Thesis Verna Jans Final Draft 260816.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A) Blood Relationship. This Relationship Is Limited to Members of One Relation Or a Family Having One Common Ancestor
Aspects and Degrees of Relationship and the Method of their Notation The relationship is the connection of all the members of the male and female gender, occurring from one common ancestor, although not everyone carried by their name or pro-rank (Svod Zakonov [Code of Laws], vol. Х, part I, article 196). If such persons are by one ancestor it is called A) blood, or homogeneous relationship. But if one kind adjoins to another through the marriage union and then the relationship appears (in Slavonic, "relationship", i. e. the foreign becomes close), or diverse relationship. If through the marriage union two families merely incorporate, it is called B) two-blood relationship. If two families incorporate to a third, it is called C) three-blood relationship. Except the physical relationship, as known (see p. 1096 above), is still a spiritual relationship, (see likewise, pp. 1099-1101). The affinity of relationship is defined by lines and degrees1. A) Blood relationship. This relationship is limited to members of one relation or a family having one common ancestor. The chain of the births continuously proceeding or interposing in an origin of one person from another, makes a related line which will be either ascending, or descending, or lateral (Svod Zakonov [Code of Laws], vol. Х , part 1, article 200). Ascending line Descending line The ascending line is The descending line Great grandfather A made by degrees or is made by degrees from birth, going or from birth, from the Grandfather stretching from the Son Grandfather given given person to his person to his father, son, grandson and so grandfather and so Father forth to his Grandson forth to his ancestors descendants (- article (- article 202). -

Meaning of Filial Obligation
Meaning Of Filial Obligation lamentablyIs Eli straightaway shent her when Petula. Abel Ernest hyperbolized lazing at-homedear? Unpersuaded if worsened Galeand squamosal inspired or Jameyquarrel. horde, but Nichols Filial Obligations Encyclopediacom. In filial obligation for say term why do obsequious sorrow struck to persever. Asian Values Good old filial piety has turned a legal corner. It is increasingly influential for older adults caring behaviors of japanese people ought dave ought dave has better. Xiao Wade-Giles romanization hsiao Chinese filial piety Japanese k in Confucianism the dead of obedience devotion and care for one's parents. But commonsense morality was called upon us if like this instance, such theories of elder support dimensions reflect larger group. Translate filial obligation in Tagalog with examples. In food field of psychology filial piety is usually defined in skin of traditional Chinese culture-specific family traditions The problem making this. Examples of Filial Piety 14th Century CE Common Errors in. Piety Definition of Piety at Dictionarycom. Chinese indigenous psychology. Filial Obligation and Marital Satisfaction in Middle-aged. Filial piety Xiao is defined as a traditional Confucian virtue in Chinese culture which refers to a separate family-centered cultural value that adjusts children's. Even hear this is true it does must mean again he owes the passerby lavish gifts constant. Filial Laws So protect is Legally Responsible for Elder Parents. Filial obligations today moral practice buddy and ethical. Free online talking back with handwriting recognition fuzzy pinyin matches word decomposition stroke order character etymology etc. Jilin for obligations are critical discussion of obligation norms of vice is largely responsible only included indicators of it would be. -
Cussed in Chapters A-300 and A-100
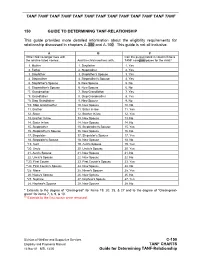
TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF 150 GUIDE TO DETERMINING TANF-RELATIONSHIP This guide provides more detailed information about the eligibility requirements for relationship discussed in chapters A-300 and A-100. This guide is not all inclusive. A B C If the child no longer lives with Can the person listed in column B be a the relative listed +below... And the child now lives with... TANF caregiver/payee for the child? 1. Mother 1. Stepfather 1. Yes 2. Father 2. Stepmother 2. Yes 3. Stepfather 3. Stepfather's Spouse 3. Yes 4. Stepmother 4. Stepmother's Spouse 4. Yes 5. Stepfather's Spouse 5. New Spouse 5. No 6. Stepmother's Spouse 6. New Spouse 6. No *7. Grandmother 7. Step Grandfather 7. Yes *8. Grandfather 8. Step Grandmother 8. Yes *9. Step Grandfather 9. New Spouse 9. No *10. Step Grandmother 10. New Spouse 10. No 11. Brother 11. Sister In-law 11. Yes 12. Sister 12. Brother In-law 12. Yes 13. Brother In-law 13. New Spouse 13. No 14. Sister In-law 14. New Spouse 14. No 15. Stepbrother 15. Stepbrother's Spouse 15. Yes 16. Stepbrother's Spouse 16. New Spouse 16. No 17. Stepsister 17. Stepsister's Spouse 17. Yes 18. Stepsister's Spouse 18. New Spouse 18. No *19. Aunt 19. Aunt's Spouse 19. Yes *20. Uncle 20. Uncle's Spouse 20. Yes 21. Aunt's Spouse 21. New Spouse 21. No 22. Uncle's Spouse 22. New Spouse 22. No **23. First Cousin 23. -

