL Tecnology Private ITI, Bihar Arwal PNB ARWAL ARWAL PR10000707 Dr. Rajendra Prasad P Mubarkpur, Kurtha Arwal Bihar Arwal NULL Private ITI, Bihar Aurangabad PUNJAB DAUDNAGAR DAUDNAGAR PR10000027 New Sai Private ITI- P Aurangabad Road, Bihar Aurangabad NULL NATIONA Bhakharuan More, , Tehsil- L BANK Daudnagar , , Aurangabad - 824113 Bihar Aurangabad PUNJAB AURANGABAD AURANGABAD PR10000064 Adharsh Industrial P Josai More Udyog Bihar Aurangabad NULL NATIONA Training Centre Pradhikar Campus L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000108 Sardar Vallabh Bhai P Daudnagar Bihar Aurangabad NULL BIHAR Patel ITC, Daudnagar GRAMIN BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000142 Adarsh ITC, P AT-,Growth centre ,Jasoia Bihar Aurangabad NULL BIHAR Daudnagar More Daudnagar GRAMIN BANK Bihar Aurangabad PUNJAB RATANUA RATANUA PR10000196 Progresive ITC P At-Growth Center Josia Bihar Aurangabad NULL NATIONA More L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000199 Arya Bhatt ITC P Patel Nagar, Daud Nagar Bihar Aurangabad NULL BIHAR GRAMIN BANK Bihar Aurangabad PUNJAB OLD GT RD. -

TRAFFIC Bulletin
TRAFFIC 2 BULLETIN HAWKSBILL TURTLE TRADE IN PAPUA NEW GUINEA IVORY IN THAILAND AND VIET NAM JUNE 2009 VOL. 22 NO. 2 22 NO. VOL. JUNE 2009 The journal of the TRAFFIC network disseminates information on the trade in wild animal and plant resources S E I Z U R E S A N D P R O S E C U T I O N S THE TRAFFIC BULLETIN SEIZURES AND PROSECUTIONS SECTION IS CITES (Convention on International Trade in Endangered Species of Wild Fauna and Flora) SPONSORED BY THE FORESTRY establishes international controls over trade in wild plants and animals, or related products, of species that BUREAU, COUNCIL OF AGRI CULTURE, have been, or may be, threatened due to excessive commercial exploitation. Parties have their own TAIWAN: COMMITTED TO SUPPORTING legislative vehicle by which to meet their obligations under CITES. The species covered by CITES are listed CITES ENFORCEMENT in three Appendices, according to the degree of protection they need: The cases reported below represent a selection of APPENDIX I includes species threatened with extinction which are or may be threatened by trade. recent seizures and prosecutions that have taken place Trade in specimens of these species is permitted only in exceptional circumstances. An export permit from around the world. The sources of this information are the country of origin (or a re-export certificate from other exporting countries) and an import permit from the cited at the end of each country section. The CITES country of importation are required. Appendix-listing for each species is placed in parentheses, where appropriate. -

Compliance Or Defiance? the Case of Dalits and Mahadalits
Kunnath, Compliance or defiance? COMPLIANCE OR DEFIANCE? THE CASE OF DALITS AND MAHADALITS GEORGE KUNNATH Introduction Dalits, who remain at the bottom of the Indian caste hierarchy, have resisted social and economic inequalities in various ways throughout their history.1 Their struggles have sometimes taken the form of the rejection of Hinduism in favour of other religions. Some Dalit groups have formed caste-based political parties and socio-religious movements to counter upper-caste domination. These caste-based organizations have been at the forefront of mobilizing Dalit communities in securing greater benefits from the Indian state’s affirmative action programmes. In recent times, Dalit organizations have also taken to international lobbying and networking to create wider platforms for the promotion of Dalit human rights and development. Along with protest against the caste system, Dalit history is also characterized by accommodation and compliance with Brahmanical values. The everyday Dalit world is replete with stories of Dalit communities consciously or unconsciously adopting upper-caste beliefs and practices. They seem to internalize the negative images and representations of themselves and their castes that are held and propagated by the dominant groups. Dalits are also internally divided by caste, with hierarchical rankings. They themselves thus often seem to reinforce and even reproduce the same system and norms that oppress them. This article engages with both compliance and defiance by Dalit communities. Both these concepts are central to any engagement with populations living in the context of oppression and inequality. Debates in gender studies, colonial histories and subaltern studies have engaged with the simultaneous existence of these contradictory processes. -

