The Dutchess County Project After Five Years
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fergie the Dutchess Mp3, Flac, Wma
Fergie The Dutchess mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Electronic / Hip hop / Pop Album: The Dutchess Country: US Released: 2006 Style: RnB/Swing, Pop Rap, Electro, Ballad MP3 version RAR size: 1892 mb FLAC version RAR size: 1848 mb WMA version RAR size: 1867 mb Rating: 4.5 Votes: 459 Other Formats: MP1 AU MOD MP4 AIFF MIDI FLAC Tracklist Hide Credits Fergalicious Bass, Drum Programming – Will.i.am*Edited By [Additional Pro Tools] – John HanesEngineer – Padraic Kerin, Will.i.am*Engineer [Assistant Mix] – Tim 1 4:52 RobertsMixed By – Serban GheneaProducer, Featuring, Keyboards – Will.I.Am*Written- By – Dania Maria Birks, Derrick Rahming, Fatima Shaheed, Juana Michelle Burns, Juanita A. Lee, Kim Nazel, Stacy Ferguson, Will Adams Clumsy Drum Programming – Will.I.Am*Engineer – Padraic Kerin, Will.i.am*Engineer 2 4:00 [Assistant Mix] – Ryan KennedyMixed By – Tony MaseratiProducer – Will.I.Am*Written- By – Bobby Troup, Stacy Ferguson, Will Adams All That I Got (The Make Up Song) Arranged By [Strings], Conductor [Strings], Producer [Additional Vocals] – Ron FairBacking Vocals – Fergie , Theresa Jones Bailey*Bass – Mike Valerio, Trey HenryBass, Keyboards, Drum Programming, Engineer – Keith HarrisCello – Cecilia Tsan, David Low, Larry Corbett, Suzie KatayamaEdited By [Additional Pro Tools] – Tal HerzbergEngineer – Will.i.am*Engineer [Additional] – Tal HerzbergEngineer [Assistant Mix] – Ryan KennedyEngineer [Assistant] – Neil TuckerFeaturing – Will.I.Am*Guitar – J. 3 CurtisMixed By – Tony MaseratiProducer – Keith Harris, Will.I.Am*Recorded -