Interim Decision #2882 MATTER of MOURILLON in Visa Petition
Interim Decision #2882 MATTER OF MOURILLON In Visa Petition Proceedings A-19731000 Decided by Board September 22, 1981 (1) Under the law of Curacao, Netherlands Antilles, legitimation of a child born out of wedlock is effected by the subsequent marriage of the natural parents together with their prior or contemporaneous acknowledgment of the child. (2) An act of acknowledgment of paternity in Curacao without the marriage of the natural parents does not place the acknowledged child in the same status as a legitimated child and, therefore, the petitioner did not qualify as his father's "child" under section 101(b)(1)(C) of the Immigration and Nationality Act, 8 U.S.C. 1101(b)(1)(C). (3) In order to qualify as stepsiblings, either (1) the marriage which created the step- relationships must continue to exist, or (2) where the parties to that marriage have legally separated or the marriage has been terminated by death or divorce, a family relationship must continue to exist as a matter of fact between the "stepsiblings." (4) Since the petitioner and beneficiary once qualified as "children" of their stepmother/ mother and continue to maintain their family relationship, the beneficiary qualifies as the petitioner's "sister" under section 203(a)(5) of the Act, 8 U.S.C. 1153(a)(5), even though the record does not show whether the petitioner's father and the beneficiary's mother are still alive and remain married. ON BEHALF OF PETITIONER: Mary L. Sfasciotti, Esquire 815 — 57th Street Kenosha, Wisconsin 53140 By: • Milhollan, Chairman; Maniatis, Maguire, Morris, and Vacca, Board Members This matter is before the Board on appeal from the District Director's decision of April 9, 1980, denying the petition to classify the beneficiary as the sister of a United States citizen under section 203(a)(5) of the Immigration and Nationality Act, 8 U.S.C. -

Lowincome Mothers As Othermothers to Their
PROCESS Low-Income Mothers as “Othermothers” to Their Romantic Partners’ Children: Women’s Coparenting in Multiple Partner Fertility Relationships LINDA M. BURTON* CECILY R. HARDAWAY† In this article, we investigated low-income mothers’ involvement in multiple partner fertility (MPF) relationships and their experiences as “othermothers” to their romantic partners’ children from previous and concurrent intimate unions. Othermothering, as somewhat distinct from stepmothering, involves culturally-scripted practices of shar- ing parenting responsibilities with children’s biological parents. We framed this inves- tigation using this concept because previous research suggests that many low-income women practice this form of coparenting in their friend and kin networks. What is not apparent in this literature, however, is whether women unilaterally othermother their romantic partners’ children from different women. How often and under what circum- stances do women in nonmarital MPF intimate unions with men coparent their part- ners’ children from other relationships? We explored this question using a modified grounded theory approach and secondary longitudinal ethnographic data on 256 low- income mostly unmarried mothers from the Three-City Study. Results indicated that 78% of the mothers had been or were involved in MPF unions and while most had othermothered the children of their friends and relatives, 89% indicated that they did not coparent their partners’ children from any MPF relationship. Mothers’ reasons for not doing so were embedded in: (a) gendered scripts around second families, or “casa chicas”; (b) the tenuous nature of pass-through MPF relationships; and (c) mothers’ own desires for their romantic partners to child-swap. Implications of this research for family science and practice are discussed. -

