Periodic Update on AEFI
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Do We Know About India's Covaxin Vaccine?
FEATURE Tamil Nadu, India COVID-19 VACCINES [email protected] BMJ: first published as 10.1136/bmj.n997 on 20 April 2021. Downloaded from Cite this as: BMJ 2021;373:n997 http://dx.doi.org/10.1136/bmj.n997 What do we know about India’s Covaxin vaccine? Published: 20 April 2021 India has rapidly approved and rolled out Covaxin, its own covid-19 vaccine. Kamala Thiagarajan examines what we know so far. Kamala Thiagarajan freelance journalist Who developed Covaxin? cheapest purchased by any country in the world at 206 rupees per shot for the 5.5 million doses the Covaxin was developed by Indian pharmaceutical government currently has on order. The government company Bharat Biotech in collaboration with the has capped the price of the vaccine sold in the private Indian Council of Medical Research, a government market, with private hospitals able to charge up to funded biomedical research institute, and its 250 rupees.13 subsidiary the National Institute of Virology. Covaxin does not require storage at sub-zero Bharat Biotech has brought to market 16 original temperatures, which would be hard to maintain in vaccines, including for rotavirus, hepatitis B, Zika India’s climate and with the frequent power cuts in virus, and chikungunya.1 The company reportedly rural areas. Covaxin is available in multi-dose vials spent $60-$70m (£43-£50m; €50-€58m) developing and is stable at the 2-8°C that ordinary refrigeration Covaxin.2 can achieve. How does Covaxin work? Bharat Biotech says it has a stockpile of 20 million The vaccine is similar to CoronaVac (the Chinese doses of Covaxin for India and is in the process of vaccine developed by Sinovac)3 in that it uses a manufacturing 700 million doses at its four facilities complete infective SARS-CoV-2 viral particle in two cities by the end of the year. -

COVID-19 Vaccines: Update on Allergic Reactions, Contraindications, and Precautions
Centers for Disease Control and Prevention Center for Preparedness and Response COVID-19 Vaccines: Update on Allergic Reactions, Contraindications, and Precautions Clinician Outreach and Communication Activity (COCA) Webinar Wednesday, December 30, 2020 Continuing Education Continuing education will not be offered for this COCA Call. To Ask a Question ▪ All participants joining us today are in listen-only mode. ▪ Using the Webinar System – Click the “Q&A” button. – Type your question in the “Q&A” box. – Submit your question. ▪ The video recording of this COCA Call will be posted at https://emergency.cdc.gov/coca/calls/2020/callinfo_123020.asp and available to view on-demand a few hours after the call ends. ▪ If you are a patient, please refer your questions to your healthcare provider. ▪ For media questions, please contact CDC Media Relations at 404-639-3286, or send an email to [email protected]. Centers for Disease Control and Prevention Center for Preparedness and Response Today’s First Presenter Tom Shimabukuro, MD, MPH, MBA CAPT, U.S. Public Health Service Vaccine Safety Team Lead COVID-19 Response Centers for Disease Control and Prevention Centers for Disease Control and Prevention Center for Preparedness and Response Today’s Second Presenter Sarah Mbaeyi, MD, MPH CDR, U.S. Public Health Service Clinical Guidelines Team COVID-19 Response Centers for Disease Control and Prevention National Center for Immunization & Respiratory Diseases Anaphylaxis following mRNA COVID-19 vaccination Tom Shimabukuro, MD, MPH, MBA CDC COVID-19 Vaccine -

COVID-19 Vaccination Programme: Information for Healthcare Practitioners
COVID-19 vaccination programme Information for healthcare practitioners Republished 6 August 2021 Version 3.10 1 COVID-19 vaccination programme: Information for healthcare practitioners Document information This document was originally published provisionally, ahead of authorisation of any COVID-19 vaccine in the UK, to provide information to those involved in the COVID-19 national vaccination programme before it began in December 2020. Following authorisation for temporary supply by the UK Department of Health and Social Care and the Medicines and Healthcare products Regulatory Agency being given to the COVID-19 Vaccine Pfizer BioNTech on 2 December 2020, the COVID-19 Vaccine AstraZeneca on 30 December 2020 and the COVID-19 Vaccine Moderna on 8 January 2021, this document has been updated to provide specific information about the storage and preparation of these vaccines. Information about any other COVID-19 vaccines which are given regulatory approval will be added when this occurs. The information in this document was correct at time of publication. As COVID-19 is an evolving disease, much is still being learned about both the disease and the vaccines which have been developed to prevent it. For this reason, some information may change. Updates will be made to this document as new information becomes available. Please use the online version to ensure you are accessing the latest version. 2 COVID-19 vaccination programme: Information for healthcare practitioners Document revision information Version Details Date number 1.0 Document created 27 November 2020 2.0 Vaccine specific information about the COVID-19 mRNA 4 Vaccine BNT162b2 (Pfizer BioNTech) added December 2020 2.1 1. -

