Icare Program Report Improving Communications and Readmissions: Stories from Fourteen Rural Colorado Communities Presented by Colorado Rural Health Center
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
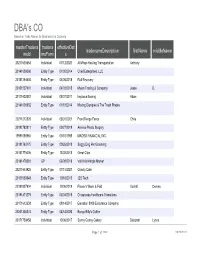
DBA's CO Based on Trade Names for Businesses in Colorado
DBA's CO Based on Trade Names for Businesses in Colorado masterTradena tradena effectiveDat tradenameDescription firstName middleName meId meForm e 20211638663 Individual 07/12/2021 All Ways Hauling Transportation Anthony 20141009560 Entity Type 01/05/2014 Chief Enterprises, LLC 20181294630 Entity Type 04/06/2018 Roll Recovery 20151237401 Individual 04/03/2015 Myers Trading & Company Jesse D. 20171602081 Individual 08/07/2017 heyzeus flooring Adam 20141035632 Entity Type 01/18/2014 Moving Disciples & The Trash Pirates 20211212829 Individual 03/01/2021 Front Range Fence Chris 20191782811 Entity Type 09/27/2019 Animas Plastic Surgery 19991088965 Entity Type 05/10/1999 MACRO FINANCIAL INC. 20181763175 Entity Type 09/26/2018 Soggy Dog Pet Grooming 20151776006 Entity Type 12/02/2015 Great Clips 20191478381 GP 06/08/2019 Vail Kris Kringle Market 20211644925 Entity Type 07/15/2021 Gravity Cafe 20131593648 Entity Type 10/16/2013 J2S Tech 20191807904 Individual 10/06/2019 Flower's Wash & Fold Xochitl Cerena 20191471279 Entity Type 06/04/2019 Crossroads Healthcare Transitions 20171612638 Entity Type 08/14/2017 Elevation 8000 Endurance Company 20201335274 Entity Type 04/14/2020 Bongo Billy's Coffee 20171759458 Individual 10/06/2017 Sunny Gunny Gallery Deborah Lynne Page 1 of 1260 09/25/2021 DBA's CO Based on Trade Names for Businesses in Colorado lastName suffix registrantOrganization address1 address2 Jackson 14580 Park Canyon rd Chief Enterprises, LLC 12723 Fulford Court Roll Recovery, LLC 5400 Spine Rd Unit C Myers 5253 N Lariat Drive Hish 10140 west evans ave. Moving Disciples & The Trash Pirates, LLC, 6060 S. Sterne Parkway Delinquent December 1, 2016 Isaacs 6613 ALGONQUIN DR Ryan Naffziger, M.D., P.C. -

Petroleum Systems and Assessment of Undiscovered Oil and Gas in the Raton Basin–Sierra Grande Uplift Province, Colorado and New Mexico by Debra K
Chapter 2 Petroleum Systems and Assessment of Undiscovered Oil and Gas in the Raton Basin–Sierra Grande Uplift Province, Colorado and New Mexico By Debra K. Higley Volume Title Page Chapter 2 of Petroleum Systems and Assessment of Undiscovered Oil and Gas in the Raton Basin– Sierra Grande Uplift Province, Colorado and New Mexico—USGS Province 41 Compiled by Debra K. Higley U.S. Geological Survey Digital Data Series DDS–69–N U.S. Department of the Interior U.S. Geological Survey U.S. Department of the Interior DIRK KEMPTHORNE, Secretary U.S. Geological Survey Mark D. Myers, Director U.S. Geological Survey, Reston, Virginia: 2007 For product and ordering information: World Wide Web: http://www.usgs.gov/pubprod Telephone: 1–888–ASK–USGS For more information on the USGS—the Federal source for science about the Earth, its natural and living resources, natural hazards, and the environment: World Wide Web: http://www.usgs.gov Telephone:1–888–ASK–USGS Any use of trade, product, or firm names is for descriptive purposes only and does not imply endorsement by the U.S. Government. Although this report is in the public domain, permission must be secured from the individual copyright owners to reproduce any copyrighted materials contained within this report. Suggested citation: Higley, D.K., 2007, Petroleum systems and assessment of undiscovered oil and gas in the Raton Basin–Sierra Grande Uplift Prov- ince, Colorado and New Mexico, in Higley, D.K., compiler, Petroleum systems and assessment of undiscovered oil and gas in the Raton Basin–Sierra Grande Uplift Province, Colorado and New Mexico—USGS Province 41: U.S. -

