Targeted Next-Gen Sequencing for Detecting MLL Gene Fusions in Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-Like Mouse Models: Tracking the Role of the Hairless Gene
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 5-2006 Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-like Mouse Models: Tracking the Role of the Hairless Gene Yutao Liu University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Life Sciences Commons Recommended Citation Liu, Yutao, "Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino- like Mouse Models: Tracking the Role of the Hairless Gene. " PhD diss., University of Tennessee, 2006. https://trace.tennessee.edu/utk_graddiss/1824 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Yutao Liu entitled "Molecular and Physiological Basis for Hair Loss in Near Naked Hairless and Oak Ridge Rhino-like Mouse Models: Tracking the Role of the Hairless Gene." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the requirements for the degree of Doctor of Philosophy, with a major in Life Sciences. Brynn H. Voy, Major Professor We have read this dissertation and recommend its acceptance: Naima Moustaid-Moussa, Yisong Wang, Rogert Hettich Accepted for the Council: Carolyn R. -

AFF3 Upregulation Mediates Tamoxifen Resistance in Breast
Shi et al. Journal of Experimental & Clinical Cancer Research (2018) 37:254 https://doi.org/10.1186/s13046-018-0928-7 RESEARCH Open Access AFF3 upregulation mediates tamoxifen resistance in breast cancers Yawei Shi1†, Yang Zhao2†, Yunjian Zhang1, NiJiati AiErken3, Nan Shao1, Runyi Ye1, Ying Lin1* and Shenming Wang1* Abstract Background: Although tamoxifen is a highly effective drug for treating estrogen receptor–positive (ER+) breast cancer, nearly all patients with metastasis with initially responsive tumors eventually relapse, and die from acquired drug resistance. Unfortunately, few molecular mediators of tamoxifen resistance have been described. Here, we describe AFF3 (AF4/FMR2 family member 3), which encodes a nuclear protein with transactivation potential that confers tamoxifen resistance and enables estrogen-independent growth. Methods: We investigated AFF3 expression in breast cancer cells and in clinical breast cancer specimens with western blot and Real-time PCR. We also examined the effects of AFF3 knockdown and overexpression on breast cancer cells using luciferase, tetrazolium, colony formation, and anchorage-independent growth assays in vitro and with nude mouse xenografting in vivo. Results: AFF3 was overexpressed in tamoxifen-resistant tumors. AFF3 overexpression in breast cancer cells resulted in tamoxifen resistance, whereas RNA interference–mediated gene knockdown reversed this phenotype. Furthermore, AFF3 upregulation led to estrogen-independent growth in the xenograft assays. Mechanistic investigations revealed that AFF3 overexpression activated the ER signaling pathway and transcriptionally upregulated a subset of ER-regulated genes. Clinical analysis showed that increased AFF3 expression in ER+ breast tumors was associated with worse overall survival. Conclusions: These studies establish AFF3 as a key mediator of estrogen-independent growth and tamoxifen resistance and as a potential novel diagnostic and therapeutic target. -

Catenin in Adrenocortical Carcinoma
Combined transcriptome studies identify AFF3 as a mediator of the oncogenic effects of β-catenin in adrenocortical carcinoma Lucile Lefèvre, Hanin Omeiri, Ludivine Drougat, Constanze Hantel, Mathieu Giraud, Pierre Val, S Rodriguez, K Perlemoine, Corinne Blugeon, Felix Beuschlein, et al. To cite this version: Lucile Lefèvre, Hanin Omeiri, Ludivine Drougat, Constanze Hantel, Mathieu Giraud, et al.. Combined transcriptome studies identify AFF3 as a mediator of the oncogenic effects of β-catenin in adrenocor- tical carcinoma. Oncogenesis, Nature Publishing Group: Open Access Journals - Option C, 2015, 4 (7), pp.e161. 10.1038/oncsis.2015.20. inserm-01182372 HAL Id: inserm-01182372 https://www.hal.inserm.fr/inserm-01182372 Submitted on 31 Jul 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. OPEN Citation: Oncogenesis (2015) 4, e161; doi:10.1038/oncsis.2015.20 www.nature.com/oncsis ORIGINAL ARTICLE Combined transcriptome studies identify AFF3 as a mediator of the oncogenic effects of β-catenin in adrenocortical carcinoma L Lefèvre1,2,3, H Omeiri1,2,3,13, L Drougat1,2,3,13, C Hantel4, M Giraud1,2,3,PVal5,6,7, S Rodriguez1,2,3, K Perlemoine1,2,3, C Blugeon8,9,10, F Beuschlein4, A de Reyniès11, M Rizk-Rabin1,2,3, J Bertherat1,2,3,12 and B Ragazzon1,2,3 Adrenocortical cancer (ACC) is a very aggressive tumor, and genomics studies demonstrate that the most frequent alterations of driver genes in these cancers activate the Wnt/β-catenin signaling pathway. -