Aurangabad, Bihar
DISTRICT HEALTH SOCIETY AURANGABAD , B IHAR District Health Action Plan 2012-2013 Prepared By: Sagar (District Programme Manager) Ashwini Kumar (District Accounts Manager) Rajeev Ranjan (District Monitoring & Evaluation Officer) B.B. Vikrant (District Planning Coordinator) Rahul Kumar Singh (District Community Mobilizer, ASHA) Under the able Guidance of: Dr. Parshuram Bharti Mr. Abhay Kumar Singh (IAS) Civil Surgeon cum Member Secretary District Magistrate cum Chairman District Health Society, Aurangabad District Health Society, Aurangabad District Health Society, Aurangabad Page -1- Table of contents Foreword Table of Contents Topics Page CHAPTER 1 INTRODUCTION 01-05 CHAPTER 2 DISTRICT PROFILE 06-14 Introduction 06 Geography 06 Demography 07 Physiography 07 History 08 Administrative Setup 09-11 Communication Map of the district 12 Health Facilities Map of the district 13 Population Details 14 CHAPTER 3 SITUATIONAL ANALYSIS 15-29 Gaps in Infrastructure 15-18 Aurangabad at a Glance 19 Health Facilities 20 Human Resource 21-22 ASHA Status 23 MAMTA Status 24 Bed Availability 25 Basic Facilities at Rural Institutions 26 District Hospital 27 Indicators of RCH 28 CHAPTER 4 SETTING OBJECTIVES AND SUGGESTED 30-36 PLAN OF ACTION Introduction 30 Targeted Objectives and Suggested Strategies 30-36 (Maternal Health, FRUs, RCH Services, VHSND, JBSY, IMNCI, Caesarean, JSY, Institutional Delivery, NPSGK, NRC) CHAPTER 5 BUDGET 37 -48 District Health Society, Aurangabad Page -2- Foreword It is very rightly said that Health is Wealth. The Importance of Health in the process of economic and social development and improving the quality of life of our citizens, cannot be denied. Recognizing the importance of Health, the Government of India has launched the National Rural Health Mission on 12 th April 2005 in India. -

Ministry of Road Transport & Highways
Ministry of Road Transport & Highways Government of India Consultancy Services for preparation of Feasibility Study and Detailed Project Report for Improvement to Two Lane with Paved shoulder of (i) Stretch from Bihar- Jharkhand Border – Raniganj – Imamganj – Sherghati of Daltonganj (on NH-39, new) – Sagalim – Tarhasi – Manatu – Chak - Raniganj – Imamganj – Sherghati road & (ii) stretch from Dangwa (Bihar-Jharkhand Border) – Nabinagar – Barun (NH-02) of Chhatarpur (NH-98) – Japla – Dangwa - Nabinagar – Barun (NH-02) road in Bihar on EPC Mode REQUEST FOR PROPOSAL (RFP) (International Competitive Bidding) July, 2016 1 INDEX Sl. No. Contents Page No. 1 Notice for inviting the proposals for Consultancy services 1 2 Letter of Invitation 2-15 3. Annex - I : List of Project along with Package Nos. 16 4. Data Sheet 17-22 5. Appendix - I : Terms of Reference 23-66 6. Supplement -I: Additional Requirements for Hill Roads 67-69 7. Supplement - II: Additional Requirements for Bridges 70-74 8 Supplement – III: Additional requirement for safety audit 75-77 9. Enclosure - I : Manning Schedule 78 10 Enclosure - II : Qualification Requirements of Key Personnel 79-82 11. Enclosure - III : Schedule for Submission of Reports and Documents 83 12. Appendix - II : Formats for Proof of Eligibility 84-90 13. Appendix - III : Formats for Technical Proposals 91-103 14. Appendix - IV : Formats for Financial Proposals 104-110 15. Appendix - V : Draft Contract Agreement 111-148 2 Ministry of Road Transport & Highways Government of India MORT&H intends to take up the Consultancy Services for preparation of Feasibility Study and Detailed Project Report for Improvement to Two Lane with Paved shoulder of (i) Stretch from Bihar- Jharkhand Border – Raniganj – Imamganj – Sherghati of Daltonganj (on NH-39, new) – Sagalim – Tarhasi – Manatu – Chak - Raniganj – Imamganj – Sherghati road & (ii) stretch from Dangwa (Bihar-Jharkhand Border) – Nabinagar – Barun (NH-02) of Chhatarpur (NH-98) – Japla – Dangwa - Nabinagar – Barun (NH-02) road in Bihar on EPC / PPP Mode. -

