IMPF Newsletter Feb-May 2015 Air Pollution: Impact on Public Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

C O N T E N T S
22.12.2014 1 C O N T E N T S Sixteenth Series, Vol.VI, Third Session, 2014/1936 (Saka) No.21, Monday, December 22, 2014/Pausa 1, 1936 (Saka) S U B J E C T P A G E S OBITUARY REFERENCE 2 ORAL ANSWERS TO QUESTIONS Starred Question No.401 to 405 4-44 WRITTEN ANSWERS TO QUESTIONS Starred Question Nos.406 to 420 45-98 Unstarred Question Nos.4601to 4830 99-495 The sign + marked above the name of a Member indicates that the Question was actually asked on the floor of the House by that Member. 22.12.2014 2 PAPERS LAID ON THE TABLE 496-508 MESSAGE FROM RAJYA SABHA 509 BUSINESS ADVISORY COMMITTEE 509 10th Report COMMITTEE ON WELFARE OF SCHEDULED 509 CASTES AND SCHEDULED TRIBES Study Tour Report COMMITTEE ON PAPERS LAID ON THE TABLE 510 1st and 2nd Reports STANDING COMMITTEE ON AGRICULTURE 510 5th Report STANDING COMMITTEE ON INFORMATION 510-511 TECHNOLOGY 1st to 4th Reports STANDING COMMITTEE ON DEFENCE 511 2nd to 5th Reports STANDING COMMITTEE ON ENERGY 511-512 st rd 1 to 3 Reports STANDING COMMITTEE ON EXTERNAL AFFAIRS 512 3rd and 4th Reports STANDING COMMITTEE ON FINANCE 512 4th, 8th, and 9th Reports STANDING COMMITTEE ON FOOD, CONSUMER 513 AFFAIRS AND PUBLIC DISTRIBUTION 1st and 2nd Reports STANDING COMMITTEE ON LABOUR 513 3rd Report 22.12.2014 3 STANDING COMMITTEE ON COAL AND STEEL 513-514 1st to 6th Reports STANDING COMMITTEE ON COMMERCE 514 115th and 116th Reports STANDING COMMITTEE ON HOME AFFAIRS 515 182nd and 183rd Reports STATEMENTS BY MINISTERS (i)Status of implementation of the recommendations contained in the 251st Report of the Standing Committee on Industry on ‘functioning of Prime Minister’s Employment Generation Programme (PMEGP)’, pertaining to the Ministry of Micro, Small and Medium Enterprises. -
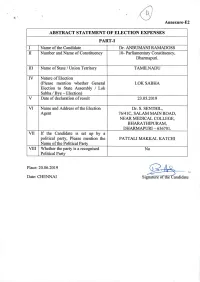
ABSTRACT STATEMENT of ELECTION EXPENSES PART-I I Name of the Candidate Dr
Annexure-E2 ABSTRACT STATEMENT OF ELECTION EXPENSES PART-I I Name of the Candidate Dr. ANBUMANI RAMADOSS II Number and Name of Constituency 10- Parliamentary Constituency, Dharmapuri. III Name of State / Union Territory TAMILNADU IV Nature of Election (Please mention whether General LOK SABHA Election to State Assembly / Lok Sabha / Bye - Election) V Date of declaration of result 23.05.2019 VI Name and Address of the Election Dr. S. SENTHIL, Agent 76/41C, SALAM MAIN ROAD, NEAR MEDICAL COLLEGE, BHARATHIPURAM, DHARMAPURI - 636701. VII If the Candidate is set up by a political party, Please mention the PATTALI MAKKAL KATCHI Name of the Political Party VIII Whether the party is a recognised No Political Party_______________ Place: 20.06.2019 O Date: CHENNAI Signature of theCandidate PART-II ABSTRACT OF STATEMENT OF ELECIONS EXPENDITURE OF CANDIDATE Amt. Incurred Amt. Incurred / Amt. Incurred Total Election S. Auth. By Authorized by Particulars Authorized by Expenditure No Candidate / Pol. Party in others in Rs. (3)+(4)+(5) Election Rs. agent in Rs. in 121 151 I Expenses in public meeting, rally, procession etc., I.(a) Expenses in Public Meeting, Rally, Procession etc. (i.e other than the ones 1732042 1732042 with Star Campaigners of the Political party. (Enclose as per Schedule-I) I.(b) Expenditure in public meeting rally, procession etc. with the Star Campaigners (i.e other than those for 1375820 1375820 general party propaganda) (Enclose as per Schedule-2) II Campaign materials other than those used in the public meeting, rally, procession -