Summits on the Air – ARM for USA - Colorado (WØC)
Summits on the Air – ARM for USA - Colorado (WØC) Summits on the Air USA - Colorado (WØC) Association Reference Manual Document Reference S46.1 Issue number 3.2 Date of issue 15-June-2021 Participation start date 01-May-2010 Authorised Date: 15-June-2021 obo SOTA Management Team Association Manager Matt Schnizer KØMOS Summits-on-the-Air an original concept by G3WGV and developed with G3CWI Notice “Summits on the Air” SOTA and the SOTA logo are trademarks of the Programme. This document is copyright of the Programme. All other trademarks and copyrights referenced herein are acknowledged. Page 1 of 11 Document S46.1 V3.2 Summits on the Air – ARM for USA - Colorado (WØC) Change Control Date Version Details 01-May-10 1.0 First formal issue of this document 01-Aug-11 2.0 Updated Version including all qualified CO Peaks, North Dakota, and South Dakota Peaks 01-Dec-11 2.1 Corrections to document for consistency between sections. 31-Mar-14 2.2 Convert WØ to WØC for Colorado only Association. Remove South Dakota and North Dakota Regions. Minor grammatical changes. Clarification of SOTA Rule 3.7.3 “Final Access”. Matt Schnizer K0MOS becomes the new W0C Association Manager. 04/30/16 2.3 Updated Disclaimer Updated 2.0 Program Derivation: Changed prominence from 500 ft to 150m (492 ft) Updated 3.0 General information: Added valid FCC license Corrected conversion factor (ft to m) and recalculated all summits 1-Apr-2017 3.0 Acquired new Summit List from ListsofJohn.com: 64 new summits (37 for P500 ft to P150 m change and 27 new) and 3 deletes due to prom corrections. -

The Old Ross Homestead
ACREAGE AND LOCATION vaulted wood beam ceilings, a 2012 taxes $1,359.24 Presenting The Old Ross Homestead, huge glass wall that opens into the ® located just 4± miles south of La great room with huge fireplace are Spanish Peaks MLS# 12-646 Veta, Colorado at 3302 CR 360 in beautiful touches to this home. The Huerfano County, which is the home highlight is the kitchen. Small but PRICE of the famous Spanish Peaks. The mighty, the kitchen is a gourmet’s $1,250,000 ranch boasts 70± acres of lush hay paradise. Centered by a large butcher FARM RANCH & RECREATIONAL PROPERTIES www.fullerwestern.com meadows, oak brush stands and block island to prepare the meal, Broker tall trees along Wahatoya Creek. this is the social hub of the home. Paul Machmuller Additionally, there are several ponds Rustic touches include hammered 719-742-3605 to attract wildlife. The property lies copper accents, huge sink and hood [email protected] THE OLD ROSS inside a conservation easement, covering the Wolf cook stove/oven, protecting this parcel and the valley wood butcher block counter tops HOMESTEAD from future development creating a and a Sub-Zero refrigerator. The view $1,250,000 lifelong private ranch for generations from each window is both unique to come. There is a large herd of and spectacular. Additionally, the 3302 County Rd. 360 elk that live in the valley and many private, screened-in porch offers the La Veta, CO 81055 deer, bear, wild turkey and loads of perfect setting for morning coffee or small game animals call this place evening glass of wine. -

Analyses of Rocks and Minerals
UNITED STATES DEPARTMENT OF THE INTERIOR Harold L. Ickes, Secretary GEOLOGICAL SURVEY W. C. Mendenhall, Director / rf Bulletin 878 ANALYSES OF ROCKS AND MINERALS FROM THE LABORATORY OF THE UNITED STATES GEOLOGICAL SURVEY 1914-36 TABULATED BY ROGER C. WELLS Chief Chemist UNITED STATES GOVERNMENT PRINTING OFFICE WASHINGTON : 1937 For sale by the Superintendent of Documents, Washington, D. C. ------ Price 15 cents V CONTENTS Page Introduction._____________________________________________________ 1 The elements and their relative abundance.__________________________ 3 Abbreviations used._______________________________________________ 5 Classification.___________________________________________________ 5 Analyses of igneous and crystalline rocks____-_________.._____________ 6 Alaska._____-_____-__________---_-_--___-____-_____-_________ 6 \ Central Alaska________________________________________ 6 Southeastern Alaska___________-_--________________________ 7 Arizona._________--____-_---_-------___-_--------_----_______ 8 Ajo district.-_--_.____---------______--_-_--__---_______ 8 Oatman district____________-___-_-________________________ 9 Miscellaneous rocks....-._...._-............_......_._.... 10 Arkansas.____________________________________________________ 11 Austria._____________________________________________________ 11 California.__,_______________--_-_----______-_-_-_-___________ 11 T ' Ivanpah quadrangle.____-_----__--_____----_--_--__.______ 11 Lassen Peak__________________ ___________________________ 12 Mount Whitney quadrangle________________________________ -

