South Sudan National Master Plan for Neglected Tropical Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nodding Syndrome Southern Sudan Medical Journal
Southern Sudan Medical Journal SSMJVolume 4. Number 1. February 2011 www.southernsudanmedicaljournal.com Two children with Nodding syndrome and their father at Lui Hospital, South Sudan. (credit: Thomas Akim). Investigation into the NODDING SYNDROME in Witto Payam Malaria in South Sudan KAP of caretakers of malnourished children Vol 4. No 1. February 2011 Southern Sudan Medical Journal CONTENTS EDITORIAL The Southern Sudan Medical Journal is a quarterly publication intended for Healthcare Professionals, Nodding Syndrome: challenges for a bizarre both those working in the Southern Sudan and those in condition Edward Eremugo Luka ...................... 2 other parts of the world seeking information on health in the Southern Sudan. It aims to offer education and information in all specialities, and to identify research MAIN ARTICLES that will inform the development of Health Services in the Southern Sudan. We plan to include reports Investigation into the Nodding syndrome of original research, critical/systematic reviews, case in Witto Payam, Western Equatoria State reports, clinical photographic materials, letters to the in 2010 John Lagu Nyungura, Thomas Akim, Editor, use of drugs, medical news of public interest, and nutrition and public health issues. Anthony Lako, Abe Gordon, Lily Lejeng and Gibson William .................................................. 3 The Journal is published in mid-February, May, August and November and is free online at Malaria in South Sudan: 1. Introduction and pathophysiology Charles Ochero Cornelio and www.southernsudanmedicaljournal.com Oromo Francis Seriano ........................................ 7 EDITORS Dr Wani Mena Malaria in South Sudan: 2. Clinical features Department of Ophthalmology and diagnosis David Attwood .......................... 10 Juba Teaching Hospital, Malaria in South Sudan: 3. Laboratory PO Box 88, Juba diagnosis Charles Ochero Cornelio Langoya ...... -

Nodding Syndrome in Ugandan Children—Clinical Features, Brain Imaging and Complications: a Case Series
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002540 on 3 May 2013. Downloaded from Nodding syndrome in Ugandan children—clinical features, brain imaging and complications: a case series Richard Idro,1,2 Robert Opika Opoka,1 Hellen T Aanyu,1 Angelina Kakooza- Mwesige,1 Theresa Piloya-Were,1 Hanifa Namusoke,1 Sarah Bonita Musoke,1 Joyce Nalugya,3 Paul Bangirana,3 Amos Deogratius Mwaka,4 Steven White,5 Kling Chong,6 Anne D Atai-Omoruto,7 Edison Mworozi,1 Jolly Nankunda,1 Sarah Kiguli,1 Jane Ruth Aceng,8 James K Tumwine1 To cite: Idro R, Opoka RO, ABSTRACT ARTICLE SUMMARY Aanyu HT, et al.Nodding Objectives: Nodding syndrome is a devastating syndrome in Ugandan neurological disorder of uncertain aetiology affecting children—clinical features, Article focus children in Africa. There is no diagnostic test, and risk brain imaging and ▪ This paper offers detailed descriptions of the complications: a case series. factors and symptoms that would allow early diagnosis clinical features and complications of nodding BMJ Open 2013;3:e002540. are poorly documented. This study aimed to describe syndrome in Ugandan children and the electro- doi:10.1136/bmjopen-2012- the clinical, electrophysiological and brain imaging physiological and brain imaging features. 002540 (MRI) features and complications of nodding syndrome ▪ It also proposes a clinical staging system for the in Ugandan children. disease. ▸ Prepublication history for Design: Case series. this paper are available Participants: 22 children with nodding syndrome Key messages ▪ online. To view these files brought to Mulago National Referral Hospital for Nodding syndrome is an epidemic neurological please visit the journal online assessment. -