Working of Central Board of Film Certification (Cbfc) and Academic Activities of Satyajit Ray Film & Television Institute (S
121 WORKING OF CENTRAL BOARD OF FILM CERTIFICATION (CBFC) AND ACADEMIC ACTIVITIES OF SATYAJIT RAY FILM & TELEVISION INSTITUTE (SRFTI), KOLKATA FOR THE PERIOD FROM 2010-11 TO 2014-15 [Action Taken by the Government on the Observations/Recommendations of the Committee th contained in their Ninety-fourth Report (16 Lok Sabha)] MINISTRY OF INFORMATION & BROADCASTING PUBLIC ACCOUNTS COMMITTEE (2018-19) ONE HUNDRED AND TWENTY FIRST REPORT SIXTEENTH LOK SABHA LOK SABHA SECRETARIAT NEW DELHI PAC NO. 2160 ONE HUNDRED AND TWENTY FIRST REPORT PUBLIC ACCOUNTS COMMITTEE (2018-19) (SIXTEENTH LOK SABHA) WORKING OF CENTRAL BOARD OF FILM CERTIFICATION (CBFC) AND ACADEMIC ACTIVITIES OF SATYAJIT RAY FILM & TELEVISION INSTITUTE (SRFTI), KOLKATA FOR THE PERIOD FROM 2010-11 TO 2014-15 [Action Taken by the Government on the Observations/Recommendations of the Committee th contained in their Ninety-fourth Report (16 Lok Sabha)] MINISTRY OF INFORMATION & BROADCASTING Presented to Lok Sabha on: 18.12.2018 Laid in Rajya Sabha on: 18.12.2018 LOK SABHA SECRETARIAT N E W D E L H I December, 2018 /Agrahayana, 1940 (Saka) CONTENTS PAGE COMPOSITION OF THE PUBLIC ACCOUNTS COMMITTEE (2018-19) (iii) INTRODUCTION (iv) CHAPTER I Report 1 CHAPTER II Observations/Recommendations which have been accepted by the Government CHAPTER III Observations/Recommendations which the Committee do not desire to pursue in view of the replies received from the Government CHAPTER IV Observations/Recommendations in respect of which replies of the Government have not been accepted by the Committee -
LOK SABHA ___ SYNOPSIS of DEBATES (Proceedings Other Than
LOK SABHA ___ SYNOPSIS OF DEBATES (Proceedings other than Questions & Answers) ______ Wednesday, August 13, 2014 / Shravana 22, 1936 (Saka) ______ OBITUARY REFERENCE HON'BLE SPEAKER: Hon. Members, I have to inform the House of the sad demise of Shri Resham Lal Jangde. Shri Jangde died on 11 August, 2014 in Raipur, Chhattisgarh at the age of 89. He was a member of the First, Second and Ninth Lok Sabhas representing the Bilaspur Parliamentary Constituency of Madhya Pradesh, now in Chhattisgarh. An able parliamentarian, Shri Jangde served as a member of various Parliamentary Committees. Shri Jangde was a member of the Madhya Pradesh Legislative Assembly for three terms from 1962 to 1967, 1972 to 1977 and from 1985 to 1989. He also served as Deputy Minister in the Government of Madhya Pradesh in 1963. An active social and political worker, Shri Jangde participated in freedom movement. He worked relentlessly for social harmony and eradication of the dowry system. We deeply mourn the loss of Shri Resham Lal Jangde and convey our condolences to the bereaved family. The Members then stood in silence for a short while. ELECTION OF DEPUTY SPEAKER THE MINISTER OF HOME AFFAIRS (SHRI RAJNATH SINGH) moved that Dr. M. Thambidurai , a member of this House, be chosen as the Deputy Speaker of this House. THE MINISTER OF EXTERNAL AFFAIRS AND MINISTER OF OVERSEAS INDIAN AFFAIRS (SHRIMATI SUSHMA SWARAJ) seconded the motion. SHRI BHARTRUHARI MAHTAB moved that Dr. M. Thambidurai, a member of this House, be chosen as the Deputy Speaker of this House. SHRI TATHAGATA SATPATHY seconded the motion. -
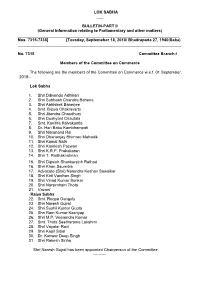
LOK SABHA ___ BULLETIN-PART II (General Information Relating To