Towards Personalized Medicine in Psychiatry: Focus on Suicide
TOWARDS PERSONALIZED MEDICINE IN PSYCHIATRY: FOCUS ON SUICIDE Daniel F. Levey Submitted to the faculty of the University Graduate School in partial fulfillment of the requirements for the degree Doctor of Philosophy in the Program of Medical Neuroscience, Indiana University April 2017 ii Accepted by the Graduate Faculty, Indiana University, in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Andrew J. Saykin, Psy. D. - Chair ___________________________ Alan F. Breier, M.D. Doctoral Committee Gerry S. Oxford, Ph.D. December 13, 2016 Anantha Shekhar, M.D., Ph.D. Alexander B. Niculescu III, M.D., Ph.D. iii Dedication This work is dedicated to all those who suffer, whether their pain is physical or psychological. iv Acknowledgements The work I have done over the last several years would not have been possible without the contributions of many people. I first need to thank my terrific mentor and PI, Dr. Alexander Niculescu. He has continuously given me advice and opportunities over the years even as he has suffered through my many mistakes, and I greatly appreciate his patience. The incredible passion he brings to his work every single day has been inspirational. It has been an at times painful but often exhilarating 5 years. I need to thank Helen Le-Niculescu for being a wonderful colleague and mentor. I learned a lot about organization and presentation working alongside her, and her tireless work ethic was an excellent example for a new graduate student. I had the pleasure of working with a number of great people over the years. Mikias Ayalew showed me the ropes of the lab and began my understanding of the power of algorithms. -

Pathway Entry Into the T Lymphocyte Developmental Molecular Dissection of Prethymic Progenitor
The Journal of Immunology Molecular Dissection of Prethymic Progenitor Entry into the T Lymphocyte Developmental Pathway1 C. Chace Tydell,2 Elizabeth-Sharon David-Fung,2,3 Jonathan E. Moore, Lee Rowen,4 Tom Taghon,5 and Ellen V. Rothenberg6 Notch signaling activates T lineage differentiation from hemopoietic progenitors, but relatively few regulators that initiate this program have been identified, e.g., GATA3 and T cell factor-1 (TCF-1) (gene name Tcf7). To identify additional regulators of T cell specification, a cDNA library from mouse Pro-T cells was screened for genes that are specifically up-regulated in intrathymic T cell precursors as compared with myeloid progenitors. Over 90 genes of interest were iden- tified, and 35 of 44 tested were confirmed to be more highly expressed in T lineage precursors relative to precursors of B and/or myeloid lineage. To a remarkable extent, however, expression of these T lineage-enriched genes, including zinc finger transcription factor, helicase, and signaling adaptor genes, was also shared by stem cells (Lin؊Sca-1؉Kit؉CD27؊) and multipotent progenitors (Lin؊Sca-1؉Kit؉CD27؉), although down-regulated in other lineages. Thus, a major fraction of these early T lineage genes are a regulatory legacy from stem cells. The few genes sharply up-regulated between multipotent progenitors and Pro-T cell stages included those encoding transcription factors Bcl11b, TCF-1 (Tcf7), and HEBalt, Notch target Deltex1, Deltex3L, Fkbp5, Eva1, and Tmem131. Like GATA3 and Deltex1, Bcl11b, Fkbp5, and Eva1 were dependent on Notch/Delta signaling for induction in fetal liver precursors, but only Bcl11b and HEBalt were up-regulated between the first two stages of intrathymic T cell development (double negative 1 and double negative 2) corresponding to T lineage specification. -