Republic of South Sudan "Establishment Order
REPUBLIC OF SOUTH SUDAN "ESTABLISHMENT ORDER NUMBER 36/2015 FOR THE CREATION OF 28 STATES" IN THE DECENTRALIZED GOVERNANCE SYSTEM IN THE REPUBLIC OF SOUTH SUDAN Order 1 Preliminary Citation, commencement and interpretation 1. This order shall be cited as "the Establishment Order number 36/2015 AD" for the creation of new South Sudan states. 2. The Establishment Order shall come into force in thirty (30) working days from the date of signature by the President of the Republic. 3. Interpretation as per this Order: 3.1. "Establishment Order", means this Republican Order number 36/2015 AD under which the states of South Sudan are created. 3.2. "President" means the President of the Republic of South Sudan 3.3. "States" means the 28 states in the decentralized South Sudan as per the attached Map herewith which are established by this Order. 3.4. "Governor" means a governor of a state, for the time being, who shall be appointed by the President of the Republic until the permanent constitution is promulgated and elections are conducted. 3.5. "State constitution", means constitution of each state promulgated by an appointed state legislative assembly which shall conform to the Transitional Constitution of South Sudan 2011, amended 2015 until the permanent Constitution is promulgated under which the state constitutions shall conform to. 3.6. "State Legislative Assembly", means a legislative body, which for the time being, shall be appointed by the President and the same shall constitute itself into transitional state legislative assembly in the first sitting presided over by the most eldest person amongst the members and elect its speaker and deputy speaker among its members. -
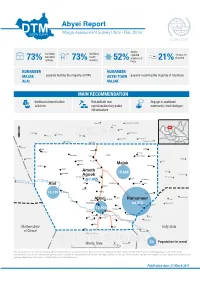
20170331 Abyei
Abyei Report Village Assessment Survey | Nov - Dec 2016 IOM OIM bomas functional functional reported villages are 73% education 73% health 52% presence of 21% deserted facilities facilities UXOs. RUMAMEER RUMAMEER MAJAK payams hosting the majority of IDPs ABYEI TOWN payams receiving the majority of returnees ALAL MAJAK MAIN SURVEY RECOMMENDATIONS MAIN RECOMMENDATION livelihood diversication Rehabilitate and Engage in sustained activities operationalize key public community-level dialogue infrastructure Ed Dibeikir Ramthil Raqabat Rumaylah Nyam Roba Nabek Umm Biura El Amma Mekeines Zerafat SUDABeida N Ed Dabkir Shagawah Duhul Kawak Al Agad Al Aza Meiram Tajiel Dabib Farouk Debab Pariang Um Khaer Langar Di@ra Raqaba Kokai Es Saart El Halluf Pagol Bioknom Pandal Ajaj Kajjam Majak Ghabush En Nimr Shigei Di@ra Ameth Nyak Kolading 15,685 Gumriak 2 Aguok Goli Ed Dahlob En Neggu Fagai 1,055 Dumboloya Nugar As Sumayh Alal Alal Um Khariet Bedheni Baar Todach Saheib Et Timsah Noong 13,130 Ed Derangis Tejalei Feid El Kok Dungoup Padit DokurAbyeia Rumameer Todyop Madingthon 68,372 Abu Qurun Thurpader Hamir Leu 12,900 Awoluum Agany Toak Banton Athony Marial Achak Galadu Arik Athony Grinঞ Agach Awal Aweragor Madul Northern Bahr Agok Unity State Lort Dal el Ghazal Abiemnom Baralil Marsh XX Population in need SOUTH SUDANMolbang Warrap State Ajakuao 0 25 50 km The boundaries on this map do not imply official endorsement or acceptance by the Government of the Republic of South Sudan or IOM. This map is for planning purposes only. IOM cannot guarantee this map is error free and therefore accepts no liability for consequential and indirect damages arising from its use. -