BHM 2008 Spring.Pdf
MAGAZINE COMMITTEE OFFICER IN CHARGE Bill Booher CHAIRMAN Lawrence S Levy VICE CHAIRMEN A Message From the Chairman 1 Tracy L. Ruffeno Gina Steere COPY EDITOR Features Kenneth C. Moursund Jr. EDITORIAL BOARD Katrina’s Gift ................................................. 2 Denise Doyle Samantha Fewox Happy 100th, 4-H .......................................... 4 Katie Lyons Marshall R. Smith III Todd Zucker 2008 RODEOHOUSTONTM ................................. 6 PHOTOGRAPHERS page 2 Debbie Porter The Art of Judging Barbecue .......................... 12 Lisa Van Etta Grand Marshals — Lone Stars ...................... 14 REPORTERS Beverly Acock TM Sonya Aston The RITE Stuff — 10 Years of Success ........ 16 Stephanie Earthman Baird Bill R. Bludworth Rodeo Rookies ............................................... 18 Brandy Divin Teresa Ehrman Show News and Updates Susan D. Emfinger Kate Gunn Charlotte Kocian Corral Club Committees Spotlight ................ 19 Brad Levy Melissa Manning Rodeo Roundup ............................................. 21 Nan McCreary page 4 Crystal Bott McKeon Rochell McNutt Marian Perez Boudousquié Ken Scott Sandra Hollingsworth Smith Kristi Van Aken The Cover Hugo Villarreal RODEOHOUSTON pickup men, Clarissa Webb arguably one of the hardest- HOUSTON LIVESTOCK SHOW working cowboys in the arena, AND RODEO MAGAZINE COORDINATION will saddle up for another year MARKETING & PUBLIC RELATIONS in 2008. DIVISION MANAGING DIRECTOR, page 14 COMMUNICATIONS Clint Saunders Houston Livestock Show and Rodeo™ COORDINATOR, COMMUNICATIONS Kate Bradley DESIGN / LAYOUT CHAIRMAN OF THE BOARD: PRESIDENT: CHIEF OPERATING OFFICER: Amy Noorian Paul G. Somerville Skip Wagner Leroy Shafer STAFF PHOTOGRAPHERS VICE PRESIDENTS: Francis M. Martin, D.V. M. C.A. “Bubba” Beasley Danny Boatman Bill Booher Brandon Bridwell Dave Clements Rudy Cano Andrew Dow James C. “Jim” Epps Charlene Floyd Rick Greene Joe Bruce Hancock Darrell N. Hartman Dick Hudgins John Morton John A. -
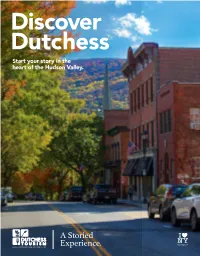
Destination Guide 2020 All Phone Numbers Are in (845) Area Code Unless Otherwise Indicated
ELCOMEELCOME Dutchess County delivers the rugged, natural beauty of the Hudson Valley, world renowned dining, and a storied history of empire builders, visionaries and artists. Take a trip here to forge indelible memories, and discover that true wealth is actually the exceptional experiences one shares in life. Old Rhinebeck Aerodrome, Red Hook Table of Contents Events . 2 Eastern Dutchess . .. 30 Groups, Meetings Explore Dutchess by Community . 4 Where to Stay . 38 & Conferences . 46 Northern Dutchess . 6 Places to Eat . 42 Accessible and LGBTQ Travel . 47 Central Dutchess . 14 Colleges . 44 About Dutchess . 48 Southern Dutchess . 22 Weddings . 45 Transportation & Directions . 49 Dutchess Tourism, Inc. is On the cover: Main Street Beacon accredited by the Destination Marketing Accreditation Program (DMAP) of DutchessTourism.com #MyDutchessStory Destinations International. Notes: To the best of our knowledge, the information in this guide is correct as of March 1, 2020. Due to possible changes, we Custom publishing services provided by recommend that you contact a site before visiting. This guide lists only those facilities that wish to be included. Listings do not represent an endorsement. The programs provided by this agency are partially funded by monies received from the County of ChronogramMedia Dutchess. This travel guide is published by Dutchess Tourism, Inc., 3 Neptune Rd., Suite A11A, Poughkeepsie, NY 12601, the County of Dutchess, in cooperation with the New York State Department of Economic Development and the I Love New York 314 Wall Street, Kingston, NY 12401 campaign. ® I LOVE NEW YORK is a registered trademark and service mark of the New York State Department of Economic ChronogramMedia.com Development; used with permission. -

Simplicity Kumar Was Recognized with the Outstanding Youth Award
(PG. 5) MAILING PANEL (PG. 6) FRONT COVER (PG. 1) HONORING OUR VOLUNTEERS NON PROFIT ORG DUTCHESS OUTREACH, INC. This year’s Volunteer Recognition Reception was US POSTAGE PAID held at The Manor at Woodside to recognize and thank the 29 NORTH HAMILTON ST., SUITE 220 NEWBURGH, NY generous efforts of Dutchess Outreach volunteers. POUGHKEEPSIE, NY 12601 Kathleen Dynes and Marie Dynes received the PERMIT NO. 405 Mary Keeley Award. Kathy and Mary, sisters, are our behind NEWS the scene volunteers helping to move food from the Letter Carriers Food Drive, loading and unloading the coat truck, sorting and bagging thousands of coats, and moving coats to The inaugural Taste Against Hunger was a 2015/2016 the various distribution sites. They never need to be asked. great success and a very enjoyable evening was had by We know they will be there to help. The Susan DeKeukelaere all who attended! Held on Friday, October 21, in the Caring Heart Award was presented to Jillian Brushini, Aula Room at Vassar College, we shared a wonderful Patrick Buddy, Michael Reap, and Charity Oyibl, their job and delicious array of foods from local Hudson Valley coach. Every Tuesday, they eagerly help sort and hang bags Restaurants, enjoyed the sweet a cappella sounds upon bags of clothing in the Children’s Clothes Closet. Divya Simplicity Kumar was recognized with the Outstanding Youth Award. of musical group ‘Cherished Memories’, all while She began volunteering in the Lunch Box ten years ago at the supporting our work and mission. We held very Since the Great Recession However, we the people understand our fellow habitants age of seven. -

