Compatibility Mode
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

11-2021 Fad Diets Monthly Handout
WEEKLY CHALLENGES skdfj FIND AN EXAMPLE OF DIET CULTURE IN Photo Courtesy of Pixabay.com YOUR FAVORITE EAT WELL, AGE WELL. MAGAZINE OR MEDIA OUTLET. FAD DIETS Has it ever seemed like there new diet coming out each week claiming to be the latest and greatest for weight loss? READ AN ARTICLE OR Unfortunately, this is a common trend among Americans today. BLOG POST ABOUT Diet culture has infiltrated almost every media outlet and does not DIET CULTURE. discriminate. Your age, ethnicity, or socioeconomic status does not exclude you from being targeted by diet companies and products. Diet culture is the practice of demanding a change in our values ENJOY A NUTRITIOUS and beliefs to fit a societal expectation. This practice can be MEAL THAT HAS ALL disguised in many ways. A few examples include eating only a few FOOD GROUPS foods or eliminating groups of foods, claiming a food is a “superfood,” or promising quick results like weight loss. It is important to be educated on diet culture, so you do not fall into the SET S.M.A.R.T. trap of predatory marketing. (Specific, Measurable, Here are some indicators of a fad diet or a diet you should avoid: Attainable, Relevant, 1. A diet that excludes or severely restricts a macronutrient Timely) GOALS WHEN group such as fat or carbohydrates. IT COMES TO YOUR 2. A diet that encourages extreme caloric restriction. HEALTH. 3. A diet that promotes excessive physical activity. 4. A diet that promises quick and unrealistic results. 5. A diet that advertises weight loss greater than 2 pounds per week. -

Functional Foods in Fad Diets: a Review
Functional Foods in Health and Disease 2017; 7(9): 702-715 Page 702 of 715 Review Article Open Access Functional Foods in fad diets: A review Daniela Abigail Navaro1; Olga Raz1; Sharon Gabriel1; Vered Kaufman Shriqui1; Esther Gonen1, Mona Boaz1,2. 1Department of Nutrition Sciences, Ariel University, (Ariel), Israel; 2Epidemiology and Research Unit, E. Wolfson Medical Center, (Holon), Israel Corresponding Author: Mona Boaz, PhD, Professor, Chair, Department of Nutrition Sciences, Ariel University, Kvish 36, Ariel, 40700, Israel Submission Date: March 18th, 2017, Acceptance Date, September 27th, 2017, Publication Date: September 30th, 2017 Citation: Navaro D.A., Raz O., Gabriel S., Shriqui V.K., Boaz M., Functional Foods in Fad Diets: A Review. Functional Foods in Health and Disease 2017; 7(9); 702-715. https://doi.org/10.31989/ffhd.v7i9.346 ABSTRACT Fad diets can be defined as any diet making claims that are unrealistic and not supported by evidence-based data. Having been developed since the early 19th century, fad diets promise drastic weight loss and/or other unsubstantiated health claims while often omitting entire food groups. Their popularity with the public makes them an important topic for nutritionists and clinicians, especially in the framework of the obesity epidemic. Additionally, it is conceivable that components of fad diets can indeed facilitate weight loss, even if the diet overall is without merit. The grapefruit diet, the cabbage soup diet, and the human chorionic gonadotropin (hCG) diet are among the most popular fad diets and are reviewed within this study not only in terms of the diet plan itself, but also in terms of possible and known weight loss and health benefits provided by the foods on which the diets are based. -
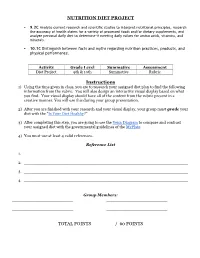
NUTRITION DIET PROJECT Instructions TOTAL POINTS / 60
NUTRITION DIET PROJECT ▪ 9.2C Analyze current research and scientific studies to interpret nutritional principles, research the accuracy of health claims for a variety of processed foods and/or dietary supplements, and analyze personal daily diet to determine if meeting daily values for amino acids, vitamins, and minerals. ▪ 10.1C Distinguish between facts and myths regarding nutrition practices, products, and physical performance. Activity Grade Level Summative Assessment Diet Project 9th & 10th Summative Rubric Instructions 1) Using the time given in class, you are to research your assigned diet plan to find the following information from the rubric. You will also design an interactive visual display based on what you find. Your visual display should have all of the content from the rubric present in a creative manner. You will use this during your group presentation. 2) After you are finished with your research and your visual display, your group must grade your diet with the “Is Your Diet Healthy?” 3) After completing this step, you are going to use the Venn Diagram to compare and contrast your assigned diet with the governmental guidelines of the MyPlate. 4) You must use at least 4 valid references. Reference List 1. _________________________________________________________________ 2. _________________________________________________________________ 3. _________________________________________________________________ 4. _________________________________________________________________ Group Members: _______________________________ -