Integrated Functional Genomic Analysis Enables Annotation of Kidney Genome-Wide Association Study Loci
BASIC RESEARCH www.jasn.org Integrated Functional Genomic Analysis Enables Annotation of Kidney Genome-Wide Association Study Loci Karsten B. Sieber,1 Anna Batorsky,2 Kyle Siebenthall,2 Kelly L. Hudkins,3 Jeff D. Vierstra,2 Shawn Sullivan,4 Aakash Sur,4,5 Michelle McNulty,6 Richard Sandstrom,2 Alex Reynolds,2 Daniel Bates,2 Morgan Diegel,2 Douglass Dunn,2 Jemma Nelson,2 Michael Buckley,2 Rajinder Kaul,2 Matthew G. Sampson,6 Jonathan Himmelfarb,7,8 Charles E. Alpers,3,8 Dawn Waterworth,1 and Shreeram Akilesh3,8 Due to the number of contributing authors, the affiliations are listed at the end of this article. ABSTRACT Background Linking genetic risk loci identified by genome-wide association studies (GWAS) to their causal genes remains a major challenge. Disease-associated genetic variants are concentrated in regions con- taining regulatory DNA elements, such as promoters and enhancers. Although researchers have previ- ously published DNA maps of these regulatory regions for kidney tubule cells and glomerular endothelial cells, maps for podocytes and mesangial cells have not been available. Methods We generated regulatory DNA maps (DNase-seq) and paired gene expression profiles (RNA-seq) from primary outgrowth cultures of human glomeruli that were composed mainly of podo- cytes and mesangial cells. We generated similar datasets from renal cortex cultures, to compare with those of the glomerular cultures. Because regulatory DNA elements can act on target genes across large genomic distances, we also generated a chromatin conformation map from freshly isolated human glomeruli. Results We identified thousands of unique regulatory DNA elements, many located close to transcription factor genes, which the glomerular and cortex samples expressed at different levels. -

Integrative Epigenomic Analysis Identifies Biomarkers and Therapeutic Targets in Adult B-Acute Lymphoblastic Leukemia
Published OnlineFirst October 29, 2012; DOI: 10.1158/2159-8290.CD-12-0208 RESEARCH ARTICLE Integrative Epigenomic Analysis Identifi es Biomarkers and Therapeutic Targets in Adult B-Acute Lymphoblastic Leukemia Huimin Geng 1 , 2 , 8 , Sarah Brennan 1 , Thomas A. Milne 3 , 10 , Wei-Yi Chen 4 , Yushan Li 1 , Christian Hurtz 7 , 8 , 15 , Soo-Mi Kweon 7 , Lynette Zickl 9 , Seyedmehdi Shojaee 7 , 8 , Donna Neuberg 9 , Chuanxin Huang 1 , Debabrata Biswas 4 , Yuan Xin 1 , Janis Racevskis 6 , Rhett P. Ketterling 11 , Selina M. Luger 12 , Hillard Lazarus 14 , Martin S. Tallman 5 , Jacob M. Rowe 13 , Mark R. Litzow 11 , Monica L. Guzman 1 , C. David Allis 3 , Robert G. Roeder 4 , Markus Müschen 7 , 8 , Elisabeth Paietta 6 , Olivier Elemento 2 , and Ari M. Melnick 1 Downloaded from cancerdiscovery.aacrjournals.org on September 26, 2021. © 2012 American Association for Cancer Research. Published OnlineFirst October 29, 2012; DOI: 10.1158/2159-8290.CD-12-0208 ABSTRACT Genetic lesions such as BCR–ABL1 , E2A–PBX1 , and MLL rearrangements (MLLr ) are associated with unfavorable outcomes in adult B-cell precursor acute lymphoblastic leukemia (B-ALL). Leukemia oncoproteins may directly or indirectly disrupt cytosine methylation pat- terning to mediate the malignant phenotype. We postulated that DNA methylation signatures in these aggressive B-ALLs would point toward disease mechanisms and useful biomarkers and therapeutic tar- gets. We therefore conducted DNA methylation and gene expression profi ling on a cohort of 215 adult patients with B-ALL enrolled in a single phase III clinical trial (ECOG E2993) and normal control B cells. -

