2018 Cuyahoga County Community Health Assessment/Chna
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Adjunct-Faculty-Reference-Guide
D J U N C T F A C U L T Y R E F E R E N C E G U I D E i VISION 2020 PRIORITY 1 Student completion for academic and career success is the first priority of Lorain County Community College’s strategic vision, Vision 2020. LCCC’s focus on student success is part of a national effort that includes LCCC students, faculty and staff, community members, partner institutions and educational partners across the country. Supporting LCCC’s Priority 1 are the following strategies and interventions: Reduce Time and Cost to Completion Blend Educational Continuum to reduce the time and cost to earn a degree or credential (i.e., Early College High School, MyUniversity, University Partnership, Competency- Based Education, Prior Learning Assessment). Coach Every Student for Success Wrap personalized intervention and coaching strategies around every student to map pathway to success to achieve goals. Improve College Readiness Minimize the need for developmental education by partnering with secondary schools; Launch new designs and delivery models to accelerate progression based on students’ needs and abilities. Enhance Student Learning Leverage innovative teaching models, adaptive learning technologies, contextualized learning and different delivery methods to help meet diverse student learning needs. Develop Structured Pathways to In-Demand Careers and Employers Raise awareness of in-demand careers, related educational programs, help students identify and persist in a career pathway that includes real-world experience and connection to employers with jobs. Engage More Adult Learners Develop programs, services and outreach services and delivery models that engage more adult learners in our community. -
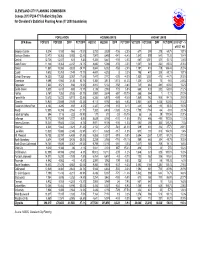
Census 2010 PL94-171 Redistricting Data for Cleveland's Statistical Planning Areas (Yr 2000 Boundaries)
CLEVELAND CITY PLANNING COMMISSION Census 2010 PL94-171 Redistricting Data for Cleveland's Statistical Planning Areas (Yr 2000 boundaries) POPULATION HOUSING UNITS VACANT UNITS SPA Name POP2010 POP2000 DIFF PCT DIFF HU2010 HU2000 DIFF PCT DIFF VCT2010 VCT2000 DIFF PCT DIFF 2010 VCT - % of TOT HU Brooklyn Centre 8,214 9,180 -966 -10.5% 3,733 3,839 -106 -2.8% 677 399 278 69.7% 18.1% Buckeye-Shaker 12,470 16,063 -3,593 -22.4% 7,947 8,488 -541 -6.4% 1,540 899 641 71.3% 19.4% Central 12,738 12,107 631 5.2% 5,306 5,441 -135 -2.5% 680 1,001 -321 -32.1% 12.8% Clark-Fulton 11,126 13,363 -2,237 -16.7% 4,890 5,066 -176 -3.5% 1,007 543 464 85.5% 20.6% Corlett 11,581 15,384 -3,803 -24.7% 5,844 6,002 -158 -2.6% 1,197 418 779 186.4% 20.5% Cudell 9,612 10,761 -1,149 -10.7% 4,401 4,393 8 0.2% 795 470 325 69.1% 18.1% Detroit-Shoreway 14,325 17,382 -3,057 -17.6% 7,447 7,772 -325 -4.2% 1,530 1,057 473 44.7% 20.5% Downtown 9,098 5,960 3,138 52.7% 5,386 3,813 1,573 41.3% 1,325 1,255 70 5.6% 24.6% Edgewater 7,633 8,571 -938 -10.9% 4,910 5,102 -192 -3.8% 745 464 281 60.6% 15.2% Euclid-Green 5,533 6,413 -880 -13.7% 3,136 2,963 173 5.8% 665 433 232 53.6% 21.2% Fairfax 5,167 7,352 -2,185 -29.7% 2,987 3,674 -687 -18.7% 865 864 1 0.1% 29.0% Forest Hills 10,612 15,723 -5,111 -32.5% 6,306 6,875 -569 -8.3% 1,869 963 906 94.1% 29.6% Glenville 15,940 23,559 -7,619 -32.3% 9,112 9,792 -680 -6.9% 2,861 1,405 1,456 103.6% 31.4% Goodrich-Kirtland Park 4,103 4,295 -192 -4.5% 2,327 2,194 133 6.1% 441 326 115 35.3% 19.0% Hough 12,805 16,359 -3,554 -21.7% 7,382 8,408 -1,026 -12.2% 1,700 1,764 -64 -3.6% 23.0% Industrial Valley 894 1,116 -222 -19.9% 177 210 -33 -15.7% 55 26 29 111.5% 31.1% Jefferson 18,172 19,949 -1,777 -8.9% 8,629 8,760 -131 -1.5% 976 486 490 100.8% 11.3% Kamms Corners 18,241 19,545 -1,304 -6.7% 8,971 9,106 -135 -1.5% 653 290 363 125.2% 7.3% Kinsman 4,021 5,842 -1,821 -31.2% 2,154 2,737 -583 -21.3% 519 631 -112 -17.7% 24.1% Lee-Miles 13,820 15,866 -2,046 -12.9% 6,511 6,628 -117 -1.8% 613 300 313 104.3% 9.4% Mt. -

Cleveland Clinic Main Campus