1 MEGA DROP HIP HOP 83 Songs, 5:27:08 Total Time, 559.4 MB
#1 MEGA DROP HIP HOP 83 songs, 5:27:08 total time, 559.4 MB Name Time Album Artist If I Had You 3:48 For Your Entertainment (Deluxe Vers… Adam Lambert Gives You Hell 3:33 When the World Comes Down (Delux… The All-American Rejects Girlfriend 3:37 Girlfriend - Single Avril Lavigne Airplanes (feat. Hayley Williams of Pa… 3:01 Airplanes (feat. Hayley Williams of Pa… B.o.B Magic (feat. Rivers Cuomo) 3:16 B.o.B Presents: The Adventures of Bo… B.o.B Nothin' On You (feat. Bruno Mars) 4:30 Nothin' On You (feat. Bruno Mars) -… B.o.B The Time (Dirty Bit) 5:08 The Beginning (Deluxe Version) The Black Eyed Peas Just Can't Get Enough 3:39 The Beginning (Deluxe Version) The Black Eyed Peas Boom Boom Pow 4:12 Boom Boom Pow - Single Black Eyed Peas I Gotta Feeling 4:49 The E.N.D. (The Energy Never Dies) Black Eyed Peas Circus 3:12 Circus (Deluxe Version) Britney Spears Hold It Against Me 3:50 Hold It Against Me - Single Britney Spears Grenade 3:42 Doo-Wops & Hooligans (Deluxe Vers… Bruno Mars Just the Way You Are 3:41 Just the Way You Are - Single Bruno Mars Teach Me How to Dougie 4:00 Teach Me How to Dougie - EP Cali Swag District Evacuate the Dancefloor (Radio Edit) 3:30 Evacuate the Dancefloor Cascada ChaCha Slide (club mix) 7:43 Casper Forever 4:39 Forever - Single Chris Brown Jar of Hearts 4:07 Jar of Hearts - Single Christina Perri Good Girls Go Bad (feat. -
2017 a N N U a L R Eport
2 0 1 7 A NNU A L R EPO R T WHO WE ARE Dutchess Outreach acts as a catalyst for community revitalization and exists in Dutchess County as an advocate and provider of hunger and relief services in order to ensure that everyone, regardless of income, has access to fresh, healthy food, and the support they need. BOARD OF DIRECTORS OFFICERS Ann St. Germain, CHAIRPERSON Elizabeth DeFiglio, VICE CHAIR Rob Caso, TREASURER Carol Ferolito, SECRETARY DIRECTORS TODD BENDER EILEEN MILLER JAN DEWEY KERI I. PETERSON PETER F. DORO ROYAL RICCI SHANE EGAN, ESQ. BRANDI RIDER CHRISTINA KINNALLY JENNIFER SHEEHAN ROBIN KLEBAN CHRISTA ST. GERMAIN CAROL LALLY METZ BHARAT THAKKAR KATHERINE MANZI-DORO NICOLE TIPPA “The best way to find AMY K. WOODS yourself is to lose yourself DIRECTORS EMERITUS in the service of others.” Geraldo M.V. DePorres -MAHATMA GANDHI Roderick J. MacLeod, Esq. OUR TEAM Brian Riddell Delia Vasquez-Habib Atticus Lanigan EXECUTIVE DIRECTOR CASE MANAGER ADMINISTRATIVE ASSISTANT Tara Whalen Letitia Butler Kenya Grant ASSOCIATE DIRECTOR LUNCH BOX MANAGER LUNCH BOX ASSISTANT Sarah A. Salem Cloud Bartoli Rich Oszip DEVELOPMENT ASSOCIATE MOBILE MARKET MANAGER DISHWASHER Nyhisha T. Gibbs Kris Glover Teresa Brennan VOLUNTEER ADMINISTRATOR FARM ASSISTANT RECEPTIONIST COVER PHOTO AND ALL PHOTOS INCLUDED (UNLESS OTHERWISE NOTED): SEAN HEMMERLE 2017 A WORD FROM OUR EXECUTIVE DIRECTOR Brian Riddell Balancing Acts One often finds inspiration in the strangest of places. In a recent issue of ‘This Week’, a foodie writer described the impact of the blending of flavors in a savory chicken sandwich capable of “restoring balance to the universe.” Silly, you say? Merely the ravenous raving of an elite epicurean? Perhaps not; for food is energy and it does have the power to change things, for example, the ability to improve the potential of children to learn (Journal of Public Economics, April 1, 2015). -