Considerations for Causality Assessment of Neurological And
Occasional essay J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2021-326924 on 6 August 2021. Downloaded from Considerations for causality assessment of neurological and neuropsychiatric complications of SARS- CoV-2 vaccines: from cerebral venous sinus thrombosis to functional neurological disorder Matt Butler ,1 Arina Tamborska,2,3 Greta K Wood,2,3 Mark Ellul,4 Rhys H Thomas,5,6 Ian Galea ,7 Sarah Pett,8 Bhagteshwar Singh,3 Tom Solomon,4 Thomas Arthur Pollak,9 Benedict D Michael,2,3 Timothy R Nicholson10 For numbered affiliations see INTRODUCTION More severe potential adverse effects in the open- end of article. The scientific community rapidly responded to label phase of vaccine roll- outs are being collected the COVID-19 pandemic by developing novel through national surveillance systems. In the USA, Correspondence to SARS- CoV-2 vaccines (table 1). As of early June Dr Timothy R Nicholson, King’s roughly 372 adverse events have been reported per College London, London WC2R 2021, an estimated 2 billion doses have been million doses, which is a lower rate than expected 1 2LS, UK; timothy. nicholson@ administered worldwide. Neurological adverse based on the clinical trials.6 kcl. ac. uk events following immunisation (AEFI), such as In the UK, adverse events are reported via the cerebral venous sinus thrombosis and demyelin- MB and AT are joint first Coronavirus Yellow Card reporting website. As of ating episodes, have been reported. In some coun- authors. early June 2021, approximately 250 000 Yellow tries, these have led to the temporary halting of BDM and TRN are joint senior Cards have been submitted, equating to around authors. -