2013 Community Health Needs Assessment – Cleveland Clinic Main Campus Founded in 1921, Cleveland Clinic is an academic medical center offering patient care services supported by research and education in a nonprofit group practice setting. More than 3,000 Cleveland Clinic staff physicians and scientists in 120 medical specialties care for more than 5 million patients across the system. Patients come to Cleveland Clinic locally, from all 50 states and from more than 132 nations around the world. Cleveland Clinic’s main campus, located in midtown Cleveland, includes a hospital with 1,288 staffed beds; an outpatient clinic; a medical school; a research institute; 26 specialty institutes; and supporting labs and facilities in 46 buildings on 167 acres. Cleveland Clinic patients represent the highest CMS case-mix index in the nation. Comprehensive services include heart care, digestive disease, nephrology and urology, cancer, neurology, diabetes and endocrinology, otolaryngology (ENT), rheumatology, gynecology, orthopaedics and pulmonology. Cleveland Clinic’s health system in Northeast Ohio consists of an academic medical center, two children’s hospitals and eight community hospitals. Each hospital is dedicated to the communi- ties it serves. We verify the health needs of our communities by performing periodic community health needs assessments (CHNAs). These formal assessments are analyzed using widely accepted criteria to determine and measure the health needs of a specific community. In accordance with Internal Revenue Code Section 501(r)(3), each hospital has conducted its own community health needs assessment. Upon review of all of the community health needs assessments for all of our Northeast Ohio facilities, Cleveland Clinic has identified five community health needs that are present in the ma- jority of hospital communities we serve. -
Coping During COVID 19
Coping During COVID 19 Your Cleveland Clinic social work team wishes the best for you and your family. COVID 19 has impacted all of our lives in one way or another. Here are some resources to ease your mind during this time. FINANCIAL Fortunately, there are available financial resources at this time. These links provide more information regarding the qualifications. Child Care Resources Cuyahoga County-ONLINE ONLY: https://docs.google.com/forms/d/e/1FAIpQLSd8-xY8s9lMQL09fdWsmWy6jeWMmv0FC- tnvVGer0Hn5Pmoug/viewform The USBG financial assistance for those employed through the hospitality industry link: https://www.usbgfoundation.org/beap USBG National Charity Foundation 2654 W Horizon Ridge Parkway Suite B5 PMB 252 Henderson, NV 89052-2803 855.655.8724 General information about Mayor Frank Jackson’s decision to maintain utilities in Cleveland-ONLINE ONLY: https://www.clevescene.com/scene-and-heard/archives/2020/03/13/city-of-cleveland-to-halt-water- and-power-shutoffs-restore- connections?fbclid=IwAR2puC3YNkx2KImyFbDZzA3HllAZpAyS885TOQ4u2zIcfENL4JSO5LPgF_8 Utility information by service provider: Dominion https://www.dominionenergy.com/company/coronavirus First Energy https://www.firstenergycorp.com/newsroom/news_articles/firstenergy-committed-to-maintaining-24- 7-service-to-customers-t.html Cleveland water http://www.clevelandwater.com/blog/how-were-addressing-covid-19-cleveland-water Interest Free loan for businesses through HMLA. Their mission statement and link for the application: https://interestfree.org/coronavirus-covid-19-emergency-fund-press- -

Cleveland Clinic Regional Hospitals EMS Protocols
VERSION: 5.0.2018 : JULY 2018 DOCUMENT NAVIGATION If viewing this document as a printed hard copy The Header color of each section defines the protocol type Introduction Blue – Adult Protocols Pink – Pediatric Purple – OB Emergencies Gray – Reference or Policy If viewing this document as portable document file (PDF with Adobe Reader) This document is hyperlinked for easy navigation in Adobe Reader. The colored boxes in each protocol tree are linked to the respective pages with further information on the specific procedure, medication, or protocol page. There is an active link when hovering over the text within the colored box and the cursor changes from a bar to a pointer finger. Left clicking will jump to the linked page containing further information. Right clicking and selecting “Previous View” will return you to the page you started at. This document is also bookmarked with respect to the individual sections. Use the book mark feature of Adobe Acrobat to display pre-designated