INDIA Public Disclosure Authorized
E-339 VOL. 1 INDIA Public Disclosure Authorized THIRD NATIONAL HIGHWAY WORLD BANK PROJECT Public Disclosure Authorized CONSOLIDATED EIA REPORT (CONSTRUCTION PACKAGES 11- V) Public Disclosure Authorized NATIONAL HIGHWAYS AUTHORITY OF INDIA NEW DELHI (Ministry of Surface Transport) March, 2000 Public Disclosure Authorized 4 4 =fmmm~E-339 VOL. 1 INDIA THIRD NATIONAL HIGHWAY WORLD BANK PROJECT CONSOLIDATED EIA REPORT (CONSTRUCTION PACKAGES II - V) NATIONAL HIGHWAYS AUTHORITY OF INDIA NEW DELHI (Ministry of Surface Transport) March, 2000 TABLE OF CONTENTS THE REPORT I The Project............................................................... 1-1 1.1 The Project Description ............................................................... ]-II 1.2 Overall Scope of Project Works ............................................................ 1-3 1.3 Proposed Improvement of the Project Highway ................... ................ 1-3 1.4 Scope of Environmental Impact Assessment ................. ........................... 1-6 1.5 Structure of The Consolidated EIA Report ........................................... 1-7 2 Policy, Legal And Administrative Framework ................... ........................... 2-1 2.1 Institutional Setting for the Project .. 2-1 2.1.1 The National Highways Authority of India (NHAI) 2-1 2.1.2 Project Implementation Units (PIU) .................................................. 2-1 2.1.3 State Public Works Departments (PWDs) .2-2 2.2 Institutional Setting in the Environmental Context .................... 2-2 2.2.1 Ministry -

Adolescents Health and Development Program in Bihar
Request for Proposal CSO/NGO partner agency Project Name: “Adolescents Health and Development Program in Bihar Engender Health Deadline for receipt of proposals: 10th September 2020 1 Contents 1. RFP NOTICE ................................................................................................................. 1 2. OUR MISSION ............................................................................................................... 3 3. ORGANIZATIONAL BACKGROUND ............................................................................. 4 4. PROJECT GOALS AND OBJECTIVES ......................................................................... 4 5. SCOPE OF WORK ........................................................................................................ 4 6. SUBMISSION OF PROPOSALS .................................................................................... 5 7. OTHER REQUIREMENTS ............................................................................................. 6 8. EVALUATION OF THE PROPOSAL .............................................................................. 6 9. DISCUSSIONS AND AWARD ........................................................................................ 7 10. OFFER VERIFICATION ............................................................................................. 7 11. FALSE STATEMENTS IN OFFER .............................................................................. 7 12. RESERVED RIGHTS ................................................................................................ -