Documentary on Sterilization of Hispanic Women I Have a Confession
35 YEARS of Publication 1976-2011 1976 2010 Vol. XXXI XXXVII No. 25 La Prensa Muñoz, Inc., Publications JUNE 24, 2011 The Afghan U.S. Men’s National Team to Face Mexico in Third Straight Gold Cup Final U.S. Will Face Mexico in Final on Saturday, June 25 at a Sold-Out Rose Bowl in Pasadena, Calif., Live at 9 p.m. ET on FOX Soccer and Univision The U.S. Men’s National Team ad- placed long ball to Donovan who was Drawdown Is vanced to an unprecedented fourth making a run down the right flank. straight CONCACAF Gold Cup fi- Donovan collected the ball near the nal in a 1-0 victory against Panama right corner of the penalty area, Long, Long at Reliant Stadium. The U.S. will face dribbled towards the goal and hitting Mexico for the third straight time in a low laser through four Panamanian the final after the USA’s archrival defenders to Dempsey who directed defeated Honduras in the second the ball into the net with his left foot Overdue semifinal. from two yards out. In a defensive match against The 2011 Gold Cup final will take Panama that didn’t see many chances place on Saturday, June 25 at a sold- PERSPECTIVE for either side, Clint Dempsey scored out Rose Bowl in Pasadena, Calif. his third goal of the 2011 Gold Cup in Kickoff for the match is set for 6 p.m. By William O. Beeman the 76th minute after a great service and the match can be seen live on NEW AMERICA MEDIA from Landon Donovan set him up for FOX Soccer and Univision. -

Brown Shoe's Footwear Collections with Music, Entertainment Superstar Fergie Debut in Stores for Spring
Published on Caleres Investor Center (https://investor.caleres.com) on Mar 17 2009 Brown Shoe's Footwear Collections with Music, Entertainment Superstar Fergie Debut in Stores for Spring Release Date: Tuesday, March 17, 2009 7:07 am CDT Terms: Dateline City: ST. LOUIS Consumers anticipating the arrival of Fergie's shoe collections since the 2008 announcement of her collaboration with Brown Shoe Company (NYSE: BWS, www.brownshoe.com) will wait no longer. Fergie(TM) and Fergalicious by Fergie(TM) footwear begin their spring launches today at select department stores and boutiques, national chains and online retailers. (Photo: http://www.newscom.com/cgi-bin/prnh/20090317/CG84644-a) (Photo: http://www.newscom.com/cgi-bin/prnh/20090317/CG84644-b) (Photo: http://www.newscom.com/cgi-bin/prnh/20090317/CG84644-c) "After months of working with the designers and watching ideas and sketches come to life, it's time for the fun part - wearing the shoes! Both lines capture the essence of my style, and I'm looking forward to the reactions as women begin seeing the shoes on the shelves and deciding which ones to add to their closets. I know I have quite a few pairs in mine!" said Fergie. Brown Shoe created two namesake footwear lines to fully capture the multi-faceted aspects of Fergie's life as an award- winning singer, songwriter and actress - from her on-stage kicks to her red carpet stilettos to her day-in-LA flats. Fergie footwear captures the multi-platinum artist's confident, individual style in a line of sophisticated, sexy footwear with a glam rock influence. -

Boardman Road Branch Library Opens April 12
NONPROFIT ORGANIZATION U.S. POSTAGE Th e PAID NEWBURGH, NY PERMIT #2290 Rotunda SPRING 2015 Vol. 15, Issue 3 P OUGHKEEP S IE P UBLIC L IBRARY D I S TRICT E XPLORE • D I S COVER • C ONNECT COMPUTER PRESCHOOLER TEEN CLASSES DE FREE! CLASSES LEARNING CENTER MEDIA LAB ESPANOL PAGE 3 INSERT, PAGE 2 INSERT, PAGE 4 PAGE 8 Boardman Road Branch Library Opens April 12 The story of Poughkeepsie’s public helped celebrate the reopening converted to a single large room libraries begins a new chapter of Adriance Memorial Library with a seating capacity of 125. The on April 12 when the Boardman in October 2009. The library is room features a professional audio Road Branch Library opens its at 141 Boardman Road, between system and devices to assist the Tom Chapin doors for the first time. With four Poughkeepsie Day School and Our hearing impaired. Children will to Perform at program rooms, 30 computers, Lady of Lourdes High School. have their own program room and and more than twice the space of 11 computers, while the teen area Opening the current branch, this beautiful The branch is designed to will feature six computers and new facility will significantly meet popular information and comfortable seating. The spacious The New York Times called increase the Library District’s recreational needs, with an adult property also offers landscaping Tom Chapin “one of the great capacity to serve the community. collection of popular fiction and possibilities, including a children’s personalities in contemporary folk music,” while The celebration will begin at 2 non-fiction books and a complete garden. -