Electronic Support for Public Health–Vaccine Adverse Event Reporting System (ESP:VAERS)
Grant Final Report Grant ID: R18 HS 017045 Electronic Support for Public Health–Vaccine Adverse Event Reporting System (ESP:VAERS) Inclusive dates: 12/01/07 - 09/30/10 Principal Investigator: Lazarus, Ross, MBBS, MPH, MMed, GDCompSci Team members: Michael Klompas, MD, MPH Performing Organization: Harvard Pilgrim Health Care, Inc. Project Officer: Steve Bernstein Submitted to: The Agency for Healthcare Research and Quality (AHRQ) U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Abstract Purpose: To develop and disseminate HIT evidence and evidence-based tools to improve healthcare decision making through the use of integrated data and knowledge management. Scope: To create a generalizable system to facilitate detection and clinician reporting of vaccine adverse events, in order to improve the safety of national vaccination programs. Methods: Electronic medical records available from all ambulatory care encounters in a large multi-specialty practice were used. Every patient receiving a vaccine was automatically identified, and for the next 30 days, their health care diagnostic codes, laboratory tests, and medication prescriptions were evaluated for values suggestive of an adverse event. Results: Restructuring at CDC and consequent delays in terms of decision making have made it challenging despite best efforts to move forward with discussions regarding the evaluation of ESP:VAERS performance in a randomized trial and comparison of ESP:VAERS performance to existing VAERS and Vaccine Safety Datalink data. However, Preliminary data were collected and analyzed and this initiative has been presented at a number of national symposia. Key Words: electronic health records, vaccinations, adverse event reporting The authors of this report are responsible for its content. -
COVID-19 Vaccineadmin VAERS
Reporting a Suspected Vaccine Adverse Event Indian Health Service, National Pharmacy & Therapeutics Committee CAPT Matthew Clark, MD, FAAP, FACP, Chair CAPT Ryan Schupbach, PharmD, BCPS, CACP, Vice Chair CAPT Christopher Lamer, PharmD, MHS, BCPS, CDE, Director of Pharmacovigilance October 2020 Potential New Vaccine for COVID-19 • Operation Warp Speed (OWS) • Collaboration between the Federal Government and biopharmaceutical companies to develop medications, diagnostic tests, and vaccines. • Shortened timelines but safety and efficacy are the primary focus. • Vaccines must be at least 50% effective for FDA EUA or approval. • Vaccines must be safe, and benefits of immunization must outweigh any risks of adverse events. • Continued need for influenza immunization • Continued need for scheduled immunizations https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html 2 Vaccine Safety: Common Adverse Events Vaccines are considered to be safe and effective with most common adverse events being mild and are signs that the body is developing immunity: • Pain, swelling, or redness where the shot was given • Mild fever • Chills • Feeling tired • Headache • Muscle and joint aches https://www.vaccines.gov/basics/safety/side_effects 3 Vaccine Safety: Serious Adverse Events More serious side effects are rare but can occur. Some examples are: • Anaphylaxis (0.65 cases/1 million vaccinations) • Thrombocytopenia from Rubella vaccine (1 case/40,000 vaccinations) • Orchitis from Mumps vaccine (0.3 cases/1 million vaccinations) • Intussusception from Rotavirus vaccine (1 case/100,000 vaccinations) • Guillain-Barre from flu vaccine (1 case/1.25 million vaccinations; association is stronger with flu infection than the vaccine) Spencer JP, Trondsen Pawlowski RH, Thomas S. Vaccine Adverse Events: Separating Myth from Reality. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -
Immunogenicity and Safety of a Third Dose, and Immune Persistence Of
medRxiv preprint doi: https://doi.org/10.1101/2021.07.23.21261026; this version posted July 25, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Immunogenicity and safety of a third dose, and immune persistence of 2 CoronaVac vaccine in healthy adults aged 18-59 years: interim results 3 from a double-blind, randomized, placebo-controlled phase 2 clinical 4 trial 5 6 Hongxing Pan MSc1*, Qianhui Wu MPH2*, Gang Zeng Ph.D.3*, Juan Yang Ph.D.1, Deyu 7 Jiang MSc4, Xiaowei Deng MSc2, Kai Chu MSc1, Wen Zheng BSc2, Fengcai Zhu M.D.5†, 8 Hongjie Yu M.D. Ph.D.2,6,7†, Weidong Yin MBA8† 9 10 Affiliations 11 1. Vaccine Evaluation Institute, Jiangsu Provincial Center for Disease Control and 12 Prevention, Nanjing, China 13 2. School of Public Health, Fudan University, Key Laboratory of Public Health Safety, 14 Ministry of Education, Shanghai, China 15 3. Clinical Research Department, Sinovac Biotech Co., Ltd., Beijing, China 16 4. Covid-19 Vaccine Department, Sinovac Life Sciences Co., Ltd., Beijing, China 17 5. Jiangsu Provincial Center for Disease Control and Prevention, Nanjing, China 18 6. Shanghai Institute of Infectious Disease and Biosecurity, Fudan University, 19 Shanghai, China 20 7. Department of Infectious Diseases, Huashan Hospital, Fudan University, 21 Shanghai, China 22 8. Sinovac Biotech Co., Ltd., Beijing, China NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

Comparative Characteristics of the Main Coronavirus Vaccines
Acta Scientific MICROBIOLOGY (ISSN: 2581-3226) Volume 4 Issue 9 September 2021 Editorial Comparative Characteristics of the Main Coronavirus Vaccines Pavel F Zabrodskii* Received: June 23, 2021 Saratov Medical University "REAVIZ", Saratov, Russian Federation Published: August 01, 2021 *Corresponding Author: Pavel F Zabrodskii, Saratov Medical University "REAVIZ", © All rights are reserved by Pavel F Saratov, Russian Federation. Zabrodskii. Since the beginning of the epidemic, vaccine development has been a priority for all developed countries. According to WHO (26 adenovirus rather than human adenovirus should reduce the risk virus. The fact that the vaccine was developed using chimpanzee January 2021), more than 60 vaccines worldwide are already in of allergic reactions and severe side-effects. However, the disadvan- clinical trials. More than 170 are being tested on animals. There tage of this product, as with all vector vaccines, is that the technol- ogy itself is new and has not previously been used in health care. One of the pluses for vector drug manufacturers is their speed of are 22 vaccines that have made it through the final phase of testing. creation. The vaccine is registered for use in the European Union. It The vaccine, developed by US company “Pfizer” and its German is licensed for emergency use in another 20 countries. clinical trials ended on 9 November 2020. In addition to EU coun- partner “BioNTech”, has been registered first in the EU. Phase III - ceutical company Sinovac Biotech, which has shown controversial tries, the vaccine is used in Australia, Saudi Arabia, Switzerland, “CoronaVac” is an inactivated vaccine from Chinese biopharma - Norway, Iceland, Serbia and some other countries. -