A Taxonomic Revision of the Phrynosoma Douglasii Species Complex (Squamata: Phrynosomatidae)
Zootaxa 4015 (1): 001–177 ISSN 1175-5326 (print edition) www.mapress.com/zootaxa/ Monograph ZOOTAXA Copyright © 2015 Magnolia Press ISSN 1175-5334 (online edition) http://dx.doi.org/10.11646/zootaxa.4015.1.1 http://zoobank.org/urn:lsid:zoobank.org:pub:6C577904-2BCC-4F84-80FB-E0F0EEDF654B ZOOTAXA 4015 A taxonomic revision of the Phrynosoma douglasii species complex (Squamata: Phrynosomatidae) RICHARD R. MONTANUCCI1 1Department of Biological Sciences, Clemson University, Clemson, SC 29634-0314. E-mail: [email protected] Magnolia Press Auckland, New Zealand Accepted by A. Bauer: 16 Jun. 2015; published: 11 Sept. 2015 RICHARD R. MONTANUCCI A taxonomic revision of the Phrynosoma douglasii species complex (Squamata: Phrynosomatidae) ( Zootaxa 4015) 177 pp.; 30 cm. 11 Sept. 2015 ISBN 978-1-77557-789-8 (paperback) ISBN 978-1-77557-790-4 (Online edition) FIRST PUBLISHED IN 2015 BY Magnolia Press P.O. Box 41-383 Auckland 1346 New Zealand e-mail: [email protected] http://www.mapress.com/zootaxa/ © 2015 Magnolia Press All rights reserved. No part of this publication may be reproduced, stored, transmitted or disseminated, in any form, or by any means, without prior written permission from the publisher, to whom all requests to reproduce copyright material should be directed in writing. This authorization does not extend to any other kind of copying, by any means, in any form, and for any purpose other than private research use. ISSN 1175-5326 (Print edition) ISSN 1175-5334 (Online edition) 2 · Zootaxa 4015 (1) © 2015 Magnolia Press MONTANUCCI Table of contents Abstract . 3 Introduction . 3 Materials and methods . 5 Results and discussion . -