Obesity Diets — Fact Or Fiction 913
Obesity Diets — Fact or Fiction 913 Obesity Diets — 159 Fact or Fiction SHILPA JOSHI The prevalence of overweight and obesity has concept on other hand is a technique to induce negative increased steadily over past 30 years. The rapid spread energy balance.2 of urbanization and industrialization and dramatic 1 lifestyle changes that accompany these trends had led CLASSIFICATION OF SOME POPULAR DIETS to pandemic of obesity, even in developing countries. 1. High fat - low carbohydrate – high protein diets e.g. The obesity has serious public health implications. Dr Atkins new diet revolution, protein power, life Excess weight has been associated with mortality and without bread morbidity. It is associated with cardiovascular disease, 2. Moderate fat - balance nutrient diets – high in type II diabetes, hypertension, stroke, gall bladder carbohydrate and moderate in protein, e.g. use of food disease, osteoarthritis, sleep apnea, respiratory problems guide pyramid, DASH diet, weight watchers diet and some types of cancer. 3. Low fat/very low fat – high carbohydrate – moderate Due to this reasons, weight loss is of major concern protein diets e.g. Dr. Dean Ornish’s program for 1 in today’s populations . Dietary recommendations are reversing heart disease, ‘eat more weigh less’, the key element in management of obesity. In recent years, New Pritikin program numerous dietary fads have emerged as a response to rising prevalence of obesity2. Popular diets have become HIGH FAT – LOW CARBOHYDRATE – HIGH increasingly prevalent and controversial. Some popular PROTEIN DIETS diets are based on long-standing medical advice and Low carbohydrate diets were first described by recommend restriction of portion sizes and calories (e.g. -

Some Fad Diets' Promises Sound Too Good to Be True
Some Fad Diets' Promises Sound Too Good to Be True Item Type Article Authors Brannon, Patsy M. Publisher College of Agriculture, University of Arizona (Tucson, AZ) Journal Arizona Land and People Rights Copyright © Arizona Board of Regents. The University of Arizona. Download date 30/09/2021 18:05:47 Link to Item http://hdl.handle.net/10150/295319 Some Fad Diets' Promises Sound Too Good to Be True Many overweight Americans, as well as some who just want to lose By Dr. Patsy M. Brannon 5 pounds, keep searching for an easy, guaranteed weight- reducing diet. Nutrition and Food Science Promoters of such diets are delighted to aid in this consumer quest, so the number of fad diets continues to increase along with the pro- moters' profits. Fad diets tend to be nutritionally unbalanced, to focus attention on only one type of food or nutrient, to appeal to the consumer with faulty logic, to neglect the issue of weight maintenance, or to make excessive claims for weight loss. The body stores excess energy, measured in kilocalories, as fat. One pound of fat represents 3,600 kilocalories of energy. To lose one pound of fat, you must expend 3,600 kilocalories more than the number in the food you eat. It is not unusual to see claims by a fad diet that you can lose 10 pounds in one week. Take a closer look at this excessive claim: Ten pounds of fat means 36,000 kilocalories. To lose that by dieting in one week, you would have to eat at least 5,000 kilocalories per day less than you normally would. -

“Alternative Nutrition”
“Alternative nutrition” Mgr. Zlata Kapounová, Ph. D., Mgr. Aleksandra Nikolić, Bc. Iuliia Pavlovská, Bc. Petra Ferenčuhová “Alternative nutrition” • General term • Types of diets, that differ from the nutritional habits of the majority of society and conventional recommendations from dietitians. • Usually based on the restriction of certain food groups, most often food of animal origin 2 Why alternative nutrition? • Health reasons – the need for change of lifestyle- obesity, gout, dyslipidemia, zoonosis • Moral and ethical reasons – compassion for animals • Ecological aspect • Economic reasons • Religion • Social factors – peer pressure, fashion,... • Taste preference Types of alternative nutrition • Vegetarianism • Macrobiotic diet • Marginal types: – Divided food diet – Diet by blood group (Adamo’s Diet) – Paleo Diet (Paleolithic diet) – Diet based on pH (alkaline diet) – Detox diet • Organic food Vegetarianism • The most widespread alternative way of eating in Czechia (about 2 % of the population - 200,000 people) • Vegetarian - generally not consuming meat • Types depending on restricted consumption of food of animal origin – semivegetarians (pulo-, pesco-) or flexitarians – lactoovovegetarians – lactovegetarians – vegans – fruitarians – vitarians - RAW fod Vegetarianism • Origin in the Eastern religions of Buddhism and Hinduism • The term dates back to the 19th century • The Vegetarian societies: – The Vegetarian Society (1847 England) – IVU - International Vegetarian Union (1908 Dresden) – EVU - European Vegetarian Union – Czech -