bookmarks and click on each to jump between sections. PROTOCOL REVISION CHANGE LOG PROTOCOL VERSION CHANGE LOG Complete revision and reformatting of current 1.0.2017: January 2017 2014 Cleveland Clinic EMS Protocols and other DRAFT supportive documentation. Draft Revision Draft edits completed on content up to and 2.0.2017: January 2017 including Adult Medical Protocol section. DRAFT EDITS Completed Edits completed and reviewed by committee. All 3.0.2017: March 2017 sections compiled and combined into one (1) FINAL COPY PDF document. Hyperlinks to be completed. Finals last minute edits made. Protocol finalized 4.0.2017: April 2017 and approved. -

2016 Annual Report
FROM PROMISE TO PROGRESS METROHEALTH’S GROUNDBREAKING COMMITMENT TO THE COMMUNITY THE METROHEALTH SYSTEM 2016 ANNUAL REPORT CHANGE IS HEALTHY OUR MISSION Leading the way to a healthier you and a healthier community through service, teaching, discovery and teamwork. 3 2016 ANNUAL REPORT TABLE OF CONTENTS Message from the CEO 6 Oscar Hispanic Clinic 28 Finances 8 Prentiss Wellness Nursery at Providence House 28 Community Benefit 9 Pride Clinic 28 SANE 28 Statistical Highlights 10 School Health Program 29 Employee Numbers 11 Several Additional Programs with Cuyahoga County 29 Locations 12 Tuberculosis Clinic 29 Fulfilling our Mission 14 Young Adult Clinic 29 Infant Mortality 14 Patient Education and Support 30 Opioids 15 AA 31 Education 16 Adult Burn Survivor Recovery Group 31 Nutrition 17 Boot Camp for New Dads 32 Transformation 18 Breastfeeding Clinic 32 Community Programs 20 Childbirth Preparation Classes 32 Clinical Programs 22 Compass Services 32 Burn Music Therapy 23 Cuyahoga County Public Library at MetroHealth 33 Care Alliance 23 Medical Center Clinics in Discount Drug Marts 23 Cuyahoga County Women, Infants, and 33 Children (WIC) Program Community Advocacy Program (CAP) 24 Diabetes Self-Management Program 33 Comprehensive Care Practice 24 Doula Volunteer Program 33 Cuyahoga Health Access Partnership (CHAP) 24 Healing Hearts 34 Health Care at the Juvenile Detention Center 24 Language Access and Communication 34 Kidz Pride Clinic 24 Services Center MDA Care Center 25 Library Cards for Newborns 34 Medicaid Technical Assistance and 25 -
Communities at the Crossroads: a Survey of Five First-Ring Suburbs
S ource: Cuyahoga County Pictometry® COMMUNITIES COMMUNITIES at the CROSSROADS at the CROSSROADS A Survey of Five First-Ring Suburbs 2017 PrOPERTY SURVEY Euclid | GarfiELD HEIGHTs | MaplE HEIGHTS SOUTH Euclid | WARRENSVILLE HEIGHTS Contents 01 INTRODUCTION ............................................................................... 1 02 EXECUTIVE SUMMARY ..............................................................3 03 ABOUT the SURVEY ....................................................................... 6 04 DECISION SUPPORT TOOLS .................................................. 10 05 REAL ESTATE MARKET TRENDS ........................................14 06 IMPACTS of DEMOLITION & REHABiliTATION .....26 07 COMMUNITY CONDITIONS ................................................. 32 Euclid .....................................................................................................38 Garfield Heights ..............................................................................50 Maple Heights ...................................................................................62 South Euclid .......................................................................................74 Warrensville Heights ...................................................................88 08 GROWING GREENER ...............................................................100 09 SUBURBAN FUTURES ...............................................................105 10 ACTION AGENDA for FIRST-RING SUBURBS ...........109 Further Reading ..............................................................................115 -

Download Press Release