Pontifical Mass Planned Afternoon of July 4 Denver
1 Colorado*8 Largest Newspaper; Total Press Run, ’AU Editions, Far Above 500,000; Denver Catholic Register, 23,007 PONTIFICAL MASS PLANNED AFTERNOON OF JULY 4 ■+ Contents Copyrighted by the Catholic Press Society, Inc., 1948—Pennission to Reprodnce, Except on Articles Otherwise Marked, Given After 12 M. Friday Following Issue Over 10,000 Persons God and County DENVER CATHaiC Expected to Attend Lowry Field Service REGISTER Archbishop Vehr Will Officiate in Devotion The National Catholic Welfare Conference News Service SuppUes The Denver Catholic Register. We Unique in Colorado With Several Mem Have Also the International News Service (Wire and Mail), a Large Special Service, Seven Smaller Services, Photo Features, and Wide World Photos. bers of Hierarchy Present VOL. x x x v m . No. 43. DENVER, COLO., THURSDAY, JUNE 17, 1943. $1 PER YEAR History will be made Sunday, July 4, Independence day, when Archbishop Urban J. Vehr of Denver celebrates a Solemn Pontifical Field Mass at 4 p.m. in Lowry Field. This will be the first.time that a Pontifical Military Field Bishop Edwin V. Byrne Named Mass has ever been offered in the West in the afternoon. More than 10,000 are expected to assist at the Mass, which probably will be celebrated on the parade grounds of the air forces’ huge technical school. Military authorities Eighth Archbishop of Santa Fe announced that this will be one of the few occasions during war Meeting to Outline time that the public will be per- mitted to enter Lowry Field. Washington, D. C.—The Apos He succeeds the late Archbishop He had been stricken while dress Summer Activities All details for the Mass, which tolic Delegation has announced the R. -
Triangulation in Colorado 1927 Datum
m-q sl6”iTSv , 2-u- 4 LJ .d U. S. DEPARTMENT OF COMMERCE R. P. LAMONT, Secretary COAST AND GEODETIC SURVEY R. S. PAlTON, Dirscta Special Publication No. 160 CO ADO [ 1927 DATUM] BY OSCAR S. ADAMS Senior Mathematician UNITED STATES GOVERNMENT PRINTING OFFICE WASHINGTON 1 1930 -~~~ For sale by the Superintendent of Documents, Wanhlngton, D. C. - - - Prico 15 cent. National Oceanic and Atmospheric Administration ERRATA NOTICE One or more conditions of the original document may affect the quality of the image, such as: Discolored pages Faded or light ink Binding intrudes into the text This has been a co-operative project between the NOAA Central Library and the Climate Database Modernization Program, National Climate Data Center (NCDC). To view the original document, please contact the NOAA Central Library in Silver Spring, MD at (301) 713-2607 x124 or [email protected]. LASON Imaging.Contractor 12200 Kiln Court Beltsville, MD 20704- 1387 January 1,2006 Blank page retained for pagination PUBLICATION NOTICES The Coast and Geodetic Survey maintains mailing lists containing the names and addresses of persons interested in its publications. When a new publica- tion or a new edition of a publication is issued on any of the subjects covered by the mailing list, a circular showing the scope and contents of the publication is sent to each person whose name and address is on the mailing list of the subject covered by the publication. If you desire to receive notices regarding publications of the Coast and Geodetic Survey as issued, you should write to the Director of the Coast arid Geodetic Survey, Washington, D. -

Haplain Joseph Higgins Flown Back to U. S. Rf,Sister
“ g- 2. 19411 iinine HAPLAIN JOSEPH HIGGINS FLOWN BACK TO U. S. lountain Community THE Pueblo Priest, Home Mom RETIIEIIT [Pastore’a FOR LflyiltOMEN ,;lub uards Its Faith SOUTH E R N COLORADO For Hospitalization, E« ight to i REGINS A00.16 “ ■ E . r , Niibl, espite Isolation Led Tour to Lourdes RF,SISTER The annual retreat for laywomen unrise Valley Near Walsenburg Likened to THE OFFICIAL CA NEWSPAPER OF THE DIOCESE OF PUEBLO Recent Letter to BisHoP Gives Description of in St. Scholastica’s academy, Can* f e ’c H & -------------------------------------------------, ^---------------------------------------------------------------------------------------- on City, will be held this year be VOL. I. No. 4. FRIDAY, AUG. 3, 1945 ginning THursday evening, Aug. PXBD drinks Pioneer Settlements of State; Fr. Faisti A Pilgrimage to Home of St. Ttiereso, 16, and closing Sunday noon. Aug. 20. The Rev, Henry Huber, O.S.6., ' go* GL. 9855 Offers Mass THere Patron of Diocese of Conception abbey. Conception 2 2 N u rse Oldest Pueblo Catholic Church Mo., will conduct this year’s exer Walsenburg.—THe Kev. Francis Faisti, assistant Pas- cises. a~ n O T E l THe Very Rev. JosePH Higgins, Pastor of St. Patrick’s I uf gt, Mary's ParisH, celebrated Mass in Sunrise Valley ParisH, Pueblo, wHo Has been on leave as army cHaPlain at Women intending to make tHa |EE SHOP Inday, July *29, and uPon His return recounted a story P re se n t/ retreat should place their reserva W e< Poputar Prf„ tacHed to a HosPital unit in Paris, France, arrived in tHe tions with Mrs, L. -