Wartime Trade and the Reshaping of Power in South Sudan Learning from the Market of Mayen Rual South Sudan Customary Authorities Project
SOUTH SUDAN CUSTOMARY AUTHORITIES pROjECT WARTIME TRADE AND THE RESHAPING OF POWER IN SOUTH SUDAN LEARNING FROM THE MARKET OF MAYEN RUAL SOUTH SUDAN customary authorities pROjECT Wartime Trade and the Reshaping of Power in South Sudan Learning from the market of Mayen Rual NAOMI PENDLE AND CHirrilo MADUT ANEI Published in 2018 by the Rift Valley Institute PO Box 52771 GPO, 00100 Nairobi, Kenya 107 Belgravia Workshops, 159/163 Marlborough Road, London N19 4NF, United Kingdom THE RIFT VALLEY INSTITUTE (RVI) The Rift Valley Institute (www.riftvalley.net) works in eastern and central Africa to bring local knowledge to bear on social, political and economic development. THE AUTHORS Naomi Pendle is a Research Fellow in the Firoz Lalji Centre for Africa, London School of Economics. Chirrilo Madut Anei is a graduate of the University of Bahr el Ghazal and is an emerging South Sudanese researcher. SOUTH SUDAN CUSTOMARY AUTHORITIES PROJECT RVI’s South Sudan Customary Authorities Project seeks to deepen the understand- ing of the changing role of chiefs and traditional authorities in South Sudan. The SSCA Project is supported by the Swiss Government. CREDITS RVI EXECUTIVE DIRECTOR: Mark Bradbury RVI ASSOCIATE DIRECTOR OF RESEARCH AND COMMUNICATIONS: Cedric Barnes RVI SOUTH SUDAN PROGRAMME MANAGER: Anna Rowett RVI SENIOR PUBLICATIONS AND PROGRAMME MANAGER: Magnus Taylor EDITOR: Kate McGuinness DESIGN: Lindsay Nash MAPS: Jillian Luff,MAPgrafix ISBN 978-1-907431-56-2 COVER: Chief Morris Ngor RIGHTS Copyright © Rift Valley Institute 2018 Cover image © Silvano Yokwe Alison Text and maps published under Creative Commons License Attribution-Noncommercial-NoDerivatives 4.0 International www.creativecommons.org/licenses/by-nc-nd/4.0 Available for free download from www.riftvalley.net Printed copies are available from Amazon and other online retailers. -

Survey of South Sudan Public Opinion April 24 to May 22, 2013 Survey Methodology
Survey of South Sudan Public Opinion April 24 to May 22, 2013 Survey Methodology • The International Republican Institute (IRI) undertook a public opinion poll in all 10 states of South Sudan. Training of the poll researchers was performed by Opinion Research Business (ORB), an international opinion research firm. Fieldwork management, analysis, supervision and execution were done by IRI under critical guidance of ORB. • Data was collected via face-to-face interviews from April 24 – May 22, 2013. • The population studied was adults ages 18 and older. A representative random sample was designed based on the latest population estimates reported in the 2010 Statistical Yearbook for South Sudan. • The survey employed probability proportional to size (PPS) sampling methodology. The population of South Sudan was stratified first at the region level and then by the state level. Within each state, IRI and ORB then selected counties. This was done by creating a multi-stage probability sample. Enumeration areas within each county were selected using PPS; households within each enumeration area were then identified using a random walk method, the days code and a skip pattern; respondents were randomly chosen within households using a Kish grid. Every other interview was conducted with a female to try to achieve 50 percent gender parity. • The questionnaire was translated into Bari, Classical Arabic, Dinka, English, Juba Arabic and Nuer (portions of the questionnaire were orally translated into other languages by the interviewer). 2 Survey Methodology • The margin of error is +/- 1.9 percent. The margin of error for subsets (i.e. age/education/tribes/ etc.) is significantly higher and should be treated as indicative only. -