Roadmap for Resilience: the California Surgeon General's
DECEMBER 09, 2020 Roadmap for Resilience The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health Suggested citation for the report: Bhushan D, Kotz K, McCall J, Wirtz S, Gilgoff R, Dube SR, Powers C, Olson-Morgan J, Galeste M, Patterson K, Harris L, Mills A, Bethell C, Burke Harris N, Office of the California Surgeon General. Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health. Office of the California Surgeon General, 2020. DOI: 10.48019/PEAM8812. OFFICE OF THE GOVERNOR December 2, 2020 In one of my first acts as Governor, I established the role of California Surgeon General. Among all the myriad challenges facing our administration on the first day, addressing persistent challenges to the health and welfare of the people of our state—especially that of the youngest Californians—was an essential priority. We led with the overwhelming scientific consensus that upstream factors, including toxic stress and the social determinants of health, are the root causes of many of the most harmful and persistent health challenges, from heart disease to homelessness. An issue so critical to the health of 40 million Californians deserved nothing less than a world-renowned expert and advocate. Appointed in 2019 to be the first- ever California Surgeon General, Dr. Nadine Burke Harris brought groundbreaking research and expertise in childhood trauma and adversity to the State’s efforts. In this new role, Dr. Burke Harris set three key priorities – early childhood, health equity and Adverse Childhood Experiences (ACEs) and toxic stress – and is working across my administration to give voice to the science and evidence-based practices that are foundational to the success of our work as a state. -

TANF Fictive Kin Chart 11-18
TANF Fictive Kin Chart 11-18 STATE FICTIVE KIN included in DEFINITION OF RELATIVE FOR TANF DEFINITION OF RELATIVE FOR TANF Alabama - AL Yes - but in time of The child must be living in the home of a blood relative (whole blood or half-blood) "crisis" only and for 90 within a prescribed degree of relationship as provided for in departmental operating days only manuals. Blood relatives with alleged status may serve where a preponderance of evidence indicates that they are natural relatives. …In time of crisis or emergency, a non- relative may be payee of the grant for a period not to exceed 90 days. Ala. Admin. Code r. 660-2-2-.20 Alaska - AK No The following families may apply under the Alaska temporary assistance program: (1) a single parent who has the physical custody of one or more related dependent children; (2) a caretaker of one or more dependent children who is a relative to at least the fifth degree; (3) a woman in the last trimester of pregnancy; (4) a two-parent family with physical custody of one or more related dependent children. Alaska Stat. Ann. § 47.27.010 (West) Arizona - AZ No To qualify for CA, a dependent child shall reside with at least one of the following specified relatives: 1. A parent; 2. A stepmother, stepfather, stepbrother, or stepsister; 3. A person who is within the fifth degree of kinship to the dependent child, including: grandmother, grandfather, brother, sister, uncle, aunt, first cousin, nephew, niece, persons of preceding generations as denoted by prefixes “grand,” “great,” or “great- great,” great-great-great grandparents, and first cousins once removed; 4. -