United States Department of the Interior Bureau of Land Management
United States Department of the Interior Bureau of Land Management Environmental Assessment for the Royal Gorge Field Office November 2013 Competitive Oil & Gas Lease Sale Royal Gorge Field Office 3028 E. Main Canon City, CO 81212 DOI-BLM-CO-200-2013-0022-EA July 2013 TABLE OF CONTENTS Contents CHAPTER 1 - INTRODUCTION .................................................................................................. 3 1.1 IDENTIFYING INFORMATION ................................................................................... 3 1.2 PROJECT LOCATION AND LEGAL DESCRIPTION .............................................. 4 1.3 PURPOSE AND NEED .................................................................................................... 4 1.3.1 Decision to be Made .................................................................................................... 4 1.4 PUBLIC PARTICIPATION ............................................................................................ 6 1.4.1 Scoping ........................................................................................................................ 6 1.4.2 Public Comment Period ............................................................................................... 7 CHAPTER 2 - ALTERNATIVES .................................................................................................. 8 2.1 INTRODUCTION............................................................................................................. 8 2.2 ALTERNATIVES ANALYZED IN DETAIL ............................................................... -

Proceedings of the United States National Museum
PROCEEDINGS OF THE UNITED STATES NATIONAL MUSEUM issued SMITHSONIAN INSTITUTION U. S. NATIONAL MUSEUM Vol. no Washington : 1959 No. 3416 GRASSHOPPERS OF THE MEXICANUS GROUP, GENUS MELANOPLUS (ORTHOPTERA; ACRIDIDAE) By Ashley B. Gurney ^ and A. R. Brooks Introduction Since the historic outbreaks of the Rocky Mountain grasshopper (Melanoplus spretus (Walsh)) in the 1870's, the close relatives of that species, especially the one recently called M. mexicanus (Saussure), have been of great economic importance in the United States and Canada. The present study was undertaken to clarify the status of the various taxonomic entities in this complex, and we hope it will stimulate further clarifying studies. We have also attempted to summarize briefly the more important information on the biology of each species. For many years the status of spretus has been a puzzle to ento- mologists because no specimens have been collected since the early 1900's. Gradually the opinion developed that spretus disappeared because it was the migratory phase of a normally solitary grasshopper, and it was supposed that mexicanus was that species. Om* study of • Entomology Research Division, Agricultural Research Service, U. S. Department of Agriculture. ' Entomology Section, Canada Department of Agriculture Research Laboratory, Saskatoon, Saskatche- wan, Canada. 1 477119—59 1 : 2 PROCEEDESTGS OF THE NATIONAL MUSEUM vol. no the aedeagus indicates that spretus is a distinct species. Any further evidence bearing on this opinion naturally is very desirable. It is chiefly on the basis of the differences in the aedeagus that mexicanus has been found to be distinct from the species commonly misidentified as M. -

Geology of the Igneous Rocks of the Spanish Peaks Region Colorado
Geology of the Igneous Rocks of the Spanish Peaks Region Colorado GEOLOGICAL SURVEY PROFESSIONAL PAPER 594-G GEOLOGY OF THE IGNEOUS ROCKS OF THE SPANISH PEAKS REGION, COLORADO The Spanish Peaks (Las Cumbres Espanolas). Geology of the Igneous Rocks of the Spanish Peaks Region Colorado By ROSS B. JOHNSON SHORTER CONTRIBUTIONS TO GENERAL GEOLOGY GEOLOGICAL SURVEY PROFESSIONAL PAPER 594-G A study of the highly diverse igneous rocks and structures of a classic geologic area, with a discussion on the emplacement of these features UNITED STATES GOVERNl\1ENT PRINTING OFFICE, WASHINGTON : 1968 UNITED STATES DEPARTMENT OF THE INTERIOR STEWART L. UDALL, Secretary GEOLOGICAL SURVEY William T. Pecora, Director For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, D.C. 20402 CONTENTS Page Page Abstract__________________________________________ _ G1 Petrography-Continued Introduction ______________________________________ _ 1 Syenite_______________________________________ _ G19 Geologic setting ___________________________________ _ 3 Porphyry _________________________________ _ 19 General features _______________________________ _ 3 Aphanite---------------------------------- 20 Sedhnentaryrocks _____________________________ _ 4 Lamprophyre _____________________________ _ 20 Structure _____________________________________ _ 4 Syenodiorite __________________________________ _ 22 Thrust and reverse faults ___________________ _ 5 Phanerite_________________________________ _ 22 Normal faults _____________________________