Environmental, Dietary and Case-Control Study of Nodding Syndrome in Uganda: a Post-Measles Brain Disorder Triggered by Malnutrition?
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Journal of the Neurological Sciences 369 (2016) 191–203 Contents lists available at ScienceDirect Journal of the Neurological Sciences journal homepage: www.elsevier.com/locate/jns Environmental, dietary and case-control study of Nodding Syndrome in Uganda: A post-measles brain disorder triggered by malnutrition? Peter S. Spencer a,b,c,d,⁎, Rajarshi Mazumder a,1, Valerie S. Palmer a,b,d, Michael R. Lasarev c, Ryan C. Stadnik a,2, Peter King a,3, Margaret Kabahenda e, David L. Kitara c, Diane Stadler f, Breanna McArdle g, James K. Tumwine h, other Members of the Oregon-Uganda Nodding Syndrome Research Team 4: a Global Health Center (former), Oregon Health & Science University, Portland, OR, USA b Department of Neurology, School of Medicine, Oregon Health & Science University, Portland, OR, USA c Oregon Institute of Occupational Health Sciences, Oregon Health & Science University, Portland, OR, USA d Faculty of Medicine, Gulu University, Gulu, Uganda e Department of Food Technology and Nutrition, College of Agricultural and Environmental Sciences, Makerere University, Kampala, Uganda f Graduate Program in Human Nutrition, School of Medicine, Oregon Health & Science University, Portland, OR, USA g Department of Public Health and Preventive Medicine, Oregon Health & Science University, Portland, OR, USA h Department of Paediatrics and Child Health, Makerere University College of Health Sciences, Makerere University, Kampala, Uganda article info abstract Article history: Nodding Syndrome (NS) is an epileptic encephalopathy characterized by involuntary vertical head nodding, Received 5 August 2016 other types of seizures, and progressive neurological deficits. -
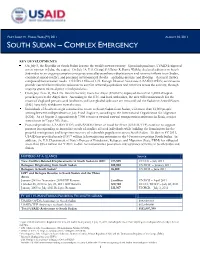
South Sudan Complex Emergency Fact
FACT SHEET #1, FISCAL YEAR (FY) 2011 AUGUST 10, 2011 SOUTH SUDAN – COMPLEX EMERGENCY KEY DEVELOPMENTS On July 9, the Republic of South Sudan became the world’s newest country. Upon independence, USAID designated a new mission in Juba, the capital. On July 14, U.S. Chargé d’Affaires R. Barrie Walkley declared a disaster in South Sudan due to an ongoing complex emergency caused by population displacement and returnee inflows from Sudan, continued armed conflict, and perennial environmental shocks—including drought and flooding—that may further compound humanitarian needs. USAID’s Office of U.S. Foreign Disaster Assistance (USAID/OFDA) continues to provide essential humanitarian assistance to conflict-affected populations and returnees across the country, through ongoing grants initiated prior to independence. From July 16 to 31, the U.N. Interim Security Force for Abyei (UNISFA) deployed more than 1,600 Ethiopian peacekeepers to the Abyei Area. According to the U.N. and local authorities, the area will remain unsafe for the return of displaced persons until landmines and unexploded ordnance are removed and the Sudanese Armed Forces (SAF) have fully withdrawn from the area. Individuals of Southern origin continued to return to South Sudan from Sudan, with more than 12,000 people arriving between independence on July 9 and August 8, according to the International Organization for Migration (IOM). As of August 3, approximately 7,500 returnees awaited onward transportation assistance in Renk, a major transit town in Upper Nile State. Post-independence, USAID/OFDA and USAID’s Office of Food for Peace (USAID/FFP) continue to support partners in responding to immediate needs of conflict-affected individuals while building the foundations for the peaceful reintegration and long-term recovery of vulnerable populations across South Sudan. -

International Journal of Multicultural and Multireligious Understanding (IJMMU) Vol
Comparative Study of Post-Marriage Nationality Of Women in Legal Systems of Different Countries http://ijmmu.com [email protected] International Journal of Multicultural ISSN 2364-5369 Volume 8, Issue 5 and Multireligious Understanding May, 2021 Pages: 238-259 Anthropological Narratives of Nodding Disease among the Acholi of Northern Uganda Alexander Paul Isiko1; Keddy Olanya Acayo2 1 Faculty of Arts and Social Sciences, Department of Religious Studies and Philosophy, Kyambogo University, Uganda 2 Department of Religious Studies and Philosophy, Kyambogo University, Uganda http://dx.doi.org/10.18415/ijmmu.v8i4.2554 Abstract Despite the scientific and specific medical interventions, nodding disease with neither a cure nor plausible explanation to its cause continues to affect the people of Acholi sub region. The disease continues to be a mystery to both the medical professionals and its victims. The World Health Organisation (WHO) affirms no known aetiology. It is so mystical that it affects only children between the ages of five and fifteen years; the disease has only been reported in Acholi sub region in Uganda without a previous history of existence in the area. In spite of the disease’s association to the Lord’s Resistance Army (LRA) war and Internally Displaced People’s (IDP) camps, other areas like Lango and Teso sub regions affected by the same have not experienced this disease. Nodding disease, therefore, seems to have defeated Western science of biomedicine and needs a different approach to explain its existence. Overtime, African societies, the Acholi inclusive, find solace in their cultural and religious beliefs to explain the existence and treatment of diseases. -