Standard Process 21-Day Purification Program
Standard Process 21-Day Purification Program A Patient Guide to Purifying, Nourishing, and Maintaining a Healthy Body and Weight Clearer . Brighter . Lighter . Your life in high resolution . The Standard Process Purification Program helps your body purify and rebuild itself from the inside out . The program gives you a structured plan for purifying, nourishing, and maintaining a healthy lifestyle . Along with Standard Process supplements, you’ll support your major organ systems with the vitamins, minerals, and other nutrients found in whole foods . In addition, this program supports the maintenance of healthy weight when combined with a healthy lifestyle . When you’ve completed the 21-day purification program, you’ll be amazed at how good you feel . You’ll learn how to transition to a new, healthful way of eating that will continue your journey toward a clearer, brighter, lighter way of life now and in the years ahead .* This plan is not a fad diet . It’s a new way of life, a strategy that you and your health care professional can modify to fit your individual requirements . The plan is a journey of discovery as you try new foods and learn about eating for better health .* Charles C . DuBois President & CEO Why Purification? . 4 Preparing for Purification. 8 Program Basics . 12 Daily Journal . 23 Visit standardprocess.com/purificationprogram for exclusive access to recipes, videos, daily emails, and a Facebook group . Post-Purification . 35 FAQs . 44 *These statements have not been evaluated by the Food and Drug Administration. Recipes . 48 These products are not intended to diagnose, treat, cure, or prevent any disease. -

Which Category Your Diet Belongs To? Statistically, It Is Estimated That Every Year, Americans Spend About $33 Billion on Weight Loss Programs and Products
Which category your diet belongs to? Statistically, it is estimated that every year, Americans spend about $33 billion on weight loss programs and products. Always be aware that if a weight loss program is promising you a magical solution to your weight problems, it is likely that he/she is trying to dupe you. If you are planning on starting a diet, it is best to either consult your doctor or a registered dietitian. They will not only help you a diet plan which meets your requirements, but also one which will be safe. In general, it is best to avoid diets which promises to deliver a quick result or fast weight loss. Be wary if its claims sound too good to be true and always trust your better judgment. You should also avoid diets which recommend that you consume less than 1000 calories per day or eliminate a major food group from your meal. This article discusses the pros and cons of two of the most popular diet plans and how effective or ineffective they actually are. While there are a lot of diet plans available today, the Atkin's and the Zone diet are the two most popular ones. Close behind them are the Pritkins Diet, the Protein Power diet, the South Beach diet, the Specific Carbohydrates diet, the Sugar Busters, and so on and so forth. ATKINS DIET The Atkin's diet is one of the most popular diets in the world today. It is a high-fat, high-protein, and low-carbohydrate plan and the dieter can consume unlimited amounts of cheese, eggs, and meat. -

High-Protein Diets and Weight Loss by Diane Welland, MS, RD
High-Protein Diets and Weight Loss By Diane Welland, MS, RD High-protein diets such as the Zone, Atkins, and Sugar Busters have come and gone for decades, their popularity rising and falling like waves in the ocean. While high-protein diets do usually lead to weight loss, they may be unbalanced meal plans that sometimes restrict entire food groups and fail to meet humans‟ essential needs for vitamins, minerals, and fiber. But that doesn‟t have to be the case. Several studies comparing high-protein, low-carbohydrate diets with high-carbohydrate, low- protein diets found high-protein diets to be just as effective and sometimes even more effective than their high-carbohydrate counterparts when it comes to weight loss. One study, published in March 2009 in The Journal of Nutrition, looked at how a moderately high-protein meal plan measured up to the USDA‟s Food Guide Pyramid diet over a 12-month period.1 Although weight-loss results were similar in both groups, the subjects consuming a high-protein diet lost more body fat and had better blood lipid profiles than the high-carbohydrate dieters, according to the journal article. More recently, a short-term study, published in 2011 in Nutrition Journal, comparing women who were overweight or obese and followed a high-protein diet with those who followed a high- fiber, high-carbohydrate diet showed that although both groups lost weight, the high-protein group lost more weight with greater fat loss and greater decreases in blood pressure.2 These studies are just two in a growing body of scientific evidence suggesting that the right high-protein diet may be a tool worth using in the fight against obesity. -