LOK SABHA ___ BULLETIN-PART II (General Information relating to Parliamentary and other matters) ________________________________________________________________________ Nos. 7315-7338] [Tuesday, Septemeber 18, 2018/ Bhadrapada 27, 1940(Saka) _________________________________________________________________________ No. 7315 Committee Branch-I Members of the Committee on Commerce The following are the members of the Committee on Commerce w.e.f. 01 September, 2018:- Lok Sabha 1. Shri Dibyendu Adhikari 2. Shri Subhash Chandra Baheria 3. Shri Abhishek Banerjee 4. Smt. Bijoya Chakravarty 5. Shri Jitendra Chaudhury 6. Shri Dushyant Chautala 7. Smt. Kavitha Kalvakuntla 8. Dr. Hari Babu Kambhampati 9. Shri Nityanand Rai 10. Shri Dhananjay Bhimrao Mahadik 11. Shri Kamal Nath 12. Shri Kamlesh Paswan 13. Shri K.R.P. Prabakaran 14. Shri T. Radhakrishnan 15. Shri Dipsinh Shankarsinh Rathod 16. Shri Khan Saumitra 17. Advocate (Shri) Narendra Keshav Sawaikar 18. Shri Kirti Vardhan Singh 19. Shri Vinod Kumar Sonkar 20. Shri Narsimham Thota 21. Vacant Rajya Sabha 22. Smt. Roopa Ganguly 23. Shri Naresh Gujral 24. Shri Sushil Kumar Gupta 25. Shri Ram Kumar Kashyap 26. Shri M.P. Veerendra Kumar 27. Smt. Thota Seetharama Lakshmi 28. Shri Vayalar Ravi 29. Shri Kapil Sibal 30. Dr. Kanwar Deep Singh 31. Shri Rakesh Sinha Shri Naresh Gujral has been appointed Chairperson of the Committee. ---------- No.7316 Committee Branch-I Members of the Committee on Home Affairs The following are the members of the Committee on Home Affairs w.e.f. 01 September, 2018:- Lok Sabha 1. Dr. Sanjeev Kumar Balyan 2. Shri Prem Singh Chandumajra 3. Shri Adhir Ranjan Chowdhury 4. Dr. (Smt.) Kakoli Ghosh Dastidar 5. Shri Ramen Deka 6. -

Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health
Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health Report of the Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health National Commission on Report of the Macroeconomics and Health National Commission on Macroeconomics and Health MINISTRY OF HEALTH AND FAMILY WELFARE GOVERNMENT OF INDIA, 2005 EQUITABLE DEVELOPMENT • HEALTHY FUTURE Report of the National Commission on Macroeconomics and Health National Commission on Macroeconomics and Health Ministry of Health & Family Welfare Government of India, New Delhi August 2005 © Ministry of Health & Family Welfare, Government of India September 2005 ISBN 81-7525-633-8 This Report does not address tertiary care and related areas such as super speciality hospital development in the public or private sector, telemedicine, medical tourism, environmental pollution or food safety etc. though they are all equally important. The Commission Report is based on background papers which can be accessed from the NCMH website www.mohfw.nic.in. They have also been published in two companion volumes. This report was written during the period April 1, 2004 - March 31, 2005. Printed at: Cirrus Graphics Private Limited B 261, Phase I, Naraina Industrial Area, New Delhi 110 028 Tel: + 91 11 51411507/1508 Fax: +91 11 51417575 email: [email protected] Editors: Pranay G. Lal and Byword Editorial Consultants Cover design: Quote Design Studio ii REPORT OF THE NATIONAL COMMISSION ON MACROECONOMICS AND HEALTH Members of the National Commission on Macroeconomics & Health Shri P. -

Setback for NCP's Saseendran TN Has Dozen CM Candidates-In-Waiting