Iran Hopes to Defeat COVID with Home-Grown Crop of Vaccines
Q&A Iran hopes to defeat COVID with home-grown crop of vaccines Iran is one of few Middle Eastern nations to transfer money is restricted, it is difficult with the capacity to develop vaccines. It to buy drugs and medicines. And we have has been doing so in earnest: more than the technology to produce vaccines, so why ten are in development, but little is known not use it? To ensure the safety of Iranians, it about them outside Iran. Nature speaks makes sense to develop a variety of vaccines to Kayhan Azadmanesh, head of the using different research and development virology division at the Pasteur Institute of strategies, as China has done. Iran in Tehran, about the nation’s vaccine landscape. Azadmanesh also advises the Why are Iranian researchers reluctant to Iranian government and is developing publicize their work internationally? vaccines through his spin-off company This could be another effect of the sanctions. Humimmune Biotech. Researchers in Iran might not want to draw too much attention to their work in case they How badly has the pandemic affected Iran? put potential partnerships in jeopardy or they Since January 2020, we’ve had five waves. run the risk of losing access to raw materials. We’re currently experiencing the highest Researchers are also extremely busy number of new cases reported so far, with during the pandemic. But some have started MAJID ASGARIPOUR/WANA VIA REUTERS MAJID ASGARIPOUR/WANA around 40,000 a day, and the most common to share results. In June, the researchers variant we detect is Delta. -

COVID-19 Vaccine Weekly Intel Report
COVID-19 Vaccine Weekly Intel Report Science, trial forecast, production and news analysis April 23rd - Prepared for BIO, DCVMN, IFPMA © 2021 Airfinity Ltd | Private & Confidential. © 2021 Airfinity Ltd | Private & Confidential Over 9 billion doses could be produced this year An analysis of forecasted production of vaccine candidates ForecasteD proDuction 9,889,406,370 8,478,587,508 7,206,503,589 5,982,385,185 4,871,966,540 3,815,817,604 2,870,502,904 2,080,496,478 1,388,902,344 830,218,085 200,715,588 425,929,684 Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21 Jul-21 Aug-21 Sep-21 Oct-21 Nov-21 Dec-21 © 2021 Airfinity Ltd | Private & Confidential 2 Over 9 billion doses could be produced this year An analysis of forecasted production of vaccine candidates split by candidate Ad26COVS1 (J&J) mRNA-1273 (MoDerna) Ad5-nCoV (CanSino) MVC-COV1901 (MeDigen/Dynavax) AZD1222 (University of OxforD/AstraZeneca) NasoVAX (Altimmune) BBIBP-CorV (Beijing/Sinopharm) NVX-CoV2373 (Novavax) BNT162b2 (Pfizer/BioNTech) S-268019 (UMN Pharma) CoronaVac (Sinovac) SCB-2019 (Clover/Dynavax) COVAXIN (Bharat/ICMR/NIV) Sputnik V (Gamaleya Research Institute) CoviVac (Chumakov FeDeral Scientific Center) UB-612 (Covaxx) CVnCoV (Curevac) Vaccine (Anhui Zhifei) 9,889,406,370 EpiVacCorona (VECTOR) Vaccine (MeDicago/GSK) GRAD-COV2 (Reithera/LeukoCare/Univercells ) Vaccine (Sanofi/GSK) 8,478,587,508 INO-4800 (Inovio Pharma) VLA2001 (Valneva/Dynavax) LUNAR-COV19 (Arcturus) ZyCoV-D (ZyDus Cadila) 7,206,503,589 5,982,385,185 4,871,966,540 3,815,817,604 2,870,502,904 2,080,496,478 -
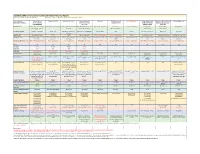
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03