OPERATION IMPACT Annual Report - 2013
Andrew M. Cuomo Governor Michael C. Green Executive Deputy Commissioner OPERATION IMPACT Annual Report - 2013 New York State Division of Criminal Justice Services 80 South Swan Street Albany, New York 12210 www.criminaljustice.ny.gov Table of Contents I. Introduction ..........................................................................................................................1 II. Operation IMPACT Funding .............................................................................................3 A. Award Process ...........................................................................................................3 B. Personnel ....................................................................................................................5 C. Initiatives....................................................................................................................5 D. Benefits of IMPACT Funding to Local Agencies .....................................................7 III. Partnership Highlights by County .....................................................................................7 IV. State Agency Contributions ................................................................................................29 V. Statistical Reports ............................................................................................... Appendix A I. INTRODUCTION The New York State Division of Criminal Justice Services (DCJS) implemented Operation IMPACT in 2004, targeting the 17 New York State counties that account -

Aimee Mann Aimee
it’s still chock full of lush harmony vocals and thoughtful pop songs (many of which were inspired by Mann’s split with Hausman). In truly bittersweet fashion, the album’s title track gave Mann her sole bona fide hit to date, hitting the upper echelons of the Billboard charts. Aimee Mann Aimee Welcome Home (Epic, 1986) For the second album, Mann began to assume much greater responsibility for the songwriting duties. This led to a sound that was clearly maturing from the first album’s dance-synth pop, providing a clear bridge to her later work whilst retaining an inescapably Eighties vibe. Standout tracks include Coming Up Close and the heartstoppingly beautiful No One Is Watching You Now. It may have been a commercial flop but Welcome Home is artistically sound. aimee manna buyer’s guide to reative force, campaigner for artists’ rights, bête-noir of record execs, Y YOU ‘TIL TUESDay filmmaker’s muse, professional cynic C…this doesn’t even come close to covering the Mann formed the Eighties post-new wave pop multifaceted talents and fractured career outfit ‘Til Tuesday in 1983 with fellow big- path of Virginian songstress Aimee Mann. haired alumni of Boston’s Berklee College of Despite a stop-start career spanning over Music, Michael Hausman (her then boyfriend), twenty years and more bad breaks than an Robert Holmes and Joey Pesce, and over the orthopaedic surgeon could shake a splint at, course of the next seven years produced three she’s amassed an impressive body of work under-appreciated albums. across a dozen or so albums. -

I Lived Experiences of Undocumented Latin@ Students
i Lived Experiences of Undocumented Latin@ Students: Phenomenological Research Study by Ricardo Pacheco Dissertation Submitted to the Doctoral Program of the American College of Education in partial fulfillment of the requirements for the degree of DOCTOR OF EDUCATION March 2021 ii Lived Experiences of Undocumented Latin@ Students: Phenomenological Research Study by Ricardo Pacheco Approved by: Dissertation Chair: Amanda Jandris, Ph.D. Committee Member: Krista Allison, Ph.D. iii Copyright © 2021 Ricardo Pacheco iv Abstract Undocumented Latin@ students face numerous life experiences. Economic, legal, and social difficulties are just a few examples affecting academic performance and potentially drop out of high school. The labeling as an undocumented Latin@ student increased the probability of nonparticipators in high school education, reducing college entry options, and societal rejection experiences. The qualitative, phenomenological research study explored the lived experiences of 20 undocumented Latin@ students. The aim was to address the connection between lived experiences of undocumented Latin@ students and the dropout rate in Lincolndale, New York. Latin@ is a term used in contemporary Latin culture to identify diverse Latinos as including gender-neutral members of the Latino community. The semi-structured interviews addressed the research questions of lived experiences and implementations for assisting undocumented Latin@ students. Various themes emerging from the data collection and analysis using MAXQDA are social-economic, sociocultural, family, school environment, religion, policy changes, economics, legal representation, communication, classes to fit goal objectives, bilingual teachers, college aspirations, and a sense of belonging. Collaborative initiatives between educators, support staff, parents/legal guardians can help undocumented Latin@ students achieve academic success. The research confirmed that life experiences of undocumented Latin@ students influence academic performance.