CONGRATULATIONS DavidAasefEmilyRobertMetroHealth’s Cunningham, Shaikh, Graczyk, Kirsch, MD, PhD PhD PhD PhD LeadsResearchOld InternationalAssistant BrooklynFeatured Assistant Professor Team Campus In Professor to of Create DepartmentPhysicalGuidelines Medicine$9M of on Biomedical RenovationsHow and to BestRehabilitation Engineering Virtually Assess Dizziness Case WesternMetroHealth Reserve System University Case Western Reserve School of Medicine “Miracles happen every day with our rehabilitation patients, who re-learn how to walk, Thetalk and Brain live their Implants lives The Cleveland FES Center congratulates David after traumatic events. This Cunningham, PhD on the appointment of Assistant investmentThat in our Old Could Brooklyn Change Professor in the Department of Physical Medicine & Campus will allow us to strengthen Rehabilitation (PM&R) at the MetroHealth System and these rehabilitation Humanity.programs and Case Western Reserve University School of Medicine. better serve our patients.” Brains are talking to computers,Dr. andCunningham’s research is focused on improving Akramcomputers Boutros, MD to brains. Are ourrehabilitative outcomes for patients with chronic MetroHealth Presidentdaydreams and CEO safe? post-stroke hemiplegia by employing methods of non-invasive brain stimulation (repetitive transcranial magnetic stimulation and transcranial direct current The Cleveland FES Center congratulatesstimulation). Emily Graczyk, PhD on her recent appointment of AasefResearch Shaikh, Assistant MD, PhD, Professor the Penni in the -

Akron General Medical Center, Goodwill Industries, and the Canton Repository
2011 Stark County Collaborative Poll Prepared for: Stark County Health Needs Assessment Committee Prepared by: The Center for Marketing and Opinion Research (CMOR) www.CMOResearch.com (330) 564-4211 Office Research Funded by: TABLE OF CONTENTS Page Executive Summary 3 Survey Questions 11 Survey Results 14 Overall needs and health 14 General health 19 Access to care 21 Exercise 29 Smoking/tobacco, alcohol, and prescription drug use 32 Obesity and access to healthy food 42 Immunizations 49 Texting and driving 52 APPENDIX A: Survey Results by Race 54 APPENDIX B: Survey Results by Location 66 APPENDIX C: Survey Results by Income 70 APPENDIX D: Quality of Life 74 APPENDIX E: Demographic Information 83 APPENDIX F: Research Methodology 104 2 Center for Marketing and Opinion Research 2011 Stark Poll- Stark County Health Needs Assessment Executive Summary The Stark County Health Needs Assessment Committee asked a series of questions as part of the 2011 Stark County Health Needs Assessment on the Stark County Collaborative Poll. The Stark County Health Needs Assessment Committee’s involvement with the 2011 Stark Poll was funded by Alliance Community Hospital, Aultman Health Foundation, and Mercy Medical Center and was coordinated by the Stark County Health Department. The questions focused on the following areas: overall needs and health, general physical and mental health, access to care, immunizations, smoking and tobacco use, alcohol consumption, prescription medication abuse, obesity and access to healthy food, exercise and texting while driving. Where possible, comparative data from previous Stark Poll administrations are included throughout the analysis. Overall Needs and Health First, all respondents were asked what they thought was the greatest unmet health need in Stark County. -

Brooklyn YMCA to Close; Building to Be Sold
28 YEARS OF SERVING THE COMMUNITY OldOld BrooklynBrooklyn NewsNews A Publication of the Old Brooklyn Community Development Corporation, Cleveland, Ohio www.oldbrooklyn.com June 2006, Volume 28 Number 4 Brooklyn YMCA to close; building to be sold by Sheila Long No. It’s a done deal. We have long-time [email protected] employees — Debbie Natal at the desk; she’s been here for ten years. She sat at the table and said, `This isn’t a job; this is part of After a half century of service to my family.’ What do you say to her? I have Brooklyn Centre, Old Brooklyn and sur- been a member for 34 years.” rounding neighborhoods, the Brooklyn Despite Boester’s obvious shock and YMCA on Pearl Road will be closing its concern, he acknowledged that Haley’s doors and put on the market for sale. assessments of the financial forecast for the Glenn Haley, the president and CEO of the Brooklyn Y were grim and somewhat com- YMCA of Greater Cleveland made the pelling. public announcement on Tuesday, May 30. “In terms of a membership,” Haley The Downtown YMCA also will be said. “You have a 60,600 square-foot facili- placed up for private sale but will continue ty that has 519 membership units. To main- as a membership branch in a contingency tain the organization and the operations, the of sale lessee relationship with the buyer. Brooklyn Y would need 2200-2500 mem- In a May 30 letter to the Brooklyn Y’s bership units just to sustain it. Over the last membership (the first notice that members Photo by Sandy Worona two years, we’ve got it up by barely 100 and received of any potential closure), Haley that is not sufficient.” wrote: In 1919, Karl Kist founded the Brooklyn branch of the YMCA; its first home was a second- floor office (with one phone) at 4145 Pearl Road shared with the YWCA and the editor of the Fiscal woes have plagued the YMCA of “The Brooklyn YMCA will be placed Brooklyn News. -

TURKEY APPEALS to POWERS Iiilhhn
Sf From Ban Frantlscol uood Is Wllhilmlim .. Odnb.r S One essential of a.lverllilno Tar Ben Franclseol persistency. by advertising can D merchant Hiitinliiliiti . (Ktnlnr 3 Only From Vancouver. secure wide distribution. Evening Only with wide distribution can h October II Btjbletin Mukurii For Vancouverl maintain low priets and hold the trade. 'hi In ml In OrtnberJ2 3:30 EDITION Publicity Is Purely a Matter of Business ESTABLISHED 1882. No. 5045. 22 PAGES. HONOLULU, TERRITORY OF HAWAII, SATURDAY, SEPTEMBER 30, 1911. 22 PAGES. PRICE 5 CENTS. f TURKEY APPEALS TO POWERS U. S. To AID HER ITALY'S DEADLY ROW ATTENDS OPENING OF COLLEGE BUILDING BIDS Campbell's 1 r . : IATTACK ALREADY ' Scheme Is WINNING THE WAR Beaten I tAasoclnled Press Cable.') pii m:u i;n woitK I y ) ;' TRIPOLI, Turkey, Sept. 30. Turkey hat appealed to the powers. iiilhhn 5 With Italy's twlft attack, already tending the Turkish war vettels to liillllill lln KupTlnli ihIpiiI Miiraton the bottom of the ocean, cut olf from gaining access to her land forces, tho ('iiiiIh-I- I llRiirnl II Empire appealed to tho world powers to Interfere in the fight, Ottoman has first, America has been asked to care for the Turks in Italy as a 7JU, ' " 4iMHHHMHBaanMSMsaanMaMsajsjajS I'niii.iil ei'wir tj skin and to guard them from tho Italians. ntlirrn nflrruninl fj Hoh ! nil of llii.ltli ii nil TRIPOLI, Sept. 30. The bombardment of the fort here has begun by tht S.inlliiry Coi.iiiiIhiiIiiii HRiiriHt It: Viililliiilo llrnl, Inl-li- 'l Italian squadron. COLLEGE1 EXTERIOR VIEW OF NEW OF HAWAII BUILDING, FOR WHICH BIDS WERE OPENED TODAY komuhI. -
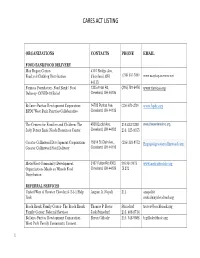
Cares Act Listing
CARES ACT LISTING ORGANIZATIONS CONTACTS PHONE EMAIL FOOD BANK/FOOD DELIVERY May Dugan Center- 4115 Bridge Ave, Food and Clothing Distribution Cleveland, OH (216) 631-5800 www.maydugancenter.net 44113, Famicos Foundation- Food Bank / Food 1325 Ansel Rd, (216) 791-6476 www.famicos.org Delivery- COVID-19 Relief Cleveland, OH 44106 Bellaire-Puritas Development Corporation- 14703 Puritas Ave, (216) 671-2710 www.bpdc.org BPDC West Park Pantries Collaborative Cleveland, OH 44135 The Centers for Families and Children- The 4500 Euclid Ave, 216.432-7200 www.thecentersohio.org. Judy Peters Basic Needs Resources Center Cleveland, OH 44103 216. 325-9355 Greater Collinwood Development Corporation- 15614 St Clair Ave., (216) 383-9772 [email protected] Greater Collinwood Food Delivery Cleveland, OH 44110 MetroWest Community Development 3167 Fulton Rd #303, 216.961.9073 www.metrowestcle.org Organization- Meals on Wheels Food Cleveland, OH 44109 X 272 Distribution REFERRAL SERVICES United Way of Greater Cleveland- 2-1-1 Help August A. Napoli 211 anapoli@ Link unitedwaycleveland.org Beech Brook Family Center- The Beech Brook Thomas P. Rover Stinedurf [email protected] Family Center: Referral Services Jack Stinedurf 216. 408-8714 Bellaire-Puritas Development Corporation- Bryan Gillooly 216. 548-9088 [email protected] West Park Family Community Connect 1 CARES ACT LISTING CHN Housing Partners- Integrated Services for Kevin J. Nowak Skapura KNowak@ COVID-19 affected low-income Cleveland Lydia Skapura 216. 912-2208 Chnhousingpartners.org households Detroit Shoreway Community Development Emily Bischoff 216.961-4242 [email protected] Organization- DSCDO COVID Relief Referral X-243 Services Frontline Services- Eviction Prevention through Susan Neth Taylor susan.neth@ Mediation Corrie Taylor 216.