Nodding Syndrome: the Unresolved Mystery of a Pediatric Disease in Sub-Saharan Africa
HOT TOPICS FROM THE OXFORD INFECTION AND IMMUNITY IN CHILDREN COURSE Nodding Syndrome: The Unresolved Mystery of a Pediatric Disease in Sub-Saharan Africa Gasim Abd-Elfarag, MD and Michaël Boele van Hensbroek, MD, PhD are generally poor and often had a history of displacement as a Nodding syndrome is a mysterious neurologic illness of unknown result of civil conflict.1 etiology, presenting with distinctive clinical features often at early age. Currently, it affects children in restricted geographical areas in South Sudan, Northern Uganda and Southern Tanzania and is associated with CLINICAL PRESENTATION high mortality and morbidity, especially in the children with severe dis- The early stage of NS is often characterized by the occur- ease. In this paper, we will give an outline of what is known about nodding rence of a repetitive head nodding, with a frequency of 5–20 nods syndrome with respect to epidemiology, clinical presentation, etiology per minute, which is the result of a brief loss of neck muscle tone and treatment. In addition, a possible approach to resolving the mystery is due to generalized seizure activity recorded by electroencephalo- presented. gram.8,10,17,18 Nodding episodes may be provoked by food and cold weather8,10,17,18,20 and in 20% are preceded by prodromal symptoms, (Pediatr Infect Dis J 2019;38:S67–S71) including dizziness, inattention, excessive sleepiness or expres- sionless staring when food is offered.17 EPIDEMIOLOGY When the disease progresses, which occur in over 80% of Nodding syndrome (NS) poses a major public health con- cases, other types of seizures, including partial complex, generalized cern in parts of Tanzania, Uganda and South Sudan, with thousands tonic-clonic and atypical absence seizures may develop.10,12,15,17–19 of children affected.1–4 However, it is not a new disease. -

1Baugust 21, 2019
EAST AFRICA Seasonal Monitor August 21, 2019 Average to above-average rainfall in northern and western sectors favorable for cropping conditions KEY MESSAGES • Figure 1. CHIRPS preliminary rainfall performance as a June-September rainfall performance remained average to percent of normal (1981-2010), July 11 – August 10, 2019 above-average from early July to early August in unimodal areas. This has sustained largely favorable cropping conditions across northern and western agricultural zones of East Africa. • Persistent, heavy rainfall led to reports of flooding in several regions of Sudan, Ethiopia, and South Sudan as of early August. Worst-affected areas include in Khartoum, Sennar, and west Darfur states in Sudan; Afar and northwest Amhara region in Ethiopia; and Northern Bahr el Ghazal and Jonglei states of South Sudan. More rain is forecast in coming weeks. • The eastern Horn and Tanzania remained seasonally sunny but atypically hotter than normal, which has accelerated declines in water and pasture availability in pastoral areas of Kenya, parts of eastern Ethiopia, and central and southern Somalia. • There is increased concern for post-harvest maize losses, for the on-going harvest and drying in parts of eastern Uganda and western Kenya, as sustained moderate to heavy rains are forecast this month. Source: FEWS NET/Climate Hazards Center SEASONAL PROGRESS Figure 2. eMODIS/NDVI percent of normal (2007-2016), Rainfall performance from July 11th to August 10th was broadly August 1-10, 2019 average across the northern and western sectors of the region, though localized areas received well above-average rainfall amounts. Unimodal rainfall-dependent areas include Sudan, South Sudan, Ethiopia, Uganda, and western Kenya (Figure 1). -

C the Impact of Conflict on the Livestock Sector in South Sudan
C The Impact of Conflict on the Livestock Sector in South Sudan ACKNOWLEDGMENTS The authors would like to express their gratitude to the following persons (from State Ministries of Livestock and Fishery Industries and FAO South Sudan Office) for collecting field data from the sample counties in nine of the ten States of South Sudan: Angelo Kom Agoth; Makuak Chol; Andrea Adup Algoc; Isaac Malak Mading; Tongu James Mark; Sebit Taroyalla Moris; Isaac Odiho; James Chatt Moa; Samuel Ajiing Uguak; Samuel Dook; Rogina Acwil; Raja Awad; Simon Mayar; Deu Lueth Ader; Mayok Dau Wal and John Memur. The authors also extend their special thanks to Erminio Sacco, Chief Technical Advisor and Dr Abdal Monium Osman, Senior Programme Officer, at FAO South Sudan for initiating this study and providing the necessary support during the preparatory and field deployment phases. DISCLAIMER FAO South Sudan mobilized a team of independent consultants to conduct this study. The views and opinions expressed in this report are those of the authors and do not necessarily reflect the views of FAO. COMPOSITION OF STUDY TEAM Yacob Aklilu Gebreyes (Team Leader) Gezu Bekele Lemma Luka Biong Deng Shaif Abdullahi i C The Impact of Conflict on the Livestock Sector in South Sudan TABLE OF CONTENTS ACKNOWLEDGMENTS………………………………………………………………………………………………………………………………………...I ABBREVIATIONS ..................................................................................................................................................... VI NOTES ..................................................................................................................................................................