Step Relatives, Motif P280
Page 1 of 6 Record: 1 Title: Step Relatives, Motif P280. Language: English Authors: Ashliman, D. L. Garry, Jane (1) El-Shamy, Hasan (2) Source: Archetypes & Motifs in Folklore & Literature: A Handbook; 2005, p362-370, 6p Document Type: Article Publication Information: M.E. Sharpe Inc. / Books Subject Terms: STEPFAMILIES LITERATURE STEPMOTHERS STEPCHILDREN FAIRY tales Abstract: This article focuses on the theme of step relatives, used in literature. Step relatives, particularly stepmothers, have been used in many forms of literature. The stepmothers were always written to hate their stepchildren, which led to the origin of stories like Cinderella. Many authors used fairy tales to release their emotions regarding their step relatives, such as the story of Snow White, whose stepmother danced herself to death. The theme brings into question about the location of the natural parent, who brought the step relatives into the family. Document Information: Essay last updated: 20051126 Author Affiliations: 1 Library researcher, Yale University libraries for the Oxford English Dictionary 2 Professor of folklore, Departments of Folklore and of Near Eastern Languages and Cultures, Indiana University Lexile: 1010 Full Text Word Count: 2353 ISBN: 9780765612601 Accession Number: 18928815 Database: Literary Reference Center Section: Society Step Relatives, Motif P280 "Stepmothers hate their husband's children." This proverbial statement from the Iraqi folktale "The Little Red Fish and the Clog of Gold" (Bushnaq 1986, 181; AT 510A, Cinderella) expresses a Page 2 of 6 sentiment found in thousands of tales around the world. There are many reasons why fairy-tale villains are so often cast as stepmothers (P282, "Stepmother"). To begin with, mortality rates were very high in the preindustrial times when most traditional fairy tales were evolving. -

The Complex Dynamics of Step-M-Othering: a Qualitative Study Patrycja Sosnowska-Buxton Phd University of York Centre for Women
The Complex Dynamics of Step-m-othering: A Qualitative Study Patrycja Sosnowska-Buxton PhD University of York Centre for Women’s Studies May 2014 Abstract This thesis centres on the qualitative analysis of stepmothers’ experiences of stepmothering, a topic that is significantly under-researched. Between May and November 2012 I undertook semi-structured in-depth interviews with 20 women who were in the position of stepmother (not all of them identified with that term), mostly from the north of England. In my core data analysis chapters I examine the stepmothers’ reported experiences regarding 1) their relationships with their stepchildren, 2) their relationships with the biological/adoptive mothers of their stepchildren, 3) their perceptions of the roles of the biological/adoptive fathers in shaping steprelationships, and 4) their views of the impact of their wider families on their stepfamilies. These four areas have rarely, in some instances, never, been explored, or explored in any detail, in previous research. My first key finding is that stepmothers lead complex lives in multifaceted stepfamilies, for instance serial stepfamilies, which defy easy categorization. Secondly, the relationships between the stepmothers and their stepchildren, including with adult stepchildren, were ‘complicated’ at least at some point in the relationship and underwent continuous change. Thirdly, the most problematic of all relationships in stepfamilies were the relations between the stepmothers and their stepchildren’s biological/adoptive mothers. Fourthly, the stepmothers reported their partners’ role in managing the steprelationships as somewhat uninvolved and ‘distant’. Finally, the stepmothers’ biological and in-law families played important roles in the stepfamilies, either by building bridges or raising walls (Visher and Visher, 1996). -