Leukaemia Section
Atlas of Genetics and Cytogenetics in Oncology and Haematology OPEN ACCESS JOURNAL INIST-CNRS Leukaemia Section Short Communication t(2;11)(p21;q23) KMT2A/? Jean-Loup Huret Medical Genetics, Dept Medical Information, University of Poitiers, CHU Poitiers Hospital, F-86021 Poitiers, France. [email protected] Published in Atlas Database: August 2016 Online updated version : http://AtlasGeneticsOncology.org/Anomalies/t0211ID1109.html Printable original version : http://documents.irevues.inist.fr/bitstream/handle/2042/68248/08-2016-t0211ID1109.pdf DOI: 10.4267/2042/68248 This article is an update of : Fleischman EW. t(2;11)(p21;q23). Atlas Genet Cytogenet Oncol Haematol 2000;4(1) This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 2.0 France Licence. © 2017 Atlas of Genetics and Cytogenetics in Oncology and Haematology Phenotype/cell stem origin Abstract Although at least 43 cases of t(2;11)(p21;q23) have Review on t(2;11)(p21;q23) with MLL (KMT2A) been described in hematological malignancies (19 involvement, with data on clinics, and the genes MDS, 21 AML, 2 acute lymphocytic leukemia involved. (ALL) and 1 chronic lymphocytic leukemia: (CLL) Keywords (Mitelman et al., 2016)., The implication of MLL was ascertained in only 5 cases (Thirman et al., 1993; Chromosome 2; chromosome 11; MLL; KMT2A; Finke et al., 1994; Fleischman et al., 1999; Kim et acute myeloid leukemia; acute lymphoblastic al., 2002; Meyer et al., 2006), a case with a hidden leukemia involvement of AFF3 (2q11) being discarded (Hiwatari et al., 2003), while thirty two case of Clinics and pathology t(2;11)(p21;q23) without MLL rearrangement are Disease available (review in Ruano and Shetty, 2016). -
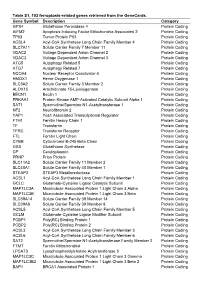
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Acute Myeloid Leukemia with T(2;6)
L al of euk rn em u i o a J Son et al., J Leuk 2013, 1:3 Journal of Leukemia DOI: 10.4172/2329-6917.1000116 ISSN: 2329-6917 Case Report Open Access Acute Myeloid Leukemia with t(2;6)(q12;q12) Reveals Dysmegakaryopoietic Finding and Poor Prognosis Jong Ae Son1, Kyung Ran Jun1*, Eul-Ju Seo2, Young-don Joo3, Seung Hwan Oh1, Ja Young Lee1, Jeong Hwan Shin1, Hye Ran Kim1 and Jeong Nyeo Lee1 1Department of Laboratory Medicine, Inje University College of Medicine, Busan, Korea 2Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea 3Department of Internal Medicine, Inje University College of Medicine, Busan, Korea Abstract We present a case of acute myeloid leukemia (AML) with a balanced translocation between chromosomes 2q12 and 6q12, t(2;6)(q12;q12). This abnormality was defined by conventional cytogenetics and multicolor banding techniques using specific probes for chromosome 2. Blasts accounted for 2% of white blood cells in peripheral blood and approximately 30% of all nucleated cells in marrow aspirates. They were medium-to-large cells with fine nuclear chromatin, indistinct nucleoli and basophilic cytoplasm. Immunophenotyping indicated the blasts were of myeloid lineage with aberrant CD7 expression. Therefore, the patient was diagnosed as ‘Acute myeloid leukemia, NOS, AML with maturation’ according to the WHO classifications. In literature review, this case should be considered as the first report of AML with t(2;6)(q12;q12). Interestingly, a bone marrow smear showed dysmegakaryopoietic findings, such as multinucleated or mononucleated megakaryocytes and micromegakaryocytes. After diagnosis, the induction chemotherapy was given with idarubicin and cytosine arabinoside according to the protocol of intermediate-prognostic AML. -