NEW DELHI | SATURDAY | JANUARY 6, 2018 nation 07 KERALA SEX-TALK SCANDAL Political gains TN has dozen CM motive behind Setback for NCP’s Saseendran triple talaq ing for the court’s decision on The woman had said in her candidates-in-waiting Complainant the woman’s plea for approach- petition that she had com- Bill: CPM ing the CPI(M)-led ruling LDF, plained against the former KUMAR CHELLAPPAN n Madurai-based son of Haassan, another film star, PTI n THIRUVANANTHAPURAM withdraws in which NCP is a partner, with Minister due to some misun- CHENNAI Karunanidhi, would react to who too had announced his a request for reinstating him in derstanding and she wanted the Stalin’s candidature. The DMK political plans is making nois- he CPI(M) on Friday the Cabinet. A judicial com- case to be withdrawn as a set- ith superstar Rajinikanth has not won any election with- es from the sidelines before he Taccused the BJP-led settlement plea mission which had looked into tlement had been reached out- Wdeclaring his political out the cooperation of Alagiri plunges into the arena. Haassan Government at the Centre of VR JAYARAJ n KOCHI the matter had already exon- side the court. She had dreams on the New Year Eve, who wields considerable influ- too has not announced the using the triple talaq bill for erated him effectively. approached the High Court Tamil Nadu politics which had ence in southern Tamil Nadu. details of the political outfit to “political gains”. Prime Minister he dreams of Kerala NCP’s In fact, Friday’s develop- after the Chief Judicial moved around former Chief Anbumani Ramadoss, son be launched by him. -
Health, Wcd, Dgps and Ngos on Implementation of the Pc & Pndt
ALL INDIA CONFERENCE OF STATE SECRETARIES - HEALTH, WCD, DGPS AND NGOS ON IMPLEMENTATION OF THE PC & PNDT ACT I. BACKGROUND It is unfortunate that for one reason or the other, the practice of female infanticide still prevails despite the fact that the gentle touch of a daughter and her voice has soothing effect on the parents. Four years since the Supreme Court has made the above-mentioned observation, the situation remains grim and this is reflected in the overall sex ratio in various states where female infanticide still prevails. However, the traditional system of killing the girl child after her birth has now given way to the more modern techniques of sex selection and female foeticide. A study of the census reports of 1991 and 2001 shows that the situation has worsened in most parts of India. The census 2001 further reveals that the situation is far worse in respect of Girl child population in the age group of 0-6, particularly in the affluent areas of Punjab (793 girls to 1000 boys), Haryana (820), Chandigarh (845), Himachal Pradesh (897) and Delhi (865). It was felt that, though the PNDT Act 1994 was amended and the amendment Act came into force in January 2003, no significant impact of the Act was felt at the grassroots level because of the difficulties associated with the implementation of the Act. 1 With a view to understanding the ground realities and impediments, in the implementation of the Pre-conception and Pre-natal Diagnostic Techniques (Prohibition of Sex Selection) Act, 1994, the National Commission for Women, decided to organize an All India Conference to debate the issue and to involve the concerned Government departments and NGOs in the consultative process. -
![19?Stcwa^]Tb2^]Vatbbbfxuc[H](https://docslib.b-cdn.net/cover/0209/19-stcwa-tb2-vatbbbfxuc-h-1630209.webp)
19?Stcwa^]Tb2^]Vatbbbfxuc[H