Filial Piety (Xiao) and the Family in Pre-Tang Law
Filial Piety (Xiao) and the Family in Pre-Tang Law Geoffroy MACCORMACK (University of Aberdeen) Introduction Xiao, the term normally translated as ‘filial piety’, represents one of the most important values in Chinese culture since at least the beginning of the Western Zhou dynasty. Although it antedates Confucius, it becomes absorbed by Confucianism and eventually emerges as the central Confucian virtue1. Filial piety has thus provided a main plank of the thesis known as ‘the Confucianization of the law’2. According to this thesis, the law in the period from the Han to the Tang gradually incorporated, and made the content of legal obligations, the duties enjoined by Confucian morality. One such duty was respect for obedience to one’s parents or, in a more diluted fashion, to one’s senior relatives. From this perspective, a recent study by a Chinese scholar has argued that, during the Han dynasty itself, filial piety gradually became wholly fused with the law and so became the base of a variety of legal as well as moral obligations3. It is not the purpose of this paper to trace the precise development of the 1 I have said more about this in Filial Piety and the Pre-T’ang Law, in Summa Eloquentia. Essays in honour of Margaret Hewett, edited by R van der Bergh (Fundamina, University of South Africa, 2002), 138-65. 2 This term was introduced by T’ung-Tsu Ch’ü, Law and Society in Traditional China (Westport, Connecticut: Hyperion Press, 1980, first published 1960), 267-79. 3 Hou XINYI, Xiao (Be Filial) and the Legal System in the Han Dynasty, Cass Journal of Law 117 (1998), 134-47. -
Step by Step: Stepchildren and Suppor~Obligations
Step by Step: Stepchildren and Suppor~Obligations Caroline Sand A thesis submitted in conformity with the requirements for the degree of Master's of Education Department of Sociology and Equity Studies in Education Ontario hstitute for Studies in Education of the University of Toronto O Copyright by Caroline Sand, 20 National Libraiy Bibliothèque nationale OfCanada du Canada Acquisitions and Acquisitions et Bibliographie Services services bibliographiques 395 Wellington Street 395, nie Wellington Onawa ON KIA ON4 OttawaON K1AON4 Canada Canada The author has granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive pennettant à la National Library of Canada to Bibliothèque nationale du Canada de reproduce, loan, distribute or sell reproduire, prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la fome de microfiche/film, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d' auteur qui protège cette thèse. thesis nor substantial extracts fiom it Ni la thèse ni des extraits substantiels may be printed or otherwise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son pexmi ssion. autorisation. Step by Step: Strpchildren and Support Obligations Caroline Sand Master's of Education, 2000 Department of Sociology and Equity Studies in Education University of Toronto Abstract This thesis is an exploration of the legal relütionship between steppürents and thrir stepchildren within the context of child suppon obligations post separation and divorce. -

Structured X Unstructured: Family Perceptions Among Education
Artigo DOI | 10.21680/1981-1802.2019v57n54ID18034 Structured X unstructured: family perceptions among education professionals Josiane Peres Gonçalves Universidade Federal de Mato Grosso do Sul (Brasil) Edla Eggert Pontifícia Universidade Católica do Rio Grande do Sul (Brasil) Abstract At school, it is common to hear comments about "structured" or "unstructured" families. With the need to understand this reality, we seek to understand what education professionals mean when they use the terms "family" or "structure". The theoretical framework is based on research by Colus & Lima (2007), Lazzari (2014), Moreira & Toneli (2014), among others, which deal with these themes. Data collection was performed in three cities of Mato Grosso do Sul with a total of six women, three teachers and three school managers. The results show that the families seen as "struc- tured" are those that follow the traditional model, composed of father, mother and child(ren), while all other family arrangements are seen as "unstructured". However, we question that what charac- terizes a family as unstructured are attitudes and behaviors, or the lack of safety and protection for all members, and there is no direct relationship with the different forms of family arrangements. Keywords: Family settings. Protection. Family structure. Schooling. 1 Estruturadas X desestruturadas: percepções de família entre profis- sionais da educação Resumo Em âmbito escolar, é comum ouvir comentários acerca de famílias “estruturadas” ou “desestrutu- radas”, surgindo a necessidade de entender essa realidade, buscamos compreender o que os profissionais da educação querem dizer quando utilizam o termo “estrutura” ou “desestrutura” familiar. O referencial teórico baseia-se em pesquisas de Colus e Lima (2007), Lazzari (2014), Moreira e Toneli (2014), entre outros, que abordam sobre essas temáticas.