List of PMGSY Works Pending Due to Forest Land Road Sanctione Road Length Expendit District Name of Package Sanctione Work Stage of Sr.No
List of PMGSY Works pending due to Forest Land Road Sanctione Road Length Expendit District Name of Package Sanctione Work Stage of Sr.No. Block Name Road Name Length d Cost Completed ure Contractor Name Remarks Name Division No. d Year Type Progress (Kms) (in Lakh) Till Date (in Lakh) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 1 Aurangabad Aurangabad Kutumba BR02R593 2016-17 ROAD L081-T03 DEO 1.7 98.28 1.7 30.29 Surface SRI RAMANDAN 700 mt Forest Bat-I AMBA ROAD Course / BT SINGH [15 Dec 2016] Land TO CHANDAUL Stage (TRACK81) 2 Aurangabad Aurangabad Deo BR02R588 2016-17 ROAD L059-T04 TO 3.05 158.82 1.5 26.64 Surface SRI RAMANDAN 1.55 Km Forest Bat-I TATARIYA Course / BT SINGH [15 Dec 2016] Land (TRACK59) Stage 3 Aurangabad Aurangabad Deo BR02R586 2016-17 ROAD T09-DEO TO 8.18 449.51 7 243.16 Surface ARVIND SINGH [06 1.18 km Forest Bat-I BHALUAHI Course / BT Jan 2017] Land (VR9) Stage 4 Aurangabad Aurangabad Madanpur BR02R619 2016-17 ROAD L115-T05 12.05 601.21 2 0 Surface SHARWAN & 10.05 Km Forest Bat-I Chilami To Course / BT SUNNY Land Pachrukhiya Stage CONSTRUCTION (TRACK115) P.V.T L.T.D [06 Jan 2017] 5 Gaya Gaya Bodh Gaya BR12R292 2013-14 ROAD L073-Lalpur To 1.617 63.85 0 0 No Progress Forest Land in Batch-I Bangal Bigha Entry Full length (VR73) 6 Gaya Gaya Tankuppa BR12R373 2013-14 ROAD L022-Chamukhap 1.77 68.18 0 15.06 Pending - M/S AADARSH Forest land-1.20 Batch-I road to Khalari Forest CONSTRUCTION Km (TRACK22) Clearance [08 Jan 2014] 7 Gaya Gaya Fatehpur BR-12R- 2013-14 ROAD T04 - 18.794 1,100.02 0 556.5 Pending - M/S Kalyani Forest land-6.00 484 Batch-II FatehpurRajauli Forest Construction [10 Jan Km Road to Patwansh Clearance 2015], M/S Kalyani (VR4) Construction [24 Dec 2014] 8 Gaya Neemchak Manpur BR12R567 2013-14 ROAD L046 - Amra T04 2.035 83.34 0 58.07 Pending - Rajeev Kumar Singh Forest Land in Bathani Batch-II To Bagahi Kala Forest [19 Jun 2014] 536 M length H. -

Womens' Empowerment
Directory of Voluntary Organisations Women’s Empowerment 2010 Documentation Centre for Women and Children (DCWC) National Institute of Public Cooperation and Child Development 5, Siri Institutional Area, Hauz Khas, New Delhi – 110016 Number of Copies: 100 Copyright: National Institute of Public Cooperation and Child Development, 2010 Project Team Project In-charge : Mrs. Meenakshi Sood Project Team : Ms. Renu Banker Ms. Alpana Kumari Computer Assistance : Mrs. Sandeepa Jain Mr. Abhishek Tiwari Acknowledgements : Ministry of Women and Child Development Planning Commission Voluntary Organisations Ministry of Rural Development Ministry of Panchayati Raj Ministry of Tribal Affairs Ministry of Urban Development DISCLAIMER All efforts have been made to verify and collate information about organisations included in the Directory. Information has been collected from various sources, namely directories, newsletters, Internet, proforma filled in by organisations, telephonic verification, letter heads, etc. However, NIPCCD does not take any responsibility for any error that may inadvertently have crept in. The address of offices of organisations, telephone numbers, e-mail IDs, activities, etc. change from time to time, hence NIPCCD may not be held liable for any incorrect information included in the Directory. Foreword Voluntary organisations play a very important role in society. They take up activities in the area of their expertise and provide support to the community in whose welfare they have interest. Social development has been ranked high on the priority list of Government programmes since Independence, and voluntary organisations have been equal partners in accelerating the pace of development. Being in close proximity to the community, voluntary organisations have done pioneering work in many areas, rendered productive services, highlighted several social problems, undertaken advocacy, and lobbied for the rights of the underprivileged.