The MLL Recombinome of Acute Leukemias in 2017
OPEN Leukemia (2018) 32, 273–284 www.nature.com/leu ORIGINAL ARTICLE The MLL recombinome of acute leukemias in 2017 C Meyer1, T Burmeister2, D Gröger2, G Tsaur3, L Fechina3, A Renneville4, R Sutton5, NC Venn5, M Emerenciano6, MS Pombo-de-Oliveira6, C Barbieri Blunck6, B Almeida Lopes6, J Zuna7,JTrka7, P Ballerini8, H Lapillonne8, M De Braekeleer9,{, G Cazzaniga10, L Corral Abascal10, VHJ van der Velden11, E Delabesse12, TS Park13,SHOh14, MLM Silva15, T Lund-Aho16, V Juvonen17, AS Moore18, O Heidenreich19, J Vormoor20, E Zerkalenkova21, Y Olshanskaya21, C Bueno22,23,24, P Menendez22,23,24, A Teigler-Schlegel25, U zur Stadt26, J Lentes27, G Göhring27, A Kustanovich28, O Aleinikova28, BW Schäfer29, S Kubetzko29, HO Madsen30, B Gruhn31, X Duarte32, P Gameiro33, E Lippert34, A Bidet34, JM Cayuela35, E Clappier35, CN Alonso36, CM Zwaan37, MM van den Heuvel-Eibrink37, S Izraeli38,39, L Trakhtenbrot38,39, P Archer40, J Hancock40, A Möricke41, J Alten41, M Schrappe41, M Stanulla42, S Strehl43, A Attarbaschi43, M Dworzak43, OA Haas43, R Panzer-Grümayer43, L Sedék44, T Szczepański45, A Caye46, L Suarez46, H Cavé46 and R Marschalek1 Chromosomal rearrangements of the human MLL/KMT2A gene are associated with infant, pediatric, adult and therapy-induced acute leukemias. Here we present the data obtained from 2345 acute leukemia patients. Genomic breakpoints within the MLL gene and the involved translocation partner genes (TPGs) were determined and 11 novel TPGs were identified. Thus, a total of 135 different MLL rearrangements have been identified so far, of which 94 TPGs are now characterized at the molecular level. In all, 35 out of these 94 TPGs occur recurrently, but only 9 specific gene fusions account for more than 90% of all illegitimate recombinations of the MLL gene. -

Abundancy of Polymorphic CGG Repeats in the Human Genome Suggest a Broad Involvement in Neurological Disease Dale J
www.nature.com/scientificreports OPEN Abundancy of polymorphic CGG repeats in the human genome suggest a broad involvement in neurological disease Dale J. Annear1, Geert Vandeweyer1, Ellen Elinck1, Alba Sanchis‑Juan2,3, Courtney E. French4, Lucy Raymond2,5 & R. Frank Kooy1* Expanded CGG‑repeats have been linked to neurodevelopmental and neurodegenerative disorders, including the fragile X syndrome and fragile X‑associated tremor/ataxia syndrome (FXTAS). We hypothesized that as of yet uncharacterised CGG‑repeat expansions within the genome contribute to human disease. To catalogue the CGG‑repeats, 544 human whole genomes were analyzed. In total, 6101 unique CGG‑repeats were detected of which more than 93% were highly variable in repeat length. Repeats with a median size of 12 repeat units or more were always polymorphic but shorter repeats were often polymorphic, suggesting a potential intergenerational instability of the CGG region even for repeats units with a median length of four or less. 410 of the CGG repeats were associated with known neurodevelopmental disease genes or with strong candidate genes. Based on their frequency and genomic location, CGG repeats may thus be a currently overlooked cause of human disease. Repetitive DNA tracts make up a signifcant portion of the human genome. Short tandem repeats (STRs) are defned as DNA motifs typically ranging from 1 to 6, usually repeated between 5 to 200 units in tandem. In total, these repeats account for 3% of the total human genome 1,2. Presently, over 30 genetic disorders have been identifed resulting from STR expansions 3. CGG repeats form a specifc STR subcategory, associated with human disease, through two distinct mutational mechanisms.