Lynne Garton Name Plant-Based Eating – Should We Believe the Hype?
The moment for plant‐based eating is Now March 24, 2017 Plant-based Eating – Should we believe the hype? Lynne Garton BSc (Hons) RD Consultant Nutritionist and Registered Dietitian www.alimenta.co.uk @dietlg Why the Renewed Interest? Alpro Foundation 20 years symposium 1 The moment for plant‐based eating is Now March 24, 2017 And in Recent Times… BUT… DAFT DIETS DISSED Food experts declare war on women leading ‘flawed’ clean eating movement amid claims it fuels anorexia Bad fad – Ruby Tandoh on how clean eating turned toxic The backlash against a ‘wellness’ diet is in full swing – and leading chefs and writers associated with it are doing their best to ditch the term. It’s time we called it what it is Clean Eating: The Dirty Truth: 7 myths busted Clean Eating - The Dirty Truth Alpro Foundation 20 years symposium 2 The moment for plant‐based eating is Now March 24, 2017 Spectrum of Plant-Based Eating… Plant-based Semi - vegetarians Pescetarians Lacto-ovo vegetarians Lacto- vegetarians Vegan What is a Plant-Based Diet… FRUITS AND VEGETABLES NUTS AND SEEDS ‘Households across all regions should select predominantly plant-based diets rich in a variety of fruits and vegetables, pulses or legumes, and minimally processed starchy staple foods’… PULSES – INCLUDING SOYA ‘This should not exclude small amounts of animal foods, which make an important nutritional contribution to plant- WHOLEGRAINS food-based diets’ FAO/ WHO (2004) Alpro Foundation 20 years symposium 3 The moment for plant‐based eating is Now March 24, 2017 The Basis of a Healthy Balanced Diet… Vitamins Protein Fats Vitamins Minerals •Sat. -

The Bear’S Words of Wisdom
2 The Bear’s Words of Wisdom Owsley "The Bear" Stanley ii Contents 1 Diet and Exercise 1 2 Low Carber Forum Posts 7 3 Interview with an Alchemist (1998) 285 4 Q&A with igibike on RawPaleoDietForum.com 291 5 The Bear’s Discussion with Rob From ZeroCarbPath 295 5.1 Advice .............................. 296 5.2 Diet ............................... 297 5.3 The basics ............................ 299 5.4 The “Meat is Toxic” Myth ................... 301 5.5 The “Good” Carb Myth ..................... 303 5.6 The “Fiber is Healthy” Myth .................. 303 5.7 On Diet Social Evolution-Acculturation ............ 305 5.8 On Anthropology ........................ 306 5.9 Bear’s Stats ........................... 307 5.10 Bear’s Meat Tips ........................ 308 5.11 Reflections on Long Term Vegetarianism ............ 309 6 The Bear’s Response to Jimmy Moore Wanting an Interview 311 iii iv CONTENTS Chapter 1 Diet and Exercise Source: http://thebear.org/essays1.html#anchor496162 One of the problems of modern living is the way in which we have departed from the things we did as we evolved. Diet is one of those things, and I be- lieve that diet and the lack of the right exercise are the main reasons for the widespead prevalence of obesity, diabetes and heart disease. I have always liked meat the best of all foods, and as a child I never wanted to eat my vegetables, other than the usual starchy things like bread and potatoes. As I grew out of my teens my weight suddenly shot up from 125 pounds to 186 in about six months. I was out on my own and trying to eat on the cheap, which naturally resulted in a rather carbohydrate-rich diet. -

Nutritional Primitivism in Low-Carbohydrate Diet Discourse
1 ‘The food nature intended you to eat’: Nutritional primitivism in low-carbohydrate diet discourse Christine Knight Discipline of English, University of Adelaide November 2007 2 Table of contents Abstract..................................................................................................................................................................3 Thesis declaration.................................................................................................................................................4 Acknowledgements...............................................................................................................................................5 Chapter 1. Low-carbohydrate diets and nutritional primitivism: an introduction............................................8 Primitivism, food studies and low-carbohydrate dieting: a literature review .........................................................................12 Low-carbohydrate diets and health............................................................................................................................20 Thesis outline.......................................................................................................................................................25 Chapter 2. Low-carbohydrate diets in social and scientific context................................................................27 Tracing the recent low-carbohydrate trend ...................................................................................................................28