C M Y K !!( RNI Regn. No. MPENG/2004/13703, Regd. No. L-2/BPLON/41/2006-2008 ,+!,% .;<= ) * ++ ,,- +. +32&-4!5 ! ""# " $" % # "# % % # " " " %" $ " ! "" # " % 6" 7 6 &' () ,, * &#+,-.'.&0 112&,.32 # 46 >=6>/.?@ .>A=.(B/ !"#$% $#$#$# !# &'" !" #$$ Chief Minister Mamata won from Wayanad with a Banerjee, who had emerged as record margin, but his humil- odi hai to mumkin hai. the most vocal critic of the iating defeat at the hands of MThe evocative tagline of Prime Minister during the poll Smriti Irani in the family pock- the BJP campaign aptly reflects campaign. All the seven phas- et borough of Amethi is the poverty next five-year. Taking the party’s massive victory in es of the polls were marred by cruelest blow the BJP has a dig at Left parties and their the Lok Sabha polls. The brand violence, and both the PM inflicted on the Congress chief. tating that the landslide alleged commitment to the ‘Modi’ has outshone every and BJP chief Amit Shah had The results show that in Srepeat mandate has sur- welfare of workers, he said the competitor, be it regional warned that those engaged in direct contest with the BJP, the prised the whole world and put BJP Government provided satraps or Congress president bloodletting will pay for it Congress has no chance to forward a “new narrative” for pension to 40 crore labourers Rahul Gandhi, who found few after the elections. Now, that survive. The two parties were India for waging a decisive bat- in the unorganised sector. takers for his “chowkidar chor the BJP stands neck and neck locked in direct contest on tle against poverty, Prime Even as Shah in his address hai” jibe at the PM. -

Supply and Infrastructure Development for Natural
127 SUPPLY AND INFRASTRUCTURE DEVELOPMENT FOR NATURAL GAS MINISTRY OF PETROLEUM AND NATURAL GAS PUBLIC ACCOUNTS COMMITTEE (2018-19) ONE HUNDRED AND TWENTY SEVENTH REPORT SIXTEENTH LOK SABHA LOK SABHA SECRETARIAT NEW DELHI 1 PAC NO. 2166 ONE HUNDRED AND TWENTY SEVENTH REPORT PUBLIC ACCOUNTS COMMITTEE (2018-19) (SIXTEENTH LOK SABHA) SUPPLY AND INFRASTRUCTURE DEVELOPMENT FOR NATURAL GAS MINISTRY OF PETROLEUM AND NATURAL GAS Presented to Lok Sabha on: 19.12.2018 Laid in Rajya Sabha on: 19.12.2018 LOK SABHA SECRETARIAT N E W D E L H I December, 2018/Agrahayana 1940 (Saka) 2 CONTENTS PAGES COMPOSITION OF THE SUB-COMMITTEE V OF PUBLIC ACCOUNTS COMMITTEE (2014-2015)…….. (iii) COMPOSITION OF THE PUBLIC ACCOUNTS COMMITTEE (2018-2019)…….. (iv) INTRODUCTION ……………………………………………………………….…. (v) PART- I I INTRODUCTORY 1-2 II INFRASTRUCTURE DEVELOPMENT 3-10 A. PIPELINE INFRASTRUCTURE 3-8 B. R-LNG TERMINALS 8-10 III IMPACT OF NON-AVAILABILITY OF NG/R-LNG ON FERTILIZER 10-13 SECTOR IV IMPACT OF NON-AVAILABILITY OF NG/R-LNG ON POWER 13-16 SECTOR V SUPPLY OF NATURAL GAS 16-24 PART – II Observations/Recommendations 25-28 APPENDICES *I. Minutes of the 2nd sitting of Sub-Committee V of Public Accounts Committee (2015-16) held on 02.12.2015. II. Minutes of the 6th sitting of Public Accounts Committee (2018-19) held on 22.06.2018. III. Minutes of the 21st sitting of Public Accounts Committee (2018-19) held on 14.12.2018. 3 COMPOSITION OF PUBLIC ACCOUNTS COMMITTEE (2018-19) MEMBERS LOK SABHA 2. Shri Subhash Chandra Baheria 3. Shri Sudip Bandyopadhyay 4. -

Chandigarh Administration on Ings Like Wedding Would Be Vate Hospitals on Cost-To-Cost Elected Representative, Damag- Were Pelted on Sunday
. E' - )9,F # ,9,F F (*&2(-34 & !!&/ 3&-45 $010%,2 - :, 0-O" *H 8 DI 0 :0 3 ' '-" '3 /0 00 0 H/32 B3- BHB0"2 -H "0" '3 '0 3"3 3. 2 J :"3 00' 0 H 80 B .*82 /014D ((. 454 G " # 0 5 6$ 4"7"8 "" ( $#) P O 4567 2 8 " , $ &* $ , # # ,1 , ) $ %& $#' Jaishankar will not hold bilat- ' # eral talks with his Pakistani , 9 # counterpart Shah Mehmood Qureshi on the sidelines of the !" conference. However, he will #$% meet Foreign Ministers of other &'( : O , member countries including ! 02 0 # China, sources said. ' # The main focus of the talks " ;<< , =>;5? ,@ ndia and China will discuss with Wang Yi will be to find an : ways to hasten up disen- amicable and mutually agree- #$ I gagement at the Line of Actual able solution to disengage and , Control (LAC) in Ladakh dur- de-escalate the tension at the 9 02 0 ing External Affairs Minister LAC. Jaishankar and his Chinese India has all along insisted ) % he Government on Tuesday counterpart Wang Yi’s talks in that disengagement and de- $ Tissued a fresh warning to Tajikistan on Wednesday. escalation from the three fric- the people not to invite the The bilateral parleys on the tion points is the prerequisite third wave of Covid-19 by sidelines of the two-day for normalising ties with each , # flouting all social distancing Shanghai Co-operation Incidentally, the diplomatic- other. ,# A norms and crowding at hill sta- Organisation (SCO) in level talks in the last week of However, China is dilly $ B tions and tourist places even as Dushanbe come at a time when June between India and China dallying and not agreeing to sit ' Uttarakhand cancelled the a stalemate persists at three resolved to hold the military- for the 12th round of parleys. -
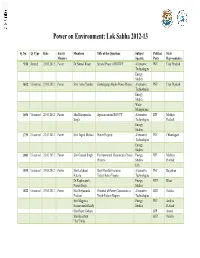
Power on Environment: Lok Sabha 2012-13
Power on Environment: Lok Sabha 2012-13 Q. No. Q. Type Date Ans by Members Title of the Questions Subject Political State Ministry Specific Party Representative *150 Starred 23.03.2012 Power Dr.Nirmal Khatri Second Phase of RGGVY Alternative INC Uttar Pradesh Technologies Energy Studies 1612 Unstarred 23.03.2012 Power Smt. Annu Tandon Kishanganga Hydro Power Project Alternative INC Uttar Pradesh Technologies Energy Studies Water Management 1656 Unstarred 23.03.2012 Power Shri Bhoopendra Agencies under RGGVY Alternative BJP Madhya Singh Technologies Pradesh Energy Studies 1739 Unstarred 23.03.2012 Power Smt. Ingrid Mcleod Power Projects Alternative INC Chhattisgarh Technologies Energy Studies 1803 Unstarred 23.03.2012 Power Shri Ganesh Singh Environmental Clearance to Power Energy BJP Madhya Projects Studies Pradesh EIA 1819 Unstarred 23.03.2012 Power Shri Lalchand Rajiv Gandhi Grameen Alternative INC Rajasthan Kataria Vidyutikaran Yojana Technologies Dr.Raghuvansh Energy RJD Bihar Prasad Singh Studies 1832 Unstarred 23.03.2012 Power Shri Nityananda Potential of Power Generation in Alternative BJD Odisha Pradhan North-Eastern Region Technologies Shri Magunta Energy INC Andhra Sreenivasulu Reddy Studies Pradesh Shri Rajen Gohain BJP Assam Shri Baijayant BJD Odisha "Jay"Panda Shri Kirti (Jha)Azad BJP Bihar *241 Starred 30.3.2012 Power Shri Power Projects Alternative CPI(M) Kerala Parayamparanbil Technologies Kuttappan Biju Rajkumari Ratna Energy INC Uttar Pradesh Singh Studies *249 Starred 30.3.2012 Power Shri Maheshwar Power Projects of NTPC Energy JD(U) Bihar Hazari Studies Shri Lalchand INC Rajasthan Kataria Starred 30.03.2012 Power Shri Ijyaraj Singh Access to Electricity Alternative INC Rajasthan *250 Technologies Shri Nityananda Energy BJD Odisha Pradhan Studies *257 Starred 30.03